Therapeutic suggestions with critically ill in palliative care
Introduction
Nowadays, the progressive development of the technology of life support and monitoring has led the health care professionals (HP) to underestimate the importance of human contact, and gradually ignore active communication with the patient. Especially in cases of critically ill patients, professionals rely much more on the numerical values produced by machines and monitors than on direct communication with the patients.
We argue that critically ill patients require not only physical (somatic) care, but also psychological support. At any stage of illness, HPs need to help the patients to understand the aim and usefulness of the treatment, and to give them information about the peculiar or frightening aspects of the situation, in order to promote positive processing.
Research data show that HPs are not aware of the communicational inefficacy in their practice (1). For example, 35% of cancer patients receiving palliative care believed that their treatment was curative, and 33% with metastases believed incorrectly that the cancer was localized, while in 98% of these cases the physicians believed that they had correctly described the disease to the patient (2). In another study, 87% of patients were not familiar with the concept of radiation treatment before radiotherapy (2).
Patients who are unconscious, responding poorly to surgical/medical treatment, or breathing through a tracheostomy, as well as those patients who are conscious but unable to move, see or talk, are considered “critically ill” in psychological sense [e.g., (3-5)]. In his papers and books, Cheek called attention to the special needs and psychological condition of the patients in a “critical state”. These patients often have a sense of helplessness and dependence, experience loss of control, see themselves as victims of a “hostile medical system”, and consider themselves as passive recipients of incomprehensibly complex medical technology (6,7). This applies particularly to critically ill patients who are treated in the intensive care unit (ICU), where about 50% of hospital deaths occur.
The elements of a “good death”, based on interviews with terminally ill patients about their needs , proved to be: awareness, autonomy, self-chosen coping style, and open, honest communication (8). In cases of chronic patients, where no cure is available, courtesy (the general consideration of others), respect (the expression of regard for a specific individual), and engagement (the sense of commitment to the encounter) were the commonly expressed communicational needs of patients across various conditions (9). Thus, it is essential to explore novel and effective communication approaches in palliative care.
One of the emerging new approaches is the use of therapeutic suggestions in medical communication with patients enrolled in palliative treatment.
Therapeutic suggestions
Suggestions are verbal or non-verbal messages that the receiver involuntarily accepts and follows. Not only our spoken or written words but also the environment, objects and nonverbal messages (eye contact, sighs, and touches) can have suggestive effects (10).
Formal hypnosis is based on suggestive techniques; however, we can use suggestive methods without inducing hypnosis. This is due to the clinical observation that a person in a special (altered) mental state, like most of the patients undergoing medical interventions, can be highly susceptible to suggestions without any formal induction technique (4,6,7).
The effectiveness of therapeutic suggestions has been shown in many different areas of healthcare. For example, therapeutic suggestions proved to be effective in the treatment of somatisation (11) and skin disorders (12). Furthermore, earlier studies found that positive suggestions and imagery reduced pain associated with chronic illnesses, such as fibromyalgia (13), migraines and tension headaches (14-16), and various types of cancer (17,18). Neuroimaging studies provided support for some of these findings as well (19). These results are especially important in the context of palliative care because symptom management for chronic illnesses is a significant concern in this medical field.
Another highly relevant issue in palliative care is comfort during unpleasant medical procedures, as patients enrolled in palliative treatments are often subjected to curative or health sustaining medical procedures at the same time. The usefulness of therapeutic suggestions has been studied extensively in this area. Research confirms that suggestive techniques can reduce side effects and increase comfort with respect to various medical procedures, such as bone marrow aspiration and lumbar puncture (20,21), surgical procedures such as total hysterectomy (22-26), and chemotherapy (27). Benefits range from reduced pain and anxiety associated with the procedures to reduced nausea and bleeding [for reviews see (28,29)]. Similarly, the use of therapeutic suggestions by the medical team can reduce the unpleasantness of radiological procedures and biopsies by diminishing pain, anxiety, and procedure times, and by reducing the occurrence of adverse events (30-33).
Reduced procedure and room times, hospital stay, medication consumption, and complications also result in significant cost savings for institutions and patients. For example, Disbrow, Bennett and Owings (34) were able to realize a cost saving of $1,200 per patient by implementing a simple 5-minute personalized suggestive script. The script contained suggestions concerning the early return of gastrointestinal motility, and was used with patients undergoing intra-abdominal operations. Other cost-benefit analyses have also found that the use of suggestive techniques in conjunction with unpleasant medical procedures is cost-effective (30-32).
The scope of palliative care has been gradually widening in the past decade. While palliative treatment was historically considered end of life care, only provided when no curative options were available, it recently has been introduced to more and more medical fields as an adjunct to curative or life-prolonging interventions. Accordingly, there is an increasing recognition of the need for proactive palliative options in the intensive care unit (35), providing pain and symptom management, and improving consistency of communication with the patients. As shown by a recent series of studies, therapeutic suggestions can be considered a viable option. These studies found that patients who were supported by a technique called psychological support based on positive suggestions (PSBPS) (36) needed less benzodiazepines, opioids, and α2-agonists during their stay at the ICU, indicating improved non-pharmacological symptom management (37-39).
Stress cognition and suggestions
Patients treated in the ICU unit find themselves in a strange and foreign environment where not much makes sense due to a lack of information and lack of context. An absence of security, information, and control cause stress (40), provoking extra physical burdens (41). Their experiences reach them as little mosaic pieces, from a self-centered point of view and every stimulus can affect them as a suggestion (4,6,7). When patients try to piece their “mosaic of experiences” together they might form a frightening picture. The key principle of PSBPS is to guide the interpretation of the whole situation in a positive direction, in order to achieve trust and co-operation. Despite evidence in psychological literature proving that warmth, love, and security are as vital to life as the perfect physical care (40,42,43), we usually don’t bear this fact in mind in somatic medicine, especially when a patient’s life is in danger. In situations of life and death, the provision of comfort and communication is often neglected. However, using PSBPS, professionals are able to reframe medical interventions perceived by the patient as intrusions into physical and mental privacy as actions of healing and care. This positive interpretation of external and internal events can act as an autosuggestion, which can further promote healing or prevent the harmful effects of excessive stress. PSBPS is a complex and versatile intervention package that not only relies on verbal therapeutic suggestions, but also uses therapeutic psychological techniques such as guided imagery, relaxation, attentive listening, and even silence. These other techniques might not be immediately recognizable as “suggestion techniques” because they do not, or do not only, use words. Nevertheless, the therapeutic process engendered by the use of these techniques can be interpreted in a similar way to the workings of verbal suggestions. They evoke involuntary thoughts, emotions, behaviours, and mental states, which in turn promote the healing process. Interpreting suggestions in this broader sense allows for the therapists and medical staff using PSBPS to fit these various psycho-behavioural tools into a coherent therapeutic framework.
In our recent series of studies in the ICU, 220 ventilated patients received either standard care, or standard care plus a 30 minute long psychological guidance based on positive suggestions every day of their hospitalization, irrespective of their medical state and state of consciousness. Control and intervention groups were comparable regarding demographics and health status. According to a meta-analysis of this study series, mechanical ventilation and length of stay were reduced by 2.5 days, which is 25–30% less time than control patients. Survival was 20% higher in the suggestion group, although this latter difference between groups did not reach statistical significance (44). One of the most interesting findings was that both surviving and deceased patients had comparably shorter care in the suggestion groups (39). Regarding subjective experiences, suggestion group patients had fewer negative perceptions, less pain, more positive thoughts and emotions, more positive attitude towards the staff, more intensive physical activity, and feelings of self-efficiency (45). These benefits are shown to serve as protective factors against PTSD (46). The same effect was reached using in-person communication or playback of a recorded script (37).
The theory of stress cognition (47) and an evolutionary approach (48) helps to understand the effectiveness and mechanisms of such an intervention.
Kulcsár’s (47) extensive literature review explains that due to critical circumstances, changes take place in the central nervous system (CNS) which lead to an altered state of consciousness, and in this state, the processing of affective information is predominant. The changes that occur in the CNS as a result of stress involve altered functioning of the hippocampus and amygdala. This altered functioning can result in a disruption on normal memory processes, specifically, causing a disconnection of space, time and agency within memory events (49-51). These alterations are greater if the stress is more serious (51-54). In this altered state, the need for social support increases, as the person can become more susceptible to suggestions, and depending on the emotional interpretation, an event can suggest danger or reassurance (55,56). Due to the aforementioned changes in the CNS, the boundaries of the self weaken or vanish (57) because of reduced activation of the “who system”, the brain system responsible for consciousness of the agent of an action (58), and the “emotional who system”, a neural system supporting the attribution of an emotion to self or other (59). The weakened self-boundary strengthens the bridge between mind and body, because both social and visceral information is processed in the insula (60-63), and here social influences are transferred to a visceral level. Thus, words can directly affect the body of the other (47). Increased importance of the communicating partner is demonstrated by the finding that stronger suggestive effects are achieved through steady rapport (39).
At first glance, this function that leaves us so vulnerable to social interactions in critical situations might seem maladaptive, but only so long as we don’t recognize its purpose. According to Csányi (64,65), the purpose of evolution is improving survival, and the key to survival is adaptation to the environment. This explains why animals in the wild have fine-tuned sensory organs. As humans, we must to adapt to an alternate environment, namely the mind of the other. By co-operating with ingroup members, we become more than ourselves, a super-organism or survival machine, while the outgroup can signify mortal danger. Accordingly, it is crucial to be faithful to the ingroup, including its customs and rules, and to avoid becoming involved with the outgroup (64,65). According to our theoretical framework, we as health care providers represent the outgroup for the patient on a basic emotional level of interpretation, a threat to survival. But, if we can include them as a member of our own group, they will likely calm down and co-operate.
We argue that the opened self-boundaries and self-centred point of view might have an evolutionarily adaptive role, namely to allow us to break the integration with our original group and join a new group if it aids our survival. This flexibility of boundaries can be just as important in positive and negative critical life events and can mean the difference between posttraumatic growth and posttraumatic stress disorder when lacking a group we are in a state of constant stress; however, when part of a group we are much more ready to trust and follow the group›s lead. In a medical setting, this can act as an energy saving function that can lead to the acceptance of treatment and reduced stress at the same time. Bejenke (6) said that patients accept suggestions according to a subjective hierarchy, and we also argue that the provision of a trustworthy, supportive, and strong group amidst an environment full of “alien minds” is of utmost importance for the patient. Often, the most trusted group member is the one at the top of the hierarchy; however, the most important conditions for earning the trust of the patient is being aligned with the patient’s inner world, and acting according to her/his expectations [The ongoing nurse-led POPPI trial is a good example of utilizing the potential of carers who are not on top of the hierarchy to provide psychological support for patients in the ICU (66)].The role of the suggestive technique of “pacing-leading” (see Box 1) is to provide continuity and trust between the former and the new group. Using this strategy, a patient is better able to accept what the carer gives, attune to it, and use the seeds of support provided to grow an entire tree of competencies and support (48).
Full table
This approach can be very powerful and leads to improvement, even with a limited number of sessions. The effectiveness of the approach can be well demonstrated by cases from the clinical practice of the first author, AKSz. As a psychologist in the ICU, she treated a man on one occasion only, and told him to switch his brain to a channel where something agreeable would happen while he was recovering in the ICU. After 2 weeks of ventilation and anaesthesia, he was surprised to wake up in the ICU because he had experienced being on a two-week fishing trip. Another lady felt that AKSz was her unremitting guardian angel for a month, when in reality they had only met 3 or 4 times. Both of these patients had successfully recovered.
While communicating with the patient, we are aware of the fact that many aspects of our presence, not only our words, act as suggestions. Taking advantage of this, we strive to activate the patient’s spontaneous response processes by stimulating their inner source of wellbeing, namely their healing and calming thoughts. This type of communication helps the client to find a new and reassuring frame for her/his situation. Evoking one sensory modality of a past event can result in the automatic activation of other modalities of the same event or memory. Therefore, by evoking a good memory, the comfortable state of the body which accompanied the event is evoked at the same time, helping the body to return to a more agreeable state (67,68). Again, we interpret this as a suggestive effect, whereby feelings and ideas involuntarily evoke other related feelings, ideas, and bodily processes. This cascade of associations happens automatically, without the presence of a skilled therapist. Thinking in this framework can be used to explain not only the effects of words on physical and mental well-being, but also those of the environment, context, ideas, and mental states. The PSBPS techniques allow control over this process by guiding the patient towards more positive association chains, or by minimizing the effects of negative ones. By providing a positive narrative or interpretation of the patient’s experiences and bodily sensations we can guide the chain of association. For example, instead of interpreting strange sensations as pain and signs of illness, we might focus on the intensive work of the body as it moves toward recovery. A solid positive narrative may be a protective factor against PTSD and might nudge the patient toward post traumatic growth.
Studies indicate that some forms of semantic information processing remain intact in unconscious patients (69,70). Our studies also indicate that starting PSBPS with patients early, while they are still unconscious, can lead to better results than waiting for the return of consciousness before starting treatment (36). In our clinical experience, patients sometimes repeat the words they hear while unconscious, treat us as if we are familiar upon regaining consciousness (71,72), or give indications of recognition while in a coma vigil. For example, a patient who was blind after an extensive stroke, and thought to be completely lacking consciousness, could learn to communicate through hand-pressing, and started crying at an emotional part of a conversation. How reassuring would it have been for him to be treated as if he were alive by someone?
Reasonable quality of life and well-being can be maintained, even when there is no chance for a long life. Even the last minutes of life can be very valuable if they are used well. Furthermore, as death is our final life crisis to resolve well (1,73,74), it’s important what happens in these moments, whether we are in the ICU or elsewhere. But, the constantly busy ICU staff often views spending time with dying patients as a waste. In reaction to this attitude, a colleague working in hospice said: “in hospice, when everybody is busy, we will even direct the cleaning lady to hold the hand of the dying one.” The ICU staff can view death as an event which consists mainly of fear and suffering, rather than an opportunity to say farewell to loved ones and the world (75), which can be damaging to the mental hygiene of the staff themselves. It is better to encourage the dying patient to relax and exploit every minute, allowing both patient and staff to learn something reassuring about death. See Box 2 for case examples.

Full table
Often our only task is to clean up the inner psychological environment of the patient, to help him/her establish goals. For example, one of the old male patients on AKSz’s ward became catatonic one day. AKSz realised that because the catatonic state had developed in the ICU, staff at the ICU were also the ones who could break it. After the patient had been catatonic for half a day, AKSz started a kind of de-hypnosis and isolated the patient from the stimuli. Within a few minutes the patient established contact. The patient revealed that while in catatonia, he had horrible nightmares. It is not certain whether his life was extended by breaking the catatonia and ending the nightmares, but his remaining lifetime became a life worth living. Many of the patients admitted to the ICU are at the end of their lives. So the goal can’t be the restoration of former functioning, either physically or psychologically. As we can see from the above mentioned cases, the psychologist can restore the patient›s courage, dignity and ability to make personal decisions, during recovery and in the process of dying. AKSz cites many cases when after a long treatment with no improvement, a patient could either die or recover after having the chance to look at her/his global state (71). This can even occur while a patient is in a coma vigil. We believe that open and positive communication likely enables patients to make their own decisions, and to choose life or death. We think that our finding, which shows that the length of recovery and the process of dying were shorter due to PSBPS, complements and supports this idea.
The main contribution of our work is to point out that we are evolutionarily wired social beings in need of a protective relationship. If this inherent characteristic of our patients is not taken into consideration, treatment is 25–30% longer, mortality may increase, costs increase, quality of life may decline because of physical and psychological iatrogenic effects. Furthermore, the patient will have a greater risk of developing PTSD following treatment. If, however, these psychological and social needs are provided for, then the patient may progress in his/her own way, be it recovery or farewell to life. Meeting these needs contributes not only to a better quality of life, but also to a better quality of death.
Speaking about death and dying
We can speak directly or indirectly about death and dying (1).
A large majority of terminally ill patients (about 80%) are not afraid of death, but they may fear the process of dying: Patients are afraid of the prolonged dying process, especially if it is full of pain and suffering (76). Fortunately, these aspects can be managed—among other things—by well formulated suggestions.
Contrary to the common preconception, most patients find that open communication, and talking about death is very important, as it provides satisfaction and rest (8). It is recommended to use the words “death” and “dying” when discussing end of life issues, instead of the euphemistic phases ‘poor prognosis’, or ‘things look bad’ [(77), p. 102].
A report of a nurse who was engaged in the treatment of an ICU patient illustrates the possibility of open communication about death. The male patient in his 30s expressed his wish not to be on a ventilator (after 6 weeks of mechanical ventilation): “I told him at the time that ‘you understand that means that you would probably die’ and he said, ‘yes I know that’.” [(78), p. 298].
When the patient raises the topic of death, we can elaborate on it by inquiring about the motives underlying their initiatives (before or after giving answers to the direct questions). For example, a technique reported by a nurse in a study on discussing end-of life issues: “I am going to die?”—‘Well, what makes you ask that question?’… or: “How long have I got?” ‘What makes you ask this?’ [(79), p. 139]. These “turning-back” questions may start a deep and rich communication tailored to the actual needs of the patients.
With indirect communication it is still possible to address the topic of death and dying with those patients who do not want to discuss their prognosis.
There are a great many possibilities to express that death is a normal part of our lives.
Some suggestive techniques based on images or themes that may be helpful in this regard include the following:
- Circles of life, seasons, falling leaves, as they enrich the ground, thus supporting the new cycle, etc.;
- Some patients would like to contact a religious consultant;
- “My grandfather just started to plant grapes now. He is 77...”;
- Ebb and flow, big storms, the waves of the sea, sunrise/sunset—all lend themselves to speaking about the inner, profound laws and processes of nature. In this context, death also appears as a phenomenon that has its own laws.
Usually the consideration that the next generation (our children and grandchildren) follow us, or that the world became richer by means of our contributions (books, theories, methods, teaching, houses, meals, gardens, etc.) gives a sense of peace and satisfaction to many patients. By simply talking about close relatives and/or “results” of actions, the patients may come to realize the richness of their lives, and consequently accept death more easily.
Discussion
As illustrated above, therapeutic suggestions can assert a clinically meaningful effect that can seriously improve the well-being and quality of life of patients by facilitating effective symptom management and a reduction in required medications.
Using PSBPS to support ventilated patients in the ICU reduced their opioid and sedative requirements by 65%, and decreased time spent on mechanical ventilation from 232 hours on average to 85 hours on average, resulting in a substantial increase in patients’ capacity to make informed decisions and communicate (37,38).
The method of therapeutic suggestion, used as a simple communicational device, can easily be incorporated into the everyday work in a clinical environment and can be readily learned by the entire medical and nursing staff.
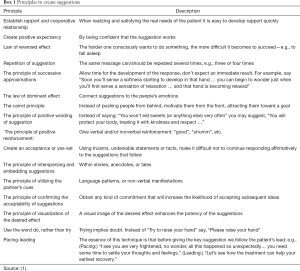
The more people who adhere to this style of communication (i.e., doctors, nurses, physiotherapists, psychologists, and other staff members), the more a beneficial effect can be expected. This is especially true when the communication is individualized, custom tailored to the special requirements of the patient and the personal style of the caregiver. See Box 1 for a summary of key principles to create suggestions. Box 3 lists possible techniques to elicit non-pharmacological pain control.

Full table
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Varga K. Suggestive communication with critically III patients in the context of death and dying. In: Kreitler S. editor. Confronting dying and death. Health Psychology Research Focus. New York: Nova Science Publishers, 2012:293-314.
- Hancock K, Clayton JM, Parker SM, et al. Discrepant perceptions about end-of-life communication: a systematic review. J Pain Symptom Manage 2007;34:190-200. [Crossref] [PubMed]
- Cheek DB. Hypnosis: an additional tool in human reorientation to stress. Northwest Med 1958;57:177-82. [PubMed]
- Cheek DB. Communication with the critically ill. Am J Clin Hypn 1969;12:75-85. [Crossref] [PubMed]
- Cheek DB. Unconscious reactions and surgical risk. West J Surg Obstet Gynecol 1960;69:325-8. [PubMed]
- Bejenke CJ. Painful medical procedures. In: Barber J. editor. Hypnosis and suggestion in the treatment of pain. New York & London: Norton & Company, 1996:209-65.
- Bejenke CJ. Preparation of patients for stressful medical interventions: Some very simple approaches. In: Peter B, Trenkle B, Kinzel FC, et al. editors. Hypnosis International Monographs No 2: Munich lectures on hypnosis and psychotherapy. München: MEG-Stiftung, 1996.
- Goldsteen M, Houtepen R, Proot IM, et al. What is a good death? Terminally ill patients dealing with normative expectations around death and dying. Patient Educ Couns 2006;64:378-86. [Crossref] [PubMed]
- Thorne SE, Harris SR, Mahoney K, et al. The context of health care communication in chronic illness. Patient Educ Couns 2004;54:299-306. [Crossref] [PubMed]
- Varga K. Suggestive techniques connected to medical interventions. Interv Med Appl Sci 2013;5:95-100. [Crossref] [PubMed]
- Thomas KB. General practice consultations: is there any point in being positive? BMJ 1987;294:1200-2. [Crossref] [PubMed]
- Spanos NP, Stenstrom RJ, Johnston JC. Hypnosis, placebo, and suggestion in the treatment of warts. Psychosom Med 1988;50:245-60. [Crossref] [PubMed]
- Castel A, Pérez M, Sala J, et al. Effect of hypnotic suggestion on fibromyalgic pain: comparison between hypnosis and relaxation. Eur J Pain 2007;11:463-8. [Crossref] [PubMed]
- Friedman H, Taub HA. Brief psychological training procedures in migraine treatment. Am J Clin Hypn 1984;26:187-200. [Crossref] [PubMed]
- Friedman H, Taub HA. Extended follow-up study of the effects of brief psychological procedures in migraine therapy. Am J Clin Hypn 1985;28:27-33. [Crossref] [PubMed]
- Nolan R, Spanos NP, Hayward A, et al. Hypnotic and nonhypnotic imagery based strategies in the treatment of tension and mixed tension/migraine headache. Unpublished manuscript, Carleton University, Ottawa, 1989.
- Graffam S, Johnson A. A comparison of two relaxation strategies for the relief of pain and its distress. J Pain Symptom Manage 1987;2:229-31. [Crossref] [PubMed]
- Zimmerman L, Pozehl B, Duncan K, et al. Effects of music in patients who had chronic cancer pain. West J Nurs Res 1989;11:298-309. [Crossref] [PubMed]
- Derbyshire SW, Whalley MG, Oakley DA. Fibromyalgia pain and its modulation by hypnotic and non‐hypnotic suggestion: An fMRI analysis. Eur J Pain 2009;13:542-50. [Crossref] [PubMed]
- Zeltzer L, LeBaron S. Hypnosis and nonhypnotic techniques for reduction of pain and anxiety during painful procedures in children and adolescents with cancer. J Pediatr 1982;101:1032-5. [Crossref]
- Liossi C, Hatira P. Clinical hypnosis versus cognitive behavioral training for pain management with pediatric cancer patients undergoing bone marrow aspirations. Int J Clin Exp Hypn 1999;47:104-16. [Crossref] [PubMed]
- Maroof M, Ahmed SM, Khan RM, et al. Intra-Operative Suggestions Reduces Incidence of Post-Hysterectomy Emesis. J Pak Med Assoc 1997;47:202-4. [PubMed]
- Nilsson U, Rawal N, Enqvist B, et al. Analgesia following music and therapeutic suggestions in the PACU in ambulatory surgery; a randomized controlled trial. Acta Anaesthesiol Scand 2003;47:278-83. [Crossref] [PubMed]
- Jakubovits E, Janecskó M, Varga K. Műtét előtti-alatti szuggesztiók hatása a betegek posztoperatív állapotára [The effect of pre- and intra-operative suggestions on patients’ postoperative condition]. Aneszteziológia és Intenzív Terápia, 1998:3-9.
- Lauder GR, McQuillan PJ, Pickering RM. Psychological adjunct to perioperative antiemesis. Br J Anaesth 1995;74:266-70. [Crossref] [PubMed]
- van der Laan WH, van Leeuwen BL, Sebel PS, et al. Therapeutic suggestion has no effect on postoperative morphine requirements. Anesth Analg 1996;82:148-52. [PubMed]
- Zeltzer LK, Dolgin MJ, LeBaron S, et al. A randomized, controlled study of behavioral intervention for chemotherapy distress in children with cancer. Pediatrics 1991;88:34-42. [PubMed]
- Richardson J, Smith JE, McCall G, et al. Hypnosis for nausea and vomiting in cancer chemotherapy: a systematic review of the research evidence. Eur J Cancer Care (Engl) 2007;16:402-12. [Crossref] [PubMed]
- Kekecs Z, Nagy T, Varga K. The effectiveness of suggestive techniques in reducing post-operative side effects: a meta-analysis of randomized controlled trials. Anesth Analg 2014;119:1407-19. [Crossref] [PubMed]
- Lang EV, Berbaum KS, Faintuch S, et al. Adjunctive self-hypnotic relaxation for outpatient medical procedures: a prospective randomized trial with women undergoing large core breast biopsy. Pain 2006;126:155-64. [Crossref] [PubMed]
- Lang EV, Rosen MP. Cost Analysis of Adjunct Hypnosis with Sedation during Outpatient Interventional Radiologic Procedures 1. Radiology 2002;222:375-82. [Crossref] [PubMed]
- Lang EV, Ward C, Laser E. Effect of team training on patients' ability to complete MRI examinations. Acad Radiol 2010;17:18-23. [Crossref] [PubMed]
- Montgomery GH, Weltz CR, Seltz M, et al. Brief presurgery hypnosis reduces distress and pain in excisional breast biopsy patients. Int J Clin Exp Hypn 2002;50:17-32. [Crossref] [PubMed]
- Disbrow EA, Bennett HL, Owings JT. Effect of preoperative suggestion on postoperative gastrointestinal motility. West J Med 1993;158:488-92. [PubMed]
- Norton SA, Hogan LA, Holloway RG, et al. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med 2007;35:1530-5. [Crossref] [PubMed]
- Varga K, Varga Z, Fritúz G. Psychological support based on positive suggestions in the treatment of a critically ill ICU patient—a case report. Interv Med Appl Sci 2013;5:153-61. [Crossref] [PubMed]
- K Szilágyi A, Diószeghy C, Fritúz G, et al. Shortening the length of stay and mechanical ventilation time by using positive suggestions via MP3 players for ventilated patients. Interv Med Appl Sci 2014;6:3-15. [Crossref] [PubMed]
- Schlanger J, Fritúz G, Varga K. Therapeutic suggestion helps to cut back on drug intake for mechanically ventilated patients in intensive care unit. Interv Med Appl Sci 2013;5:145-52. [Crossref] [PubMed]
- K Szilágyi A, Diószeghy C, Benczúr L, et al. Effectiveness of psychological support based on positive suggestion with the ventilated patient. J Ment Health 2007;2:149-70.
- Levine S, Weinberg J, Ursin H. Definition of the Coping Process and Statement of the Problem. In: Levine S, Baade E, Ursin H. editors. Psychobiology of Stress: A Study of Coping Men. New York: Academic Press, 1978:3-22.
- Selye H. The stress of life. New York: McGraw-Hill, 1956.
- Spitz RA. Hospitalism; an inquiry into the genesis of psychiatric conditions in early childhood. Psychoanal Study Child 1945;1:53-74. [Crossref] [PubMed]
- Harlow HF, Harlow M. Social deprivation in monkeys. Scientific American. 1962;207:136-46. [Crossref] [PubMed]
- K Szilágyi A, László Z, Kekecs Z, et al. A pszichés faktor hatása az ápolási és a lélegeztetési időre intenzívterápiás osztályon [The effects of the psychological factor in the intensive care unit on treatment and ventilation time]. Aneszteziológia és Intenzív Terápia 2014;44:22.
- Tóth Á. Szuggesztív hatások tükröződése az élménymintázatban - Intenzív osztályon kezelt, lélegeztetett betegek élményeinek vizsgálata [Subjective effects in phenomenal experiences – The study of experiences of ventilated patients treated in the intensive care unit]. [Doctoral Dissertation]. Budapest: KGRE, 2013.
- Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther 2000;38:319-45. [Crossref] [PubMed]
- Kulcsár Z. A társas interakciók pszichológiai hatásai és agyi mechanizmusai. Egy hipotézis körvonalai. Társas támogatás [The psychological effects and neural mechanisms of social interaction. The outlines of a hypothesis]. In: Kulcsár Z, editor. Teher alatt… Pozitív traumafeldolgozás és poszttraumás személyiségfejlődés. Budapest: Trefort Kiadó, 2005:315-93.
- Szilágyi AK. Az intenzívterápia harmóniájának nyomában [In pursuit of the harmony of intensive care]. In: Varga K, Gősiné Greguss A. editors. Tudatállapotok, hipnózis, egymásra hangolódás. Budapest: L’Harmattan Kiadó, 2012:149-78.
- Bower GH, Sivers H. Cognitive impact of traumatic events. Dev Psychopathol 1998;10:625-53. [Crossref] [PubMed]
- Wheeler MA, Stuss DT, Tulving E. Toward a theory of episodic memory: the frontal lobes and autonoetic consciousness. Psychological Bulletin 1997;121:331-54. [Crossref] [PubMed]
- Jacobs WJ, Nadel L. Neurobiology of reconstructed memory. Psychol Public Policy Law 1998;4:1110-253. [Crossref]
- Spiegel D, Cardeña E. Disintegrated experience: The dissociative disorders revisited. J Abnorm Psychol 1991;100:366-78. [Crossref] [PubMed]
- Sierra M, Berrios GE. Depersonalization: neurobiological perspectives. Biol Psychiatry 1998;44:898-908. [Crossref] [PubMed]
- Tellegen A, Atkinson G. Openness to absorbing and self-altering experiences ("absorption"), a trait related to hypnotic susceptibility. J Abnorm Psychol 1974;83:268-77. [Crossref] [PubMed]
- Albrecht TL, Burleson BR, Goldsmith D. Supportive communication. In: Miller GR, editor. Handbook of Interpersonal Communication. Thousand Oaks, London, New Delhi: Sage Publications, 1994:419-49.
- Burleson BR, Albrecht TL, Sarason IG. Communication of social support. Thousand Oaks, London: Sage publication, 1994.
- d'Aquili EG, Newberg AB. The mystical mind: Probing the biology of religious experience. Minneapolis, MN: Fortress Press, 1999.
- Georgieff N, Jeannerod M. Beyond consciousness of external reality: a “who” system for consciousness of action and self-consciousness. Conscious Cogn 1998;7:465-77. [Crossref] [PubMed]
- Ochsner KN, Knierim K, Ludlow DH, et al. Reflecting upon Feelings: An fMRI Study of Neural Systems Supporting the Attribution of Emotion to Self and Other. J Cogn Neurosci 2004;16:1746-72. [PubMed]
- Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci 2002;3:655-66. [Crossref] [PubMed]
- Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol 2003;13:500-5. [Crossref] [PubMed]
- Craig AD. Significance of the insula for the evolution of human awareness of feelings from the body. Ann N Y Acad Sci 2011;1225:72-82. [Crossref] [PubMed]
- Craig AD. How do you feel—now? the anterior insula and human awareness. Nat Rev Neurosci 2009;10:59-70. [Crossref] [PubMed]
- Csányi V. Az emberi természet. Humánetológia [Human nature. Human ethology]. Budapest: Vince Kiadó, 1999.
- Csányi V. Az emberi viselkedés. [Human behavior]. Budapest: Sanoma, 2006.
- Mouncey P. ISRCTN53448131: Provision of psychological support to people in intensive care 2015. Available online: http://www.isrctn.com/ISRCTN53448131?q=&filters=conditionCategory:Mental%20and%20Behavioural%20Disorders&sort=&offset=1&totalResults=1636&page=1&pageSize=20&searchType=basic-search
- Bandler R, Grinder J. Reframing: Neuro-Linguistic Programming and the Transformation of Meaning. Moab, UT: Real People Press, 1982.
- Grinder J, Bandler R. Trance-formations: Neuro-linguistic programming and the structure of hypnosis. Moab, UT: Real People Press, 1981.
- Owen AM, Coleman MR, Boly M, et al. Detecting awareness in the vegetative state. Science 2006;313:1402. [Crossref] [PubMed]
- Benczúr L. Doctoral dissertation. Pozitív szuggesztiók szerepe az intenzív osztályon fekvő lélegeztetett betegek kezelésében [The role of positive suggestions in the treatment of patients intensive care unit patients]. [Doctoral Dissertation]. Budapest: ELTE, 2012.
- K Szilágyi A. Suggestive communication in the intensive care unit. In: Varga K. editor. Beyond the Words: Communication and Suggestion in Medical Practice. New York: Nova Science Publishers, 2011:223-37.
- Varga K. The possible explanation of metaphors in re-interpreting negative life events: our experiences with the critically ill. Hypnos 2004;31:201-7.
- Yalom ID. Existential Psychotherapy. New York: Basic Books, 1980.
- Biró E. Suggestive Elements in the Communication with Patients Facing Death: A RealisticInterpretation of Hope at the End of Life. In: Varga K. editor. Beyond the Words: Communication and Suggestion in Medical Practice. New York: Nova Science Publishers, 2011:249-60.
- Varga ZK, Baksa D, Szilágyi AK. A halál iránti attitűd és összefüggéseinek vizsgálata kritikus állapotú betegek ápolásával foglalkozó populációkban: intenzívterápiás osztályon illetve hospice-ellátásban dolgozó nővérek körében. Kharon 2009;13:8-54. [The study of attitude toward death, and its correlates in a population of carers of critically ill patients: among intensive care and hospice nurses].
- Kutner JS, Steiner JF, Corbett KK, et al. Information needs in terminal illness. Soc Sci Med 1999;48:1341-52. [Crossref] [PubMed]
- Marik PE, Zaloga GP. CPR in terminally ill patients? Resuscitation 2001;49:99-103. [Crossref] [PubMed]
- Hsieh HF, Shannon SE, Curtis JR. Contradictions and communication strategies during end-of-life decision making in the intensive care unit. J Crit Care 2006;21:294-304. [Crossref] [PubMed]
- Clayton JM, Butow PN, Tattersall MH. When and how to initiate discussion about prognosis and end-of-life issues with terminally ill patients. J Pain Symptom Manage 2005;30:132-44. [Crossref] [PubMed]
- Engelberg RA, Patrick DL, Curtis JR. Correspondence between patients' preferences and surrogates' understandings for dying and death. J Pain Symptom Manage 2005;30:498-509. [Crossref] [PubMed]
- Winchester TA. Teaching communication skills to nursing home certified nursing assistants. Geriatr Nurs 2003;24:178-81. [Crossref] [PubMed]
- Parker S, Clayton J, Hancock K, et al. Communicating prognosis and issues surrounding end of life in adults in the advanced stages of a life-limiting illness: A systematic review. Sydney: NHMRC Clinical Trials Centre and the University of Sydney, 2006.


