Sexual healthcare for cancer patients receiving palliative care: a narrative review
Introduction
The aim of palliative care is to provide a holistic approach, which encompasses all aspects of a person’s wellbeing including physical, psychosocial, emotional and spiritual. For many patients, maintaining their sexual health is an important aspect of their quality of life (QoL); communication and participation in sexual activities can provide a sense of normalcy and offer couples mutual enjoyment and foster a sense of closeness (1,2). Although expressions of sexuality may be impacted by changes to physical capability, physical expression can be replaced by validation of the emotional connection between patients and their partners (1). Healthcare providers (HCPs) should recognize that many patients in the terminal phase of their illness continue to value intimate relationships, thus emphasize the need to incorporate standardized sexual health assessments and discussions as a part of the palliative care services that are provided to patients.
One study demonstrated that many terminally ill patients value their sexuality and want the opportunity to discuss impact of treatment (3). However, HCPs often take a strict medical approach to diagnosis and treatment, and fail to anticipate changes to patients’ sexuality (4). Some institutions have adopted systematic frameworks for the delivery of sexual health services using models such as the Skilled Steps, PLISSIT (Permission, Limited Information, Specific Suggestion and Intensive Therapy), Kubler-Ross Theory, BETTER (Bring up the topic, Explaining, Telling patients about resources, Timing of sexual health services, Education on specific topics and Recording the interactions), 5As-Ask, Advise, Assess, Assist, Arrange, and ALARM (Activity, Libido, Arousal, Resolution and Medical Information) models, which provide HCPs with strategies for approaching sexual health care (1,5-8). Research demonstrates, however, that palliative patients are rarely referred to specialists such as sex therapists for further support if needed (9,10).
Furthermore, it is reported that HCPs rarely conduct sexual health assessments due to barriers including inadequate clinical training and intimacy assessment skills, lack of acknowledgement of the importance of sexual health, or personal discomfort with the topic itself (11). This is more evident with adolescent or elderly patients, as they are commonly perceived as groups that are not sexually active (12). When sexual health assessments are carried out, they often focus on physical function, documenting symptoms of sexual dysfunction and loss of libido as a result of cancer treatment, but fail to address the psychological or sociological aspects of intimacy and sex (13). If patients receive sexual health information in a proactive manner as part of the consent process, so that they understand the impact of treatments, they may avoid unnecessary issues and be aware of strategies to maintain a healthy and enjoyable intimate relationship throughout their cancer journey (14).
This review was conducted to explore the prevalence and importance of including sexual healthcare in the palliative setting as a component of the holistic care provided to cancer patients, to identify current interventions that are implemented to address sexual health issues and identify the barriers that patients and HCPs may encounter which may prevent sexual health discussions.
Methods
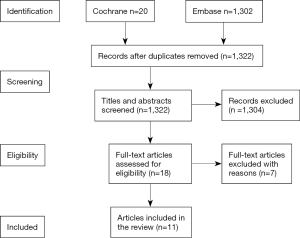
A literature search was conducted on Medline and Embase databases (from inception to July 19, 2016). Our search strategy included both MeSH and free text keyword searches: “cancer”, “sexual health”, “sexual wellbeing”, “sexual functioning”, “sexual behaviour”, “sexual dysfunction”, “intimacy”, “intimate relationship”, “palliative care”, “hospice care”, “terminal care”, “sexual partners”, and “sexuality”. Results were limited to studies conducted in humans and the English language. The search generated a total of 1,322 results that were independently screened by two authors (K Ariello, K Wang) first by title, then abstract, and subsequently full text using eligibility and ineligibility criteria. Figure 1 provides an overview of the screening process. If a disagreement arose on whether an article should be included, discussion ensued until a consensus could be reached. If a consensus was not reached a third author (M Choi) was consulted.
Screening criteria
Eligibility and ineligibility criteria were generated for the present review by five authors (K Ariello, K Wang, M Choi, L Rowbottom, R Macdonald) to select articles for inclusion. Articles were included if they discussed sexual health/functioning/behavior/dysfunction or intimacy and relationships for patients in terminal/hospice/palliative care settings. Only original articles were included in this review; case reports, case series and review articles were excluded. The reference section of each review article identified was screened for potentially eligible studies.
Data extraction
Information about study cohort characteristics, main findings, and conclusions, were independently extracted from full text articles by two authors (K Ariello, K Wang). Data extracted was subsequently compared to ensure accuracy.
Results
A total of 1,322 articles were identified after the conducted search, including 1,302 articles from Embase and 20 from Cochrane. Eleven of these articles met the inclusion criteria and were included in the present review, summarized in Table 1.

Full table
Prevalence and impact of sexual health assessments
Six of the 11 articles that were included in this review indicated either an absence or low frequency of sexuality discussions between HCPs and patients in palliative settings. Research conducted by de Vocht et al., which interviewed patients with a wide range of cancer diagnoses and partners of patients, reported that most HCPs did not address sexuality and intimacy issues (5). Similar results were observed in medical consultations between adolescent patients and HCPs, where none of the 25 patients had their sexual history taken despite multiple visits (15). Although uncommon, sexuality discussions did occur as reported by HCPs and patients in the remaining four articles. It is interesting to note that in the case study conducted by Krychman et al. the brain cancer patient initiated sexuality discussions with her HCP (16). Whereas in other studies, results indicated that often when these discussions occur they are initiated by HCPs and not by patients.
Nine of the ten articles reported on the impact of sexual health assessments, emphasizing the importance of including sexuality discussions in the palliative care setting. In general, patients and HCPs reported positive outcomes when assessments/discussions occurred and negative implications in its absence. Researchers found numerous psychosocial benefits of these discussions, as HCPs were able to offer validation, emotional support and reassurance to patients and intimate partners (1,6,10,16,17). Furthermore, these discussions allowed trained HCPs to suggest alternative methods of expressing sexuality for patients who suffered from physical sexual dysfunctions and to patients for changes in their sexuality that could take place during treatment (17). Most importantly, patients reported that sexual health continued to be an important aspect in their QoL despite changes in the frequency and activity of physical expression (17,18). Although a small population, adolescent patients should not be overlooked; without dedicated sexual assessments, opportunities to educate patients on sexually transmitted diseases, pregnancies and high-risk sexual behaviour would be scarce (15).
Interventions and suggestions
Ten of the 11 articles discussed suggestions or current interventions to increase the occurrence of sexual health assessments. In the majority of these studies, patients suggested some form of improvement by their HCPs or their practice, the most common of which were: HCPs should be further educated and trained in sexual health care, HCPs should take initiative and give patients the opportunity to discuss sexuality concerns, and psychosexual support should be a standard a part of patient treatment (1,3,5,17). Thirty oncology HCPs also suggested that further training, specialized education, and implementation of a standard routine in sexual health care may be key in addressing this issue (10).
Three studies suggested specific models or guides for HCPs to follow when approaching the topic of sexuality with patients. The ‘Stepped Skills’ model describes a team approach to addressing sexuality, where different members of the care team are ascribed complementary roles that ensure different strengths are used to provide optimal sexual health care, i.e., instead of one HCP addressing sexuality and palliative issues, multiple HCPs work as a team to provide support on different issues (5). The PLISSIT model could provide structured framework for sexual health care in palliative settings; HCPs can use the model to guide sexuality discussions with patients (1). Lastly, the Kubler-Ross theoretical model of the stages of death can provide a better understanding of the difficulties patients and partners face at end-of-life; however, it should be noted that this model has been criticized for its lack of empirical validation and its strict vision of the process of death (6).
Barriers limiting the frequency of sexual health assessments
Results from 8 of the 11 articles discussed potential barriers that HCPs and patients encounter which may limit sexual health discussions in palliative settings. Most of these studies addressed factors that prevent HCPs from providing sexual health care. Some HCPs have reported physical limitations such as lack of time, whereas others have indicated psychosocial issues such as personal discomfort, inadequate training and prioritizing treatment of disease over addressing sexual health (5,10). Inadequate education in sexual health care may be the reason why HCPs have difficulty accepting that adolescents with life-limiting conditions would still value their sexuality, and may also account for their reluctance to discuss sexual health when asked by patients (3,15). Patients most likely encounter emotional barriers that keep them from initiating sexuality discussions with HCPs such as feelings of shyness, and patients may also be waiting for HCPs to initiate discussions (1,6,17).
Discussion
Sexuality in palliative settings
This review presents results that provide further evidence demonstrating a low prevalence of sexual health assessments in palliative care, explores emotional and physical barriers that HCPs and patients encounter and discusses established as well as less well-known interventions that can potentially address this issue.
Sexuality is a fundamental aspect of life; for many people, physical intimacy and the desire for sexual expression do not stop because of disease or treatment (1). Despite this, the few primary research studies that were available and included in our review indicated that sexuality discussions occur rarely or not at all in the palliative settings (3,5,10,15,17). It is interesting to note that HCPs have expressed that if patients had concerns in sexuality they would initiate these discussions, whereas most patients reported that despite waiting for the opportunity to discuss these issues, their HCPs never approached this topic (17). Research should further explore psychological factors that cause patients to feel discomfort in discussing sexuality with their HCPs, who should be trustworthy and understanding figures. In addition, it may be helpful to explore any significant differences across cultures in patients and HCPs related to the discussion of sexual health care.
The positive impact of providing sexual health care in palliative settings should outweigh any negative aspects that are associated with this issue. HCPs should focus on potential improvements in providing sexual health care instead of personal barriers limiting their ability to do so, as palliative patients continue to value intimacy and expression of sexuality as an important aspect in QoL; a holistic approach also means holistic assessments encompassing all aspects of patient care (18). Furthermore, sexual health care as a part of treatment can positively impact patients and intimate partners; HCPs can use this opportunity to provide expert advice for physical dysfunctions and symptoms associated with disease and also to provide psychosocial support through validation, reassurance and education (1,10,17). The results we have presented on the lack of sexual health assessments and their importance to palliative patients are in accordance with more than 25 years’ worth of research, yet sexual health care is still an issue that is commonly overlooked by palliative HCPs (19). More recently, Leung et al. also reported on the limited attention focused on sexual health in palliative care (8).
Majority of the barriers that were reported by patients and HCPs specifically indicated or implied that HCPs require more formalized training and education in sexual health care to increase HCPs’ comfort and ability to provide sexual health support (10,16). A study that investigated the outcomes of a 2-year educational intervention reported that post training workshops, the frequency of sexuality discussions were significantly higher among workshop attendants (31%) than non-attendants (11%); which indicates formal education as a potential and viable intervention (20). However, another major barrier that HCPs encounter includes a strict medicalized approach, focusing on diagnosis and treatment of disease, which physically limits time that can be spent providing psychosocial support (10). Patients often are too embarrassed or shy to raise concerns with their HCPs and often wait for HCPs to initiate these discussions (1,17). Interestingly, Hawkins et al. reported that when concerns were raise regarding sexuality with patients’ HCPs, the majority of HCPs did not provide medical advice and often dismissed patients, claiming that they do not need to discuss or focus on sexuality issues (3). This finding once again affirms the need for more formalized training and education, and may also imply an even greater gap in HCP education than was previously emphasized in other studies and reviews. This result is not completely new, as patients and HCPs have previously indicated that HCPs may have personal assumptions and stereotypes (21). However, it may potentially be another issue to improve upon, as HCPs in palliative care especially should be working towards addressing issues related to patient QoL.
In addition to formalized education or training and standardizing sexual health care in palliative settings, there are a variety of ways for HCPs to approach sexuality in patients. Results explored three specific models and guides that HCPs may use and reference in their practice to initiate sexuality discussions: a Stepped Skills model, the PLISSIT model and the Kubler-Ross theoretical model of the stages of death (1,5,6). However, only a few results have indicated the use of these models in patient care. Some institutions have adopted similar systematic frameworks to the PLISSIT model, also used for the delivery of sexual health services such as the BETTER, 5As and ALARM models (7,8). In addition to incorporating systematic framework, Leung et al. suggests two components that HCPs should follow when approaching sexuality in patients: (I) use of open-ended questions and a curious approach to give patients the opportunity to express themselves and (II) to attend constantly to details (8). There are a variety of delivery models and information on sexual health care that HCPs can reference; HCPs should explore and find what works best to accommodate their specific palliative patient population. Finally, perhaps a simple question asking how patients feel about discussing sexuality can welcome an open discussion that may become a small step forward in addressing the issue of sexual health care in palliative settings.
Limitations
With the exception of research conducted by Hawkins et al., majority of the data collected from primary research articles and presented in this review were drawn from studies with small sample sizes and often with patients from the same institution (3). Furthermore, interviews with patients and HCPs often required a retrospective recall of previous consultations or interactions. Future research with larger sample sizes that compare data from various institutions with oncology/palliative care populations may present a more comprehensive view on this topic. This review also emphasized barriers that patients and HCPs reported which prevent HCPs from initiating these discussions. However, further exploration on the emotional barriers that patients encounter may also shed light on new tools that can help patients be the first to raise concerns in these discussions.
Conclusions
A review of previous literature indicated poor understanding of patient concerns regarding sexual health and intimacy leading to minimal incorporation of sexual health care in palliative settings. Maintaining sexuality and sexual intimacy has many positive implications for both the physical and psychosocial wellbeing of patients. Formalized education and skills training can raise awareness in HCPs and provide them with the tools to better understand and approach sexuality in patients. In addition, there are a variety of systematic framework that can be implemented to guide HCPs in delivering sexual health care such as, Stepped Skills, PLISSIT, Kubler-Ross theoretical stages of death, BETTER, 5As and ALARM. Future studies may want to explore if there are any differences in approach to sexuality across cultures, the effectiveness of implementing systematic framework and other barriers that limit patient ability to raise concerns with HCPs. A better understanding and approach to sexual health care by HCPs may be the first step in creating a truly holistic assessment in palliative care.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Taylor B. Experiences of sexuality and intimacy in terminal illness: a phenomenological study. Palliat Med 2014;28:438-47. [Crossref] [PubMed]
- Redelman MJ. Is there a place for sexuality in the holistic care of patients in the palliative care phase of life? Am J Hosp Palliat Care 2008;25:366-71. [Crossref] [PubMed]
- Hawkins Y, Ussher J, Gilbert E, et al. Changes in sexuality and intimacy after the diagnosis and treatment of cancer: the experience of partners in a sexual relationship with a person with cancer. Cancer Nurs 2009;32:271-80. [Crossref] [PubMed]
- Mercadante S, Vitrano V, Catania V. Sexual issues in early and late stage cancer: A review. Support Care Cancer 2010;18:659-65. [Crossref] [PubMed]
- de Vocht H, Hordern A, Notter J, et al. Stepped skills: A team approach towards communication about sexuality and intimacy in cancer and palliative care. Australas Med J 2011;4:610-9. [Crossref] [PubMed]
- Rothenberg MI, Dupras A. Sexuality of individuals in the end-of-life stage. Sexologies 2010;19:147-52. [Crossref]
- Mick JA, Hughes M, Cohen MZ. Using the BETTER Model to assess sexuality. Clin J Oncol Nurs 2004;8:84-6. [Crossref] [PubMed]
- Leung MW, Goldfarb S, Dizon DS. Communication About Sexuality in Advanced Illness Aligns With a Palliative Care Approach to Patient-Centered Care. Curr Oncol Rep 2016;18:11. [Crossref] [PubMed]
- Stausmire JM. Sexuality at the end of life. Am J Hosp Palliat Care 2004;21:33-9. [Crossref] [PubMed]
- Vermeer WM, Bakker RM, Stiggelbout AM, et al. Psychosexual support for gynecological cancer survivors: current practices and need for assistance. Support Care Cancer 2015;23:831-9. [Crossref] [PubMed]
- Cort E, Monroe B, Oliviere D. Couples in palliative care. Sex Relatsh Ther 2004;19:337-54. [Crossref]
- Marks A, Murphy T, Bower K. Adolescent sexuality at the end of life: Practical approaches to a difficult problem. J Pain Symptom Manage 2014;47:390-1. [Crossref]
- Kelemen A, Groninger J, Cagle J, et al. Bringing sexy back: sexuality and intimacy concerns in an advanced heart failure population receiving palliative care consultation. J Hear Lung Transplant 2016;35:S19-20. [Crossref]
- Gianotten WL. Sexuality in the palliative-terminal phase of cancer. Sexologies 2007;16:299-303. [Crossref]
- Sargant NN, Smallwood N, Finlay F. Sexual History Taking: A Dying Skill? J Palliat Med 2014;17:829-31. [Crossref] [PubMed]
- Krychman ML, Amsterdam A, Carter J, et al. Brain cancer and sexual health: a case report. Palliat Support Care 2004;2:315-8. [Crossref] [PubMed]
- Lemieux L, Kaiser S, Pereira J, et al. Sexuality in palliative care: patient perspectives. Palliat Med 2004;18:630-7. [Crossref] [PubMed]
- Ananth H, Jones L, King M, et al. The Impact of Cancer on Sexual Function: a controlled study. Palliat Med 2003;17:202-5. [Crossref] [PubMed]
- Blagbrough J. Importance of sexual needs assessment in palliative care. Nurs Stand 2010;24:35-9. [Crossref] [PubMed]
- Jonsdottir JI, Zoëga S, Saevarsdottir T, et al. Changes in attitudes, practices and barriers among oncology health care professionals regarding sexual health care: Outcomes from a 2-year educational intervention at a University Hospital. Eur J Oncol Nurs 2016;21:24-30. [Crossref] [PubMed]
- Sawin EM. The Body Gives Way, Things Happen: Older women describe breast cancer with a non-supportive intimate partner. Eur J Oncol Nurs 2012;16:64-70. [Crossref] [PubMed]