Assessing psychosocial distress: a pain audit at IRCH-AIIMS
Key messages
Clinical practice within the public health system in the Indian context poses serious challenges to multi-modal total pain management. In light of our audit, we suggest possible procedures to improve pain management in this high-volume scenario, where patients present with multiple forms of distress—economic, psychological, social, spiritual and physical.
Introduction
Cancer pain is severe and excruciating, it deteriorates the quality of life of patients and increases the emotional and psychological burden of family members. At IRCH AIIMS, on an average 50 cancer pain patients visit the four days a week pain OPD. Out of these, about 20 patients have been seen to get inadequate pain relief.
The concept of ‘total pain’—comprised of psychological, social, spiritual and physical factors—has gained prominence within palliative medicine in India and abroad (1-3). Given the new prominence of the ‘total pain’ model and in light of the presence of inadequately treated pain patients at our clinic, we felt a need to assess whether psychosocial components of cancer pain receive the same quality of care as physical pain.
Summary: purpose of audit
- To examine the current procedures of assessing psychosocial pain in the AIIMS pain clinic;
- To analyze data collected through existing assessment procedures;
- To instigate changes in these procedures to bring them up to date with global standards.
Materials and methods
Setting the standards
Clinical audits are now understood as vital components of pain management practice. The on-going UK national-level audit of pain management by the British Pain Society is just one example. Its authors underscore the need for globally recognized standards. For this audit, we identified the NHS (Quality Improvement Scotland) Best Practice Statement for ‘the management of pain in patients with cancer’ as our standard of assessment (4). The primary reason for the selection was the up-to-date quality of its protocols, as well as its careful attention to pain assessment procedures and to the ‘total pain’ model. For our purposes, the following sub-section of the NHS Best Practice Statement is relevant:
Statement 2 (c): pain in patients with cancer is assessed using a formalized, pain assessment tool which measures:
- physical aspects/manifestations of pain;
- Functional effects (interference with activities of daily living);
- Psychosocial factors (level of anxiety, mood, cultural influences, fears, effects on interpersonal relationships, factors affecting pain tolerance);
- Spiritual aspects.
The above statement suggests that Best Practice pain assessment must include physical, functional, psychosocial and spiritual aspects. We further add that these must be completed at a 100% level.
Thus, our standards for this audit can be described as follows:
- 100% of documented pain assessments will include a descriptive of physical, functional, psychosocial and spiritual aspects;
- 100% of the psychosocial components of documented pain assessment will include both functional (interference with daily life and activities) and non-functional factors (i.e. anxiety, mood, depression and so on).
Measuring data completion
Each patient at the AIIMS pain clinic is assessed with a pain assessment form (5). A total of 686 pain assessment forms were analysed. They were processed through the descriptive statistics modules of SPSS.
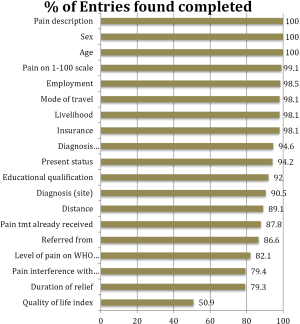
The first step for us was to audit the completion of individual categories within each pain form. We hoped that this would indicate which areas were being comprehensively addressed, and which were less well accounted for within the existing layout of the form. An audit of data completion revealed that basic demographic information and pain assessment measures were recorded at near 100% levels (Figure 1). Other demographic information such as employment, mode of travel, insurance protection and educational qualifications were also well recorded. We find thus that social factors that index economic vulnerability are already being well recorded. However, psychosocial factors (such as ‘pain interference with daily life’ and ‘quality of life’) were less well recorded (both under 80%).
Analysis of data - general demographics of patients
The distribution of the gender of patients was 57.4% male and 42.6% female. Significance tests revealed that women were much less likely to be educated than men. The highest numbers of referrals were from other departments within AIIMS. Medical and radiational oncology contributed the highest number of patients (33.2% and 28.6% respectively). This was followed by a high number of patients who sought treatment directly - 16.6%. Only 2.9% of patients were referred to the clinic from other hospitals; this may be index a wide under-treatment of pain, if understood alongside the paucity of pain clinics in the city in general.
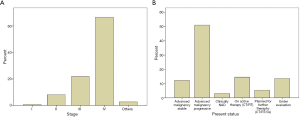
An overwhelmingly large number of patients - 66.7% were stage IV, followed by 21.8% in stage III. Very few patients were in the early stages (I-0.7%, II-8.2%). Amongst all the patients, 48.1% exhibited advanced progressive malignancies (Figure 2).
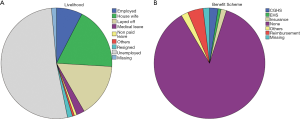
Most patients were either uneducated (36%) or had an education below the 10th Std level (32.5%). More than half the patients were reported themselves to be housewives (18.4%). Equally alarmingly, 88.3% of patients had no insurance of any kind (Figure 3). Patients travelled overwhelmingly by public transport (90.9%), even though the above data reveals most to be presenting at advanced stages of the disease. The median distance that patients travelled was 50 kilometres, confirming that a significant number of patients travel across states for treatment at AIIMS.
A significant finding was that among the 478 patients (69.7%) reporting prior treatment outside the pain clinic, most reported extremely inadequate duration of relief from their present treatment regime. 44.4% reported less that 2 hours of relief, and 34.7% reported less than four hours of relief. While the data is slanted towards those who are presently dissatisfied with their existing treatment, the large number of patients who are inadequately treated for pain should still be understood as a cause of concern.
The socio-demographic data point to a lack of education, presentation in advanced stages, widespread unemployment, lack of medical insurance and the need to travel large distances. We will keep these factors in mind in making suggestions for improving the psychosocial assessment of this specific demographic of patients.
Analysis of data - psychosocial factors
The focus of our audit is on psychosocial variables. We found these to be distributed across the pain assessment form under three different categories.
The first was under the category of ‘symptoms’ - a list that mixed physical and psychosocial categories
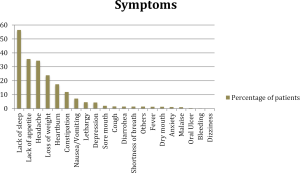
The most often reported symptom was ‘lack of sleep’ (56.5%), followed by ‘lack of appetite’ (35.6%). This was followed by ‘headache’ (34.4%), ‘loss of weight’ (24%) and ‘heartburn’ (17.5%). Significance tests revealed that those reporting ‘lack of sleep’, ‘lack of appetite’ and ‘loss of weight’ as symptoms were strongly associated with high levels of pain on the 0-100 scale and on the WHO ladder. These indicate a consistency in the measures of these functional symptoms.
However, psychiatric symptoms like depression (4.4%) and anxiety (1.2%) were found to be very rarely reported and recorded (Figure 4). These numbers are far lower than other studies in the literature that have focused on the prospective psychiatric assessment of cancer patients. We will discuss this in our following analysis.
The second psychosocial variable was categorized under the question ‘Pain Interference with Daily Life’
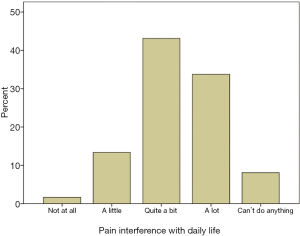
Patients were asked to what extent pain interfered with their daily life. Options were ‘not at all’, ‘a little’, ‘quite a bit’, ‘a lot’ and ‘can’t do anything’ (Figure 5). Most patients reported ‘quite a bit’ (43.1%) followed by ‘a lot’ (33.8%). Significance tests revealed patients reporting a high degree of pain interference with daily life were more likely to report higher level of pain on the 0-100 scale and lower durations of relief from existing treatment. This shows a consistency across the existing assessment data. We note here that this variable is an indicator of functionality in relation to psychosocial wellness.
The final psychosocial variable was found to be the quality of life index
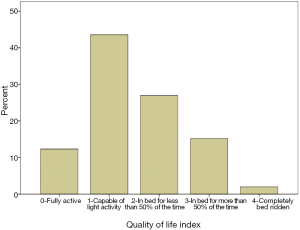
Quality of life data was recorded under options ranging from ‘fully active’, ‘capable of light activity’, ‘in bed for less than 50% of the time’, ‘in bed for more than 50% of the time’ to ‘completely bed-ridden’ (Figure 6).
The largest number of patients reported themselves as capable of light activity (43.6%). Tests revealed significant expected associations of ‘quality of life’ with pain reporting on the 0-100 scales and WHO ladder score, with patient disease stage, and with reported level of pain interference in daily life. This indicates a consistency across these measures of pain assessment.
Discussion
Review against the standards
How do these findings measure up against the standards that we have already set? A look at the pain assessment form (5) as well as our record of the completion of the forms (Figure 1) reveals high rates of completion (90-100%) of most of the physical factors—site, number, intensity, pain description, aetiology and type of pain and history of treatment.
Our focus in this audit however, is on psychosocial factors and we shall now concentrate on this aspect of total pain. The standards we have set require the following:
- 100% records of social, psychological and physical factors of pain;
- 100% records of both functional and non-functional aspects of psychosocial pain.
We have found that existing evaluation of psychosocial factors are distributed under the heading of ‘Symptoms’, ‘Pain Interference in Daily Life’ and a question on the ‘Quality of Life’. Comparison of this layout of the form as well as an analysis of its completion has revealed the following:
(I) Quality improvement Area 1: under—completion of psychosocial categories.
Explanation: while demographic and physical pain categories are efficiently and comprehensively completed, we have found an under-completion of psychosocial categories. ‘Quality of Life Index’ is filled at a rate of 50.9% and ‘Pain Interference with Daily Life’ is filled at a rate of 79.4%.
Quality improvement Area 2: psychosocial categories are dispersed across the form in a way that make them difficult to assess quickly and comprehensively.
Explanation: we have found that categories that pay attention to psychosocial factors are dispersed across social demographic markers, within symptoms that measure both physical and psychosocial factors, and with two questions in different areas of the form that record pain interference with daily life and quality of life. The dispersal across a variety of sites makes it difficult to assess overall psychosocial morbidity in a quick, efficient and comprehensive manner.
(II) Quality improvement Area 2: our standards suggest that functional effects and psychosocial factors be assessed as two different categories. That existing psychosocial categories focus on external functionality rather than psychological distress.
Explanation: both markers of psychosocial distress in our existing form (‘pain interference with daily life’ and ‘quality of life’) focus on patient’s functionality. At least one study in the Indian context has shown that other factors such as peace of mind, happiness with family relations and spiritual tasks are more important that the ability to carry on day-to-day functionality (6). Our chosen standard too suggests that factors such as mood, cultural influences and effects on interpersonal relationships be included. We recognize the need to expand psychosocial assessment from its exclusive focus on functionality to a wider understanding psychosocial distress.
Quality improvement Area 3: that there seems to be an under-reporting of markers of distress and depression in relation to a wider literature on psychological morbidity in the Indian context, as well as in relation to a prior study at this same pain clinic.
Explanation: the incidence of reported psychosocial factors have been seen to be low in this audit~4.3% for depression, and 1.1% for level of anxiety. Other studies in the Indian context have reported much higher incidences of psychiatric morbidity amongst comparable populations of advanced stage cancer patients seeking palliative care. A study at our this very pain clinic in 2005 revealed a high incidence of severe depression 33.3% (7). Another survey of psychiatric morbidity and psychological distress suggests that most studies amongst heterogeneous samples in the Indian context reveal psychiatric morbidity rates that range from 40-80% (8). We take this to indicate a need for a more careful psychosocial assessment at the clinic that is more sensitive to psychosocial distress.
(III) Quality improvement Area 4: analysis of existing data reveals consistent socioeconomic difficulties that need to be systematically accounted for and scored in a psychosocial assessment.
Explanation: this audit has already revealed the severe socioeconomic problems of the patient population at AIIMS. These include lack of education, insurance, employment, means of travel and so on. Further, the data reveals a presentation of disease at a very advanced stage. For a robust psychosocial assessment, the specificity of this feature of patients needs to be accounted for and scored in a more systematic manner.
Instigating change
Having identified key points of improvement, we now review 14 validated and globally used pain assessment protocols in order to assess whether existing procedure might benefit from a comparative review. In the table below, we assess each protocol to see if they can help us with the three areas of quality improvement identified above (Table 1). Instead of reviewing the entire protocol, we concentrate on the sub-sections that assess non-physical aspects of total pain. To summarize, we are looking for a tool that is easy to complete, that can assess specifically psychosocial categories in inadequately relieved patients, and that is attentive to functional as well as non-function related factors, such as mood, depression, anxiety and socio-economic stress.

Full Table
Analysis
About eight of the fourteen tools assessed were well balanced between functional and non-functional symptoms of psychosocial distress, while four were sensitive to socioeconomic distress. In the final analysis, only two tools emerged that fulfilled all the criteria that we had identified as crucial through our audit—the WHO-QOL questionnaire and the Distress Inventory for Cancer-2 (DIC-2). Both tools have been tested and validated through rigorous studies (references).
The DIC-2 recommends itself as the most superior for our purposes for the following reasons. While the WHO-QOL questionnaire has been shown to have validity across a range of chronic conditions, the DIC-2 has been developed specifically with cancer patients in mind. Additionally, the DIC-2 was developed, tested and validated over a period of several years in the Indian context (21,22); its questions reflect a sensitivity to concerns with family life and spirituality that we have found to be prominent in our clinical experience. Further, the DIC-2 identifies multi-dimensional psychosocial distress in cancer patients as a specific form and along a continuum, defined separately and before clinical anxiety and depression. Finally, studies have shown that the use of DIC-2 can significantly predict patient non-compliance to treatment and loss in follow-up (22).
The DIC-2 thus emerges as the most appropriate comprehensive tool for our clinical practice. The reasons for this are as follows:
- Specificity of this tool for cancer patients;
- Sensitivity to multidimensional distress—social, economic, spiritual and psychological;
- Ease of administration;
- Development and rigorous validation in the Indian context;
- Identification of early distress to help compliance to treatment and avoid loss in follow-up.
However, given the volume of our clinical practice, we do not think it feasible to administer the DIC-2 to every patient, especially in the outpatient setting where we treat over 50 patients on a daily basis. For this purpose, the American Pain Society Patient Outcome Questionnaire appears to be the easiest and balanced tool for a quick, initial psychosocial assessment. Its short, simple format and its balance of total pain factors make it the best choice for a first-line assessment of outpatients.
Recommendations
Recommendation 1
We suggest that DIC-2 be incorporated into the pain management protocol at AIIMS. Given the high-volume of patients, we suggest that this tool be administered to the subgroup of inadequately relieved patients, whose pain has proved recalcitrant to first line therapy. High distress scores could provide the basis for in-house counseling, or if required, referrals to psychiatrists and home-care services.
Recommendation 2
We suggest that the American Pain Society Patient Outcome Questionnaire be incorporated into the general pain assessment form. It is a short and balanced tool that can provide initial information about both functional and non-functional psychosocial distress in a quick and easy manner.
It is hoped that this two-tiered model will bring our assessment procedures up to the standard we set ourselves while conducting our audit, while at the same time keeping in mind the exigencies of our high-volume clinical practice.
Conclusions
Our audit exercise reveals important concerns about psychosocial assessment in our pain clinic. These included incomplete completion of psychosocial components of pain, a bias towards functional factors of psychosocial distress, an under-reporting of non-functional distress and an inadequate assessment of economic distress and its impact upon psychosocial wellbeing. Important barriers we perceived to better completion were the high-volume of an urgently distressed patient population and an inadequately conceptualized assessment tool.
After comparing 14 existing validated tools we recommended a new assessment procedure that would consist of a two-tiered approach—one for a quick initial survey of every patient and another for a more comprehensive assessment of patients inadequately relieved by physical management.
Clinical practice within the public health system in the Indian context poses serious challenges to multi-modal total pain management. In light of our audit, we suggest possible procedures to improve pain management in this high-volume scenario, where patients present with multiple forms of distress—economic, psychological, social, spiritual and physical. We look forward to similar studies that might produce innovative solutions in enhancing total pain management within the context of the specific exigencies of high-volume quality pain care in the developing world. We must ensure that acutely distressing psychosocial symptoms do not remain invisible, and receive the same degree of quality attention as physical pain.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Otis-Green S, Sherman R, Perez M, et al. An integrated psychosocial-spiritual model for cancer pain management. Cancer Pract 2002;2:S58-65. [PubMed]
- Saunders CM. eds. The management of terminal disease. Hodder Arnold, 1978.
- Zaza C, Baine N.. Cancer pain and psychosocial factors: a critical review of the literature. J Pain Symptom Manage 2002;2:526-42. [PubMed]
- NHS-QIS. Best Practice Statement: Management of Pain in Cancer Patients. Scotland, 2009.
- Chaturvedi SK. What’s important for quality of life to Indians--in relation to cancer. Soc Sci Med 1991;2:91-4. [PubMed]
- Pahwa M, Babu N, Bhatnagar S.. Fighting cancer is half the battle... living life is the other half. J Cancer Res Ther 2005;1:98-102. [PubMed]
- Mehrotra S.. Psycho-oncology research in India: Current status and future directions. J Indian Acad Appl Psychol 2008;2:7-18.
- Pasero C, McCaffery M. Pain assessment and pharmacologic management. Recherche 2010;67:02.
- Cleeland CS. The Brief Pain Inventory (Long form). Pain Research Group, 1991.
- Otis-Green S, Kuebler K, Davis M, et al. Psychosocial pain assessment form. Palliative practices: An interdisciplinary approach 2005:462-7.
- Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;2:365-76. [PubMed]
- Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 1993;2:570-9. [PubMed]
- Cleeland CS, Mendoza TR, Wang XS, et al. Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 2000;2:1634-46. [PubMed]
- de Haes JC, van Knippenberg FC, Neijt JP. Measuring psychological and physical distress in cancer patients: structure and application of the Rotterdam Symptom Checklist. Br J Cancer 1990;2:1034-8. [PubMed]
- Rogers SN, Gwanne S, Lowe D, et al. The addition of mood and anxiety domains to the University of Washington quality of life scale. Head Neck 2002;2:521-9. [PubMed]
- Psychiatric Research Unit W.C.C.i.M.H. WHO (Five) Well-Being Index. Frederiksborg General Hospital, Hillerød, 1998.
- Skevington SM, Lotfy M, O’Connell KA, et al. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 2004;2:299-310. [PubMed]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;2:361-70. [PubMed]
- Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Archives of General Psychiatry 1961;1:561-71. [PubMed]
- Gordon DB, Polomano RC, Pellino TA, et al. Revised American Pain Society Patient Outcome Questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain 2010;2:1172-86. [PubMed]
- Thomas BC, Mohan VN, Thomas I, et al. Development of a distress inventory for cancer: preliminary results. J Postgrad Med 2002;2:16-20. [PubMed]
- Thomas BC, Thomas I, Nandamohan V, et al. Screening for distress can predict loss of follow-up and treatment in cancer patients: results of development and validation of the Distress Inventory for Cancer Version 2. Psychooncology 2009;2:524-33. [PubMed]