Patients’ perceptions of palliative surgical procedures: a qualitative analysis
Introduction
Cancer is the leading cause of death in many developed countries and more than 7.6 million people die of cancer worldwide annually (1). When therapy in cancer patients is no longer considered curative, a palliative, patient-centered approach should be adopted for end-of-life care. Palliative care for incurable cancer can involve both medical and surgical strategies; however, the prevalence of palliative surgery in current practice is often underappreciated. Major US cancer centers have reported that 6–12% of all procedures were for palliative intent (2,3). Additionally, up to 40% of inpatient surgical consultations for oncology patients are for consideration of palliative surgical treatment (4).
The management of patients with incurable malignancies can be challenging, as many will experience significant symptoms or develop acute conditions from their disease or cancer therapies. In the palliative setting, the emphasis of treatment is placed on maintaining or improving quality of life. A number of modalities can be available for treatment of symptoms including chemotherapy, radiation, endoscopy, percutaneous interventions and surgery. Often, surgery is the only therapeutic option for relief of symptoms from the underlying malignancy. However, the decision to undergo an operation without curative intent, that has the potential to cause harm, should be extensively discussed with the patient, their family and their oncology team. Palliative surgical procedures have been associated with 28–40% complication rate and 9–36% mortality (2,3,5,6).
Numerous reports describe predictors of survival outcomes in palliative patients undergoing surgical therapy for symptom control (4,6,7). However, the patient’s perception of the “success” or benefit from the surgery in terms of satisfaction with treatment and alleviation of symptoms has not been well evaluated in the literature. Qualitative research has the advantage of understanding meanings and experiences inadequately captured with quantitative research (8). The objective of this study was to prospectively evaluate patients’ experiences and perceptions of palliative surgery for symptom control in advanced incurable malignancies through qualitative analysis.
Methods
Patients
Patients were prospectively recruited from a tertiary care cancer center (Sunnybrook Health Sciences Centre, Toronto, Ontario, Canada) from January 1, 2014 through December 31, 2014. Patients were enrolled from the inpatient and outpatient services of General Surgery, Surgical Oncology, Medical Oncology, Radiation Oncology, Palliative Care, Neurosurgery, and Orthopedic Surgery. Inclusion criteria were age >18 years, English speaking, incurable stage IV (metastatic) malignancy, planned surgery (elective/emergency), and less than 12-month expected survival. Demographic data was collected including age, sex, marital status, cancer type, type of operation, peri-operative morbidity and mortality. Operations were defined as emergency operations if the symptoms of disease or functional status of the patient were severe enough to require immediate hospital admission through the emergency room. Elective cases were performed in elective operating time within 4 weeks of the consent being signed in clinic. Eligible patients were approached for participation in the study and informed consent was obtained. This study was approved by the Sunnybrook Health Sciences Centre Research Ethics Board.
Interviews
Semi-structured, qualitative interviews were conducted in person with patients prior to surgery or, when this was not feasible (e.g., emergency procedures), within 48 h following surgery. It was felt that a patient who had an interview within 48 h of the operation would still be able to remember their pre-operative symptoms and would not have recouped any major symptomatic benefits from the operation as yet. A second interview was conducted one month post-operatively by phone. An interview guide was developed to direct the interview process but questions were open-ended to facilitate discussion. The interviews were a one-on-one interaction between a researcher and the patient and lasted approximately 20 minutes. Interviews were recorded and verbatim transcriptions were completed to enable analysis. Transcriptions were reviewed after six pilot interviews by the research team to ensure that areas of interest were being discussed; the interview guide was modified slightly to elucidate more information from future interviewees.
Qualitative analysis
Content analysis was used to qualitatively analyze the interview data in order to understand the meaning of the palliative surgery for patients (9,10). An inductive approach was used, as prior knowledge about the patient’s experience with palliative surgery was limited. Coding of the interview transcripts identified content-related categories directly derived from the interview data. Categories with underlying meaning were then linked together to form themes. Analysis was completed independently by three researchers (TD Hamilton, D Selby, and FC Wright) who subsequently met to discuss the themes. There was no discrepancy among the researchers regarding the generated themes.
Morbidity, mortality and survival
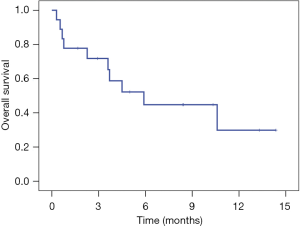
Peri-operative morbidity and mortality were determined using prospective chart review and defined according to the Clavien-Dindo classification (11). Overall survival (OS) was defined as the time from surgery until death or last follow-up and was calculated using Kaplan-Meier curve estimation.
Results
Patients
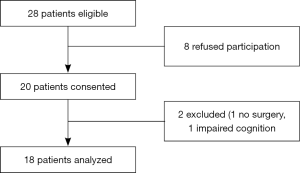
A total of 28 patients were eligible for participation during the study period (Figure 1). Eight patients declined to participate because they were either too tired/weak [3] or uncomfortable with the discussion of a palliative approach to care [5]; this included both elective and emergency patients. The remaining 20 were interviewed. Two patients were excluded from the final analysis after being interviewed; one patient did not have the planned surgical intervention and another patient had significantly impaired cognition. All patients completed the full interview. Six patients did not complete a 1-month post-operative interview because they had died [4] or were unable to be contacted [2]. There was a technical failure with the recording device and complete transcription was not available for the last 4 interviews in which it was used. Data saturation was achieved (based on the pre-operative interview) after 14 patients.
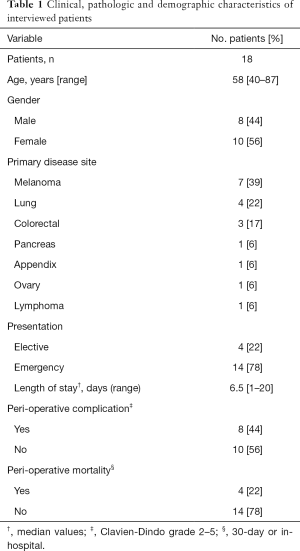
The median age of patients analyzed was 58 years (Table 1). There was a slight female predominance, 56% (10 of 18); the most common primary disease sites were melanoma [7], lung [4], and colorectal [3]. Most patients had surgical interventions that were an emergency (78%), rather than elective (22%). Indications for surgical intervention included: gastro-intestinal obstruction [9], impending/pathologic fracture [4], brain metastases [2], loco-regional disease control from extensive lymphadenopathy [2], and debulking of intra-abdominal tumor [1].
Full table
Morbidity, mortality and survival
Eight patients (44.4%) had peri-operative complications (grade 2–5) associated with their surgical procedure. Two patients had grade 2 complications; one had a urinary tract infection treated with antibiotics and one developed a deep venous thrombosis treated with anticoagulation. Two patients had grade 3 complications; both patients had significant wound infections requiring re-operation and antibiotics. Four patients (22.2%) had peri-operative mortality (grade 5); one patient developed disease progression and died of hepatic failure, two became significantly debilitated and died, and one developed an anastomotic leak requiring re-operation and died of sepsis. All four peri-operative mortalities were following emergency operations.
At the time of last follow-up (June 2015), 10 patients (56%) had died (all of disease): lung [3], colorectal [3], melanoma [2], pancreas [1], ovary [1]). Median OS was 6 months with a median follow-up of 4 months (Figure 2).
Qualitative analysis
The following themes were identified from the qualitative analysis for both pre- and post-operative interviews (Table 2).

Full table
No other option
The majority of patients (14 of 18) perceived that they had no choice in deciding whether or not to proceed with a palliative surgical intervention. Although most recognized that they had discussed other possibilities with their cancer care providers, these alternate options were largely dismissed. Many felt the option of non-operative care was essentially “doing nothing” and thus, not a valid option. Others stated that the choice to proceed with surgery was “life or death” in that not proceeding with surgery would ultimately lead to death and that surgery offered the sole chance of survival.
Pre-operative understanding/insight
There was a marked difference in understanding of the role of surgery between patients needing emergency versus elective interventions. Those undergoing an emergency palliative operation generally had a poor understanding of their prognosis and the role of surgery in overall care, as well as unrealistic expectations of what could be achieved with surgery (6 of 14 patients). Many voiced that they did not know, or were not told their prognosis. Others thought that their prognosis was much better than what was expected by their care providers. Regarding the role of surgery, most viewed it as necessary to survive. Many also stated expectations of getting back to a “normal life” after surgery. In contrast, all patients undergoing an elective surgical intervention seemed to have a more accurate understanding of their prognosis. They also saw surgery as a potential bridge to other therapies (i.e., chemotherapy or radiation) in addition to treating symptoms. Expectations were more realistic in this group as they had an understanding that surgery could help with symptoms but would not cure their disease.
Prolonged recovery
Post-operatively, participants described a prolonged recovery after surgery, even those without significant complications. The most commonly voiced limitations were of fatigue and restricted mobility. Some reported that they were unable to do as many activities compared to pre-operatively.
Benefits of surgery
All patients completing the post-operative interview perceived they had benefitted from surgery in the short or long term. All were thankful to be alive and attributed survival to surgery. Others gained significant improvement in symptomatology that prompted surgical intervention. Four patients also described an emotional benefit that surgery provided in the form of hope for the future.
Improved post-operative understanding/insight
Post-operatively, all patients (emergency and elective) seemed to have a better understanding of prognosis and the role of surgery in their overall care. In particular, those that had a limited understanding of prognosis pre-operatively had a much more realistic description at the post-operative interview. As well, many patients clearly described their overall multi-modal treatment plans, including chemotherapy and radiation, following recovery from surgery. All patients that were alive when assessed at one month post-operatively felt that they would make the same choice if faced with the same decision again.
Discussion
Palliative surgery is defined as a procedure with the primary intention of improving QOL and/or relieving symptoms caused by an advanced disease (12). The decision to recommend palliative surgery is complex (13). Few studies describe the tenets that guide decision-making for patients in palliative situations. Some have evaluated subjective patient symptom control, estimates of quality of life and early initiation of palliative care referrals (14-17). Others have qualitatively evaluated perceptions of pain and its management in cancer patients (18). Decision-making from the surgical oncologist’s perspective has also been analyzed (13). However, reports that qualitatively evaluate patients’ experiences and perceptions of palliative surgery are limited. This study reports what patients perceive to be their treatment options and the benefits of palliative surgery when faced with debilitating symptoms in a non-curative setting.
In this study, we identified a dominant peri-operative theme that patients felt they had “no other option” regarding the decision for palliative surgery. Most patients equated not undergoing surgery with imminent death, even for those for whom immediate death would not have resulted from not having surgery (e.g., impending fracture, spinal cord compression). This perception of “no other option” was more pronounced in the group of patients undergoing an emergency procedure. Similarly, patients’ general understanding of prognosis was limited or overestimated, particularly for the patients proceeding with emergency surgery. It is likely that the stressful hospital environment, combined with the patient’s acute symptomatology, may limit a patient’s ability to make objective decisions and may skew their perception of long-term survival (19-21); this may also fuel patient denial as a barrier to communication about realistic expectations from treatment. In contrast, patients undergoing elective palliative surgeries and post-operative patients had not only a more accurate appreciation of prognosis, but also a clearer understanding of the role of surgery in their overall treatment plan. The pre-operative limited patient understanding of treatment options and prognosis points to the need to focus on improving communication with patients and families so that expectations of the benefit of surgery can be appropriately managed.
In our series, 22% of patients died within 30 days of surgery and 56% had died within a median 4 months of surgery; this is considerable, but falling within the range of published series where peri-operative mortality was 9–36% (2,3,5,6). The high rate of peri-operative mortality in this study may be explained by the fact that 78% of the patients in the current study had emergency surgical inventions as opposed to elective procedures. The high mortality may also reflect that this was a small study (as suited to a qualitative investigation), which may have skewed our results. Importantly, our findings are consistent with previous population-based studies indicating that palliative surgery is a pre-terminal event for many patients, especially when performed for an emergency situation (22). We feel strongly that patients and families should be counseled about the overall significance of palliative surgery so that they make informed decisions and adequately prepare for their final days or months of life.
Interestingly, in spite of the significant rate of peri-operative complications (44%), surviving patients perceived they benefitted greatly from palliative surgery. Many patients gained improvement in the symptomatology that prompted the surgical intervention leading to an improvement in QOL. Importantly some patients reported an emotional benefit from surgery. They described that after the surgery they now had hope for their future. In more recent literature that discusses how to assess outcomes of palliative surgery, a number of authors have suggested that success be measured by relief of symptoms and improved QOL in addition to the standard measures of morbidity and mortality (7); these patient-reported outcomes are paramount in establishing high-quality surgical care in the palliative setting. Thus, despite the considerable peri-operative morbidity and mortality observed in this study, the patient-centered benefit should not be underappreciated.
The strengths of this study are the prospective evaluation of patients as well as assessments at two different time points (peri- and post-treatment) to identify potential changes in patient perceptions over time. As this study included a broad spectrum of palliative surgeries in both elective and urgent settings, it is generalizable to numerous physicians treating cancer patients at the end-of-life. Possible limitations of the study were the relatively small number of patients and the technical recording failure in four interviews. However, data saturation was achieved with our sample (23). In addition, performing initial interviews within 48 h of surgery is a potential limitation, as perceptions could be different than pre-operatively; however, due to the nature of surgery being performed in a timely fashion, this was necessary from a practical perspective. A second post-operative interview was not possible in six patients, which could confound the results. Unfortunately, this illustrates the gravity of disease in the study population. The eight patients that declined participation could potentially confound the results; weaker patients may have reduced performance status and patients uncomfortable with a palliative approach to care may be in denial towards the gravity of their disease, which would affect their perception of palliative surgical procedures. The perspective of individual patient’s family members, while often critical to decision-making, was not specifically evaluated in this study.
Conclusions
As physicians treating advanced cancer patients at the end-of-life, we should focus on improving communication with patients and their families so that they better understand prognosis and all potential surgical and non-surgical options for care (24). Importantly with this qualitative study, we identified that although morbidity and mortality were high, patients perceived that they benefit physically and mentally from a palliative operation. In the era of reporting patient-centred outcomes, the patient’s voice stating whether or not they felt they benefited from their palliative operation should be acknowledged.
Acknowledgements
We thank the Departments of Surgery and Palliative Medicine at Sunnybrook Health Sciences Centre for assisting in recruiting patients for this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Sunnybrook Health Sciences Centre Research Ethics Board (No. 2013-455) and written informed consent was obtained from all patients.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA: A Cancer Journal for Clinicians 2011;61:69-90. [Crossref] [PubMed]
- Miner TJ, Brennan MF, Jaques DP. A. Prospective, Symptom Related, Outcomes Analysis of 1022 Palliative Procedures for Advanced Cancer. Ann Surg 2004;240:719-26; discussion 726-7. [PubMed]
- Krouse RS, Nelson RA, Farrell BR, et al. Surgical Palliation at a Cancer Center. Arch Surg 2001;136:773-8. [Crossref] [PubMed]
- Badgwell BD, Smith K, Liu P, et al. Indicators of surgery and survival in oncology inpatients requiring surgical evaluation for palliation. Support Care Cancer 2009;17:727-34. [Crossref] [PubMed]
- Tseng WH, Yang X, Wang H, et al. Nomogram to Predict Risk of 30-Day Morbidity and Mortality for Patients With Disseminated Malignancy Undergoing Surgical Intervention. Ann Surg 2011;254:333-8. [Crossref] [PubMed]
- Francescutti V, Miller A, Satchidanand Y, et al. Management of Bowel Obstruction in Patients with Stage IV Cancer: Predictors of Outcome After Surgery. Ann Surg Oncol 2013;20:707-14. [Crossref] [PubMed]
- Miner TJ, Cohen J, Charpentier K, et al. The Palliative Triangle. Arch Surg 2011;146:517-22. [Crossref] [PubMed]
- Pope C, Mays N. Qualitative Research: Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995;311:42-5. [Crossref] [PubMed]
- Cho JY, Lee EH. Reducing Confusion about Grounded Theory and Qualitative Content Analysis: Similarities and Differences. The Qualitative Report 2014;19:1-20.
- Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107-15. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of Surgical Complications. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Dunn GP, Martensen R, Weissman D. Surgical Palliative Care: A Resident’s Guide. Chicago, IL: 2009.
- McCahill LE, Krouse RS, Chu DZ, et al. Decision Making in Palliative Surgery. J Am Coll Surg 2002;195:411-22. [Crossref] [PubMed]
- Chi DS, Phaeton R, Miner TJ, et al. A Prospective Outcomes Analysis of Palliative Procedures Performed for Malignant Intestinal Obstruction Due to Recurrent Ovarian Cancer. Oncologist 2009;14:835-9. [PubMed]
- Fujitani K, Yamada M, Hirao M, et al. Optimal indications of surgical palliation for incurable advanced gastric cancer presenting with malignant gastrointestinal obstruction. Gastric Cancer 2011;14:353-9. [Crossref] [PubMed]
- Miner TJ, Jaques DP, Shriver CD. A prospective evaluation of patients undergoing surgery for the palliation of an advanced malignancy. Ann Surg Oncol 2002;9:696-703. [Crossref] [PubMed]
- Wallen GR, Baker K, Stolar M, et al. Palliative care outcomes in surgical oncology patients with advanced malignancies: a mixed methods approach. Qual Life Res 2012;21:405-15. [Crossref] [PubMed]
- Gibbins J, Bhatia R, Forbes K, et al. What do patients with advanced incurable cancer want from the management of their pain? A qualitative study. Palliative Medicine 2014;28:71-8. [Crossref] [PubMed]
- Weeks JC, Cook EF, O'Day SJ, et al. Relationship Between Cancer Patients’ Predictions of Prognosis and Their Treatment Preferences. JAMA 1998;279:1709-14. [Crossref] [PubMed]
- Weeks JC, Catalano PJ, Cronin A, et al. Patients' Expectations about Effects of Chemotherapy for Advanced Cancer. N Engl J Med 2012;367:1616-25. [Crossref] [PubMed]
- Gattellari M, Voigt KJ, Butow PN, et al. When the Treatment Goal Is Not Cure: Are Cancer Patients Equipped to Make Informed Decisions? J Clin Oncol 2002;20:503-13. [Crossref] [PubMed]
- Winner M, Mooney SJ, Hershman DL, et al. Management and Outcomes of Bowel Obstruction in Patients with Stage IV Colon Cancer. Dis Colon Rectum 2013;56:834-43. [Crossref] [PubMed]
- Guest G, Bunce A, Johnson L. How Many Interviews Are Enough?: An Experiment with Data Saturation and Variability. Field Methods 2006;18:59-82. [Crossref]
- van Vliet LM, Epstein AS. Current State of the Art and Science of Patient- Clinician Communication in Progressive Disease: Patients’ Need to Know and Need to Feel Known. J Clin Oncol 2014;32:3474-8. [Crossref] [PubMed]