Sixty-day mortality after stereotactic radiosurgery of brain metastases—a forgotten palliative treatment outcome
The ultimate outcome of individuals with brain metastases (BRM) is not often in doubt. However, it is clear that all patients with BRM do not share the same prognosis and should not receive the same treatment. Stereotactic radiosurgery (SRS) is an attractive option for treatment of BRM because it avoids whole-brain radiotherapy (WBRT)-associated morbidity. But SRS is limited by regional central nervous system relapses and short survival (SS) in some people (1). In BRM trials, more than 10% of the treated patients died within 8 weeks (2). Similar findings of SS have recently emerged following WBRT or SRS of BRM (2-4). The resulting early death could denote overtreatment and call into question the need to treat. Nevertheless, because of the significant morbidity and mortality associated with BRM as well as with expected survival of less than 3 months, these patients should be considered for palliative care (5). The principal aim of therapy is the improvement of the duration and quality of life. We examined the early mortality rate at our gamma knife radiosurgery center because regular audits of rendered service are expected from any charge involved with patient care.
In a retrospective analysis of 121 people treated by SRS for BRM between March 2000 and April 2010, we identified 29 (24%) patients who died within 60 days following therapy (Table 1). Seventeen were women and 12 were men. The mean age of the deceased patients was 56 (range, 36−82) years. Many individuals exhibited a poor performance status at presentation, and about half of the studied subjects possessed other significant illness at the time of BRM diagnosis. The deceased were diagnosed with six different primary malignancies; the most common was lung cancer (62%) followed by colon (10%), breast (10%), bladder/kidney (10%) cancers and malignant melanoma (8%). The primary neoplasm was not under control in 45% of the cases, and extracranial metastases were detected in a third of the patients. BRM were associated with symptoms in 25 people (86%) and were solitary in 18 patients (62%). With respect to intracranial metastatic tumor locations, 48%, 24% and 28% were in the supratentorial or infratentorial compartments or in both regions of the brain, respectively. Concerning the SRS procedure, the median number of target BRMs was 1 (range, 1−5), the median applied margin dose (usually prescribed at the 50% isodose line) was 16 Gy (range, 12−22 Gy), and the median tumor volume was 2.9 cm3 (range, 0.2−20 cm3).
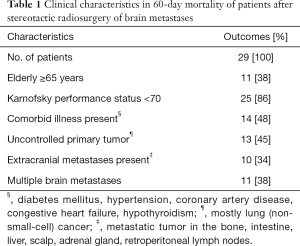
Full table
Outcomes after treatment of BRM often focus on median survival and toxicity. There is no national agreed standard rate for early death. The observed SS rates after WBRT have ranged from more than 10% to 54% (2,3,6), and our 24% incidence was following SRS. Several interesting observations about potential factors predictive of SS that have been noted by others were also seen in our review of cases. First, uncontrolled primary tumors were found in about half of the studied patients (2-4). Second, the frequency of multiple BRM detected in the examined subjects has ranged from 34% to 71% (2,4), and the frequency of extracranial metastases was from 26% to 57% (2-4). The poor performance status exhibited in the majority (86%) of our patients is in contrast to the fewer than 18% seen in the experience of Zindler et al. (4). In advanced cancer, almost 150 variables have been evaluated for their ability to predict prognosis; of all of them, performance status has consistently shown an association with survival duration (7).
The current study emphasizes three important SS considerations: (I) in people with a limited life span, any treatment could be considered an unjustified patient stress and poor utilization of health care resources; (II) when treatment is applied to an a-priori unfavorable cohort of people, early mortality may elicit an erroneous interpretation of ineffective therapy; (III) it is imperative to also bear in mind not to exclude those individuals with incorrectly predicted SS from receiving beneficial therapy.
The limitations of this retrospective study include the small number of subjects, heterogeneity in patient composition and possible selection bias because of missed cases. Additionally, the SS precluded an assessment of the possible causes of death (e.g., progression of BRM leading to neurological deterioration, the primary lesion or extracranial systemic disease), of the quality of short life and of the control of the treated BRMs. Regardless of whether early death was expected or unexpected, the event should lead to a reflection about the appropriateness of the therapeutic concept. If people at high risk of early death could be identified before starting therapy, they could potentially be offered other palliative management programs such as hospice care (8). Moreover, if factors associated with SS could be identified, then therapeutic strategies to minimize the chance of a patient developing these factors might represent opportunities to improve prognosis by reducing future early death occurrences.
In summary, although SS after SRS could not definitely be attributed to a specific prognostic factor, we believe that the poor performance status presented by patients increases the odds of dying early. Prognosis predictive models, developed because of physician inaccuracy in estimating life expectancy, are imperfect even if the systems perform well in large groups of people (4). The question remains—how can we be certain that a particular individual is near the end of life?
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ebner DK, Gorovets D, Rava P, et al. Patients with Long-Term Control of Systemic Disease Are a Favorable Prognostic Group for Treatment of Brain Metastases with Stereotactic Radiosurgery Alone. World Neurosurg 2017;98:266-72. [Crossref] [PubMed]
- Nieder C, Thamm R, Astner ST, et al. Prediction of very short survival in patients with brain metastases from non-small cell lung cancer. Cancer Ther 2008;6:163-66.
- Nieder C, Pawinski A, Molls M. Prediction of short survival in patients with brain metastases based on three different scores: a role for 'triple-negative' status? Clin Oncol (R Coll Radiol) 2010;22:65-9. [Crossref] [PubMed]
- Zindler JD, Jochems A, Lagerwaard FJ, et al. Individualized early death and long-term survival prediction after stereotactic radiosurgery for brain metastases of non-small cell lung cancer: Two externally validated nomograms. Radiother Oncol 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Tsao MN, Rades D, Wirth A, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol 2012;2:210-25. [Crossref] [PubMed]
- Lock M, Chow E, Pond GR, et al. Prognostic factors in brain metastases: can we determine patients who do not benefit from whole-brain radiotherapy? Clin Oncol (R Coll Radiol) 2004;16:332-8. [Crossref] [PubMed]
- Glare P, Sinclair C, Downing M, et al. Predicting survival in patients with advanced disease. Eur J Cancer 2008;44:1146-56. [Crossref] [PubMed]
- Warner A, Dahele M, Hu B, et al. Factors Associated With Early Mortality in Patients Treated With Concurrent Chemoradiation Therapy for Locally Advanced Non-Small Cell Lung Cancer. Int J Radiat Oncol Biol Phys 2016;94:612-20. [Crossref] [PubMed]


