Patient preference for stereotactic radiosurgery plus or minus whole brain radiotherapy for the treatment of brain metastases
Introduction
Brain metastases are a cause of significant morbidity and 20–40% of patients with metastatic cancer will develop disease to their brain during their illness (1). As imaging modalities improve, the incidence of brain metastases also rises (2). Patients can present with neurocognitive and neurological symptoms of varying severity that can interfere with quality of life, however uniformly, prognosis is poor with median survival measuring between 2 and 3 months without treatment.
In general, radiotherapy techniques for treatment of patients with brain metastases include whole brain radiotherapy (WBRT) and stereotactic radiosurgery (SRS) for a selected population. Increased screening and improved imaging techniques have led to not only an increased incidence of brain metastases, but identification of patients with limited brain metastases which may be more amenable to the latter.
The addition of SRS to WBRT was found to improve local control and possibly improve overall survival in patients with single brain metastasis (3-5). In an attempt to spare the neurocognitive sequelae of WBRT, a number of trials have compared SRS plus WBRT to SRS alone.
In a randomized control trial where 132 patients with 1–4 brain metastases received either SRS alone or SRS plus WBRT, combination therapy resulted in better local control and a lower incidence of development of new brain metastases, but no difference in overall survival (3). Two further studies compared functional outcomes. Patients who received SRS plus WBRT had greater neurocognitive decline at 4 months compared to those that received SRS alone (5). Kocher et al. found that addition of WBRT did not improve duration of functional independence and survival (4). In both studies, the addition of WBRT reduced the probability of recurrence at the initially treated sites and development of new brain metastases. Adverse events in all three trials were similar (6).
Given similarities in survival between both treatments but differences in neurocognition and risk of development of new metastases, patient values are an important component in treatment decision making. To date, no studies have assessed patient preferences in this setting. The goal of this study was to determine to proportion of patients who wish to partake in treatment decisions and their important considerations when making such decisions.
Methods
Between 2012 and 2014, patients seen in consultation for radiosurgery for brain metastases were screened at two regional cancer centers in North America (Odette Cancer Centre at Sunnybrook Health Science Centre, Toronto, Canada and University Hospitals Seidman Cancer Center, Cleveland, Ohio). This study was approved at the Institutional Research Ethics Board at both sites of patient recruitment.
Patients were included if they were older than 18 years of age, had the ability to provide consent, had a maximum of four brain metastases on MRI, had no previous brain treatment, were RPA class 1 or 2 [Karnofsky Performance Status (KPS) >70], and if treating physicians believed both treatments were appropriate and were able to maintain equipoise. Patients were excluded if they refused treatment, had undergone prior surgery or radiotherapy for brain metastases, had leptomeningeal disease or had primary malignancy of small cell lung cancer, lymphoma, germ cell tumors, leukemia or unknown primary.
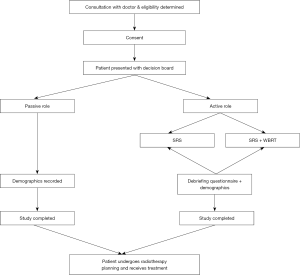
Patients consenting to this study were asked to participate in the decision-making process for treatment and specifically whether they wished to play an active role or passive role (Figure 1). Those electing for a passive role received treatment at the discretion of the treating physician. Patients who wished to have an active role in treatment decision making were presented with a decision board (Figure S1) outlining major outcomes extracted from the three aforementioned studies. They then had the opportunity to discuss all necessary questions relating to each regimen with the treating radiation oncologist.
After deciding treatment, a debriefing questionnaire was completed (Figure S2). These questions evaluated outcomes from clinical trials and practical considerations thought to be pertinent to the patient when making a decision. An open-ended question was offered for patients to list considerations not listed. Each item was ranked on a scale of zero (not at all important to consider) to 10 (extremely important to consider). Descriptive statistics summarized findings.
Results
A total of 23 patients were included for analysis (Table 1). The majority of patients were male (15/23; 65.2%) and all patients were Caucasian (23/23; 100%). The average age of included patients was 65.5 years (±10.7 SD). Most patients had high school education (13/23; 56.5%) followed by college/graduate education (9/23; 39.1%). The most common primary cancer was non-small cell lung cancer (15/23; 65.2%) followed by melanoma (3/23; 13.0%) and renal cell carcinoma (3/23; 13.0%). Median KPS was 90.
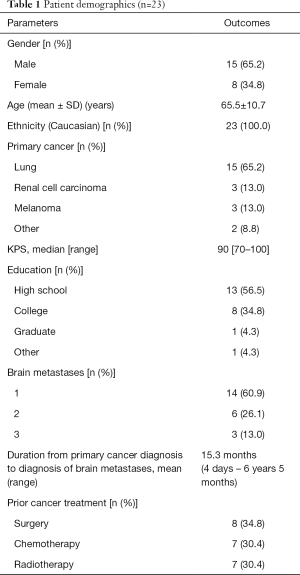
Full table
Most patients were referred for treatment of single brain metastasis (14/23; 60.9%) while six patients had two metastases (26.1%) and three patients had three brain metastases (13.0%). On average, patients were diagnosed with brain metastases 15.3 months after primary cancer diagnosis, however one patient was seen in consultation 3 days after primary cancer diagnosis. A total of 8 (34.8%), 7 (30.4%) and 7 (30.4%) patients had previous cancer related surgery, chemotherapy and radiotherapy.
All patients wished to take an active role in decision making. The majority of patients (91.3%; 21/23) elected for SRS alone and two patients decided to receive SRS plus WBRT (8.7%; 2/23). In patients who had prior radiotherapy, all patients (100%; 7/7) elected for SRS alone and in those receiving radiotherapy for the first time, the majority (87.5%; 14/16) wanted only SRS.
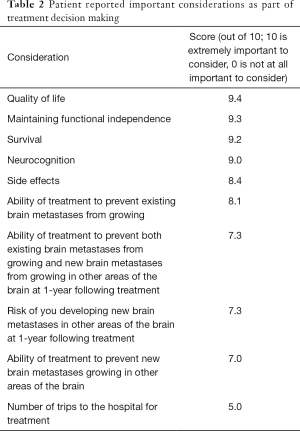
All factors were found to be important as part of patients’ decision making (at least 5/10). The most important factors influencing treatment decisions are described in Table 2. Quality of life (9.4/10), maintaining functional independence (9.3/10) and influence of treatment on survival (9.2/10) were most important factors. Multiple trips to the hospital (5.0/10) and preventing new brain metastases from growing (7.0/10) were seen as least important. In open ended responses, other factors identified as being important included ability to start chemotherapy sooner (n=2), seeking expert advice from relatives (n=2), hair loss (n=1) and time and travel (n=1).
Full table
Discussion
Patient values play an important role in treatment decision making especially if mortality are similar. This is the first study to our knowledge to assess patient preferences for radiotherapy technique in the treatment of brain metastases. All patients in our study wished to play an active role in treatment decision making. Most prefer SRS alone and value quality of life, functional independence and survival as the most important factors when arriving at their treatment preference.
In an era of patient centered care, treatment success is measured by both disease outcome and patient satisfaction which is founded by two-way communication and informed decision making. The extent to which patients wish to participate in decision making should be explored early. Previous studies have found poorer quality of life in patients who report discordance between actual and preferred roles as part of the cancer treatment decision making process. Atherton et al. found that in both patients who preferred an active role in decision making, but felt that they played a passive role, and vice versa, self-reported physical health and mood were worse compared to those who played the role they preferred (7).
The proportion of patients wishing to play an active role in decision making has varied. In a large meta-analysis involving over 3,000 patients, approximately 25% of patients wished to play an active role in treatment decision making, 25% had physicians make decisions for them and 50% preferred a collaborative role (8). With medical literature more available and greater self-advocacy, the number of patients wishing to partake in decision making may be increasing. In 1996, 52% of newly diagnosed breast cancer patients preferred a passive role in treatment decision (9) making whereas in a similar setting in 2006, only 22% of patients wished to defer all decisions to the treating physician (10). Interestingly, patients with advanced stage disease tended to prefer more passive approaches (11,12) where in our sample of patients with metastatic brain disease, all patients wished to play an active role.
Nearly all of our patients elected for SRS without the addition of whole-brain radiotherapy citing quality of life and functional independence as most important factors influencing their decision. These factors may reflect the perceived relationship between neurocognitive decline and functional independence, which was more important to our sample than recurrence or development of new metastatic disease. Our findings are similar to prior studies that have explored patient values as part of treatment decision making. Especially in older individuals, quality of life is consistently reported as a top priority when deciding between treatment choice (13). In other studies, patients have expressed hesitation in treatments associated with functional and/or cognitive impairment (14). Though still important to patients, our sample responded that prevention of development of new metastatic brain lesions were least important in treatment decision making but prioritized quality of life and functional independence.
Interestingly, the two patients who preferred SRS + WBRT did not have prior radiotherapy treatments and all patients who previously had radiotherapy preferred SRS alone. Further statistical analysis is limited by sample size, however, we wonder about the impact of prior patient experiences with similar treatments and how this influences decision making. A second surprising finding was that survival was scored as the third highest factor influencing treatment decision making despite the decision board (and prior prospective trials) presenting that survival was no different between treatment groups. We wonder if patients judged the equivalence of survival as being important, thereby allowing them to select treatment based on other factors, whereas if a survival difference did exist, these other factors may not be as highly considered. Or perhaps survival was seen to encompass not only the duration of time of life remaining, but also the quality of life during that period (in this case, possible worsening neurocognitive function). We encourage future studies to further explore patient reasoning in their decision making.
We are limited by sample size and our cohort (mostly lung cancer) is not representative of all patients with brain metastases. Patient values and preferences may differ based on issues unique to primary cancers. Further, a number of patients in our sample received prior chemotherapy, radiation therapy and/or surgery and we are unable to characterize how this influenced our findings, and in particular, how delivery of prior treatment information may affect current decision making. Though our sample was not sufficient to characterize the impact of socioeconomic factors on preferences, previously studies have shown that these do not significantly influence whether patients wish to take an active or passive decision making role (15). Prior studies have also identified preferences in desired role as part of treatment decision making that vary based on ethnic background (16). Unfortunately, our convenience sample only included those of Caucasian ethnicity and we urge future studies to compare preferences among more diverse samples.
Patients receiving radiotherapy for brain metastases wish to participate in their treatment decision making when presented with a simple, and easy to understand decision board. Nearly all patients elected for therapy that would spare neurocognitive decline. Functional independence, quality of life and survival were seen as the most important considerations when deciding on treatment. Our methodology can be applied to other settings in oncology and have previously been shown to improve patient satisfaction and quality of life. Especially in areas where treatment is not clearly defined, patient input and an understanding of patient values is important to delivering most appropriate care.
Acknowledgements
The authors thank Dr. Mitchell Machtay for providing the support for the portion of the study performed at University Hospitals Seidman Cancer Center (UHSCC). The portion of the study performed at University Hospitals Seidman Cancer Center (UHSCC) was funded by the Department of Radiation Oncology at UHSCC.
Footnote
Conflicts of Interest: SS Lo was a member of an oligometastasis research consortium funded through a grant from Elekta AB, and has received travel expenses for past educational seminars from Accuray. Dr. Sahgal reports receiving research grants from Elekta AB and honoraria for past educational seminars from Elekta AB, Medtronic, and Varian Medical Systems. The other authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Institutional Research Ethics Boards at the Odette Cancer Centre (NO. 268-2012) and University Hospitals (NO. 00008600) written informed consent was obtained from all patients.
References
- Loeffler JS, Patchell RA, Sawaya R. Treatment of metastatic cancer. In: DeVita VT Jr, Hellman S, Rosenberg SA, et al. editors. Cancer: Principles and Practice of Oncology. 5th ed. Philadelphia: Lippincott–Raven Publishers; 1997:2523.
- Eichler AF, Loeffler JS. Multidisciplinary management of brain metastases. Oncologist 2007;12:884-98. [Crossref] [PubMed]
- Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 2006;295:2483-91. [Crossref] [PubMed]
- Kocher M, Treuer H, Voges J, et al. Computer simulation of cytotoxic and vascular effects of radiosurgery in solid and necrotic brain metastases. Radiother Oncol 2000;54:149-56. [Crossref] [PubMed]
- Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 2009;10:1037-44. [Crossref] [PubMed]
- Tsao M, Xu W, Sahgal A. A meta-analysis evaluating stereotactic radiosurgery, whole-brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer 2012;118:2486-93. [Crossref] [PubMed]
- Atherton PJ, Smith T, Singh JA, et al. The relation between cancer patient treatment decision-making roles and quality of life. Cancer 2013;119:2342-9. [Crossref] [PubMed]
- Singh JA, Sloan JA, Atherton PJ, et al. Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the Control Preferences Scale. Am J Manag Care 2010;16:688-96. [PubMed]
- Beaver K, Luker KA, Owens RG, et al. Treatment decision making in women newly diagnosed with breast cancer. Cancer Nurs 1996;19:8-19. [Crossref] [PubMed]
- Hack TF, Degner LF, Watson P, et al. Do patients benefit from participating in medical decision making? Longitudinal follow-up of women with breast cancer. Psychooncology 2006;15:9-19. [Crossref] [PubMed]
- Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer. JAMA 1997;277:1485-92. [Crossref] [PubMed]
- Beaver K, Booth K. Information needs and decision-making preferences: comparing findings for gynaecological, breast and colorectal cancer. Eur J Oncol Nurs 2007;11:409-16. [Crossref] [PubMed]
- Martin VC, Roberto KA. Assessing the stability of values and health care preferences of older adults: A long-term comparison. J Gerontol Nurs 2006;32:23-31. [PubMed]
- Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med 2002;346:1061-6. [Crossref] [PubMed]
- Degner LF, Sloan JA. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol 1992;45:941-50. [Crossref] [PubMed]
- Tariman JD, Berry DL, Cochrane B, et al. Physician, patient, and contextual factors affecting treatment decisions in older adults with cancer and models of decision making: a literature review. Oncol Nurs Forum 2012;39:E70-83. [Crossref] [PubMed]