
Effects of social support, anxiety, and hope levels on cognitive bias in patients with nasogastric/nasoenteric tubes
Highlight box
Key findings
• Social support, anxiety, and hope influence cognitive bias in patients with nasogastric/nasoenteric tubes.
What is known and what is new?
• Cognitive bias may lead to unplanned extubation in conscious patients with nasogastric/nasoenteric tubes.
• Social support significantly affects cognitive bias in patients with nasogastric/nasoenteric tubes. Anxiety and hope play a mediating role in social support and cognitive bias.
What is the implication, and what should change now?
• Positive psychological intervention and obtention of support could improve the cognitive bias of patients with nasogastric/nasoenteric tubes.
Introduction
Unplanned extubation of inpatients is a common adverse nursing event (1). The incidence of unplanned extubation of a nasogastric/nasoenteric tubes is high (2), which can lead to prolonged hospital stays, increased treatment costs, cause pain for the patient, adversely affect the family, and even cause medical and nursing disputes (3-5). The influencing factors of unplanned extubation are various, and cognitive bias is one of them. A cognitive bias is a systematic error in thinking that impacts one’s choices and judgments (6,7). In the medical setting, patients’ cognitive bias may lead to unplanned extubation of nasogastric/nasoenteric tubes. To prevent this from happening, it is of great significance to understand and identify the factors influencing cognitive bias in patients with nasogastric/nasoenteric tubes.
According to previous studies by other groups, the levels of social support, anxiety, and hope are important factors that affect cognitive bias (8-10), but whether these factors have the same effect on cognitive bias in patients with nasogastric/nasoenteric tubes remains unclear. At present, few studies have focused on the mechanisms whereby social support, anxiety, and hope level influence patients’ cognitive bias. Therefore, the aims of this study were to (I) investigate associations between cognitive bias, social support, anxiety, and hope level; (II) analyze the impact path and degree of social support, anxiety, and hope level on cognitive bias. We hoped to provide a valuable reference for improving catheter safety for patients with nasogastric/nasoenteric tubes. We present this article in accordance with the SURGE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-932/rc).
Methods
Research participants
Patients with nasogastric/nasoenteric tubes from 16 hospitals in Suzhou from December 2019 to March 2022 were selected as the research cohort using convenience sampling method. In this study, a total of 453 questionnaires were sent out, and 438 were received with an effective recovery rate of 96.69%. Questionnaires were distributed on the spot; the researcher instructed the patients to complete the questionnaires and was responsible for collecting them. The researchers read the items of the questionnaires to the patients with handwriting difficulties and then completed the questionnaire on behalf of the patients who dictated their responses. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of The First Affiliated Hospital of Soochow University (Approval No. [2020]131) and informed consent was provided by all participants.
The inclusion criteria were as follows: (I) age ≥18 years; (II) stable condition with clear consciousness, decision-making, and behavioral abilities; (III) nasogastric/nasoenteric tubes for more than 1 day; (IV) ability to complete the questionnaire independently or with the help of the researcher; (V) willingness to voluntarily participate in the study and sign the informed consent.
The exclusion criteria were as follows: (I) language communication barriers; (II) history of mental disorders.
Measures
Participant characteristics
A self-developed general data questionnaire was used to collect the participant characteristics, including the following: (I) demographic data in which gender, age, education level, medical insurance, living style, marital status, religious belief, health care, and monthly household income per capita (yuan) were included; (II) disease-related data in which disease type, sleep (hours/day), combined chronic disease, and protective restraint were included.
Cognitive bias
The cognitive bias of patients with nasogastric/nasoenteric tubes was assessed using a self-developed questionnaire named the Cognitive Bias Questionnaire for Patients with Nasogastric/nasoenteric Tubes which was developed based on qualitative research methods, the Delphi expert enquiry, and group discussions. The questionnaire included 5 dimensions (representative bias, overconfidence, attributional bias, loss aversion, and cognitive compliance) and each dimension included 3 items for a total of 15 items. The questionnaire was rated on a 5-point Likert scale (1-stronly disagree and 5-strongly agree). Scores ranged from 15 to 75 with a higher score relating to greater level cognitive bias. In this study, the questionnaire demonstrated good reliability, with Cronbach’s alpha equal to 0.884 and ranging from 0.774 to 0.894 for each of the 5 dimensions.
Anxiety
Generalized Anxiety Disorder 7 (GAD-7) was used to evaluate the anxiety level of patients with nasogastric/nasoenteric tubes. The scale was developed by Spitzer et al. (11) in 2006. GAD-7 was used to measure the anxiety experienced by patients in the last 2 weeks. The scale includes 7 items, which are scored using a 4-point Likert method. Scores ranged from 7 to 28 with a higher score relating to greater level anxiety. In this study, the scale demonstrated good reliability with Cronbach’s alpha of 0.882.
Social support
The Perceived Social Support Scale (PSSS) was used to evaluate the level of social support of patients with nasogastric/nasoenteric tubes. The scale was developed by Zimet et al. (12). The scale includes 3 dimensions which are named friend support, family support, and other support, with a total of 12 items. The scale is scored by Likert 7-grade scoring method, from “strongly disagree” to “strongly agree” as “1–7 points”, and the sum of each item is the total score, with a higher total score indicating higher levels of social support perceived by individuals. The Cronbach’s alpha of the aggregate table in this study was 0.927.
Hope
The Herth Hope Index (HHI), developed by Herth (13), was used to evaluate the level of hope in patients with nasogastric/nasoenteric tubes. The scale includes 3 dimensions, defined as positive attitude, positive action, and intimate relationship, with a total of 12 items. A 4-point Likert scoring method is adopted (1-strongly disagree and 4-strongly agree). Items 3 and 6 require reverse scoring. Scores ranged from 12 to 48 with a higher score indicating a greater hope level. The Cronbach’s alpha of the scale in this study was 0.887.
Statistical analysis
Epidata 3.1 software (The EpiData Association, Odense, Denmark) was used for data entry, and SPSS 25.0 (IBM Corp., Armonk, NY, USA) and AMOS 22.0 software (IBM Corp.) were used for data analysis. Measurement data were expressed as mean ± standard deviation (mean ± SD). Comparisons of the cognitive bias scores among participants were analyzed by t-test or analysis of variance (ANOVA) test. Pearson correlation analysis was used to explore the relationship between social support, hope, and anxiety and cognitive bias. AMOS 22.0 software was used to establish the structural equation model of the relationship among social support, hope, and anxiety and cognitive bias. Mediating roles of hope and anxiety levels in social support and cognitive bias was performed by Bootstrap method. A P value of <0.05 (2-sided) was considered statistically significant.
Results
Participant characteristics
A total of 438 patients with nasogastric/nasoenteric tubes aged 62.92±11.82 years were investigated in this study. Participant characteristics are presented in Table 1.
Table 1
| Variables | Classification | Cases (%) | Cognitive bias score, mean ± SD | t/F | P value |
|---|---|---|---|---|---|
| Gender | Male | 298 (68.0) | 42.29±9.26 | 0.687 | 0.492 |
| Female | 140 (32.0) | 41.85±8.71 | |||
| Age (years) | ≤40 | 34 (7.8) | 40.41±6.45 | 3.431 | 0.033 |
| 41–60 | 102 (23.3) | 40.67±8.70 | |||
| ≥61 | 302 (68.9) | 43.05±9.36 | |||
| Disease type | Not cancer | 239 (54.6) | 41.20±9.15 | −2.770 | 0.006 |
| Cancer | 199 (45.4) | 43.59±8.85 | |||
| Education level | Primary school and below | 226 (51.6) | 43.37±9.57 | 2.594 | 0.052 |
| Junior high school | 120 (27.4) | 41.57±9.41 | |||
| High school/technical secondary school | 52 (11.9) | 41.19±6.41 | |||
| College/university or above | 40 (9.1) | 39.80±7.50 | |||
| Religious belief | No | 430 (98.2) | 42.28±9.12 | −0.107 | 0.915 |
| Yes | 8 (1.8) | 42.63±6.99 | |||
| Marital status | Divorced/death of a spouse/unmarried | 39 (8.9) | 41.90±9.82 | −0.279 | 0.780 |
| Married | 399 (91.1) | 42.32±9.02 | |||
| Living situation | Living alone | 16 (3.7) | 42.13±9.10 | −0.072 | 0.943 |
| Not living alone | 422 (96.3) | 42.29±9.09 | |||
| Health care | No | 21 (4.8) | 43.29±8.47 | −0.517 | 0.606 |
| Yes | 417 (95.2) | 42.24±9.12 | |||
| Monthly household income per capita (yuan) | <3,000 | 73 (16.7) | 40.67±8.91 | 2.332 | 0.098 |
| 3,000–8,000 | 326 (74.4) | 42.38±8.96 | |||
| >8,000 | 39 (8.9) | 44.49±10.04 | |||
| Sleep (hours/day) | <5 | 234 (53.4) | 43.19±9.15 | 3.229 | 0.041 |
| 5–7 | 75 (17.1) | 42.23±10.01 | |||
| >7 | 129 (29.5) | 40.67±8.09 | |||
| Combined chronic disease | No | 303 (69.2) | 42.26±9.28 | 0.074 | 0.941 |
| Yes | 135 (30.8) | 42.33±8.67 | |||
| Protective constraint | No | 198 (45.2) | 43.20±9.12 | 1.935 | 0.054 |
| Yes | 240 (54.8) | 41.52±9.00 |
SD, standard deviation.
Current status of patients’ social support, anxiety, and hope levels and cognitive bias
In order to explore the current situation of patients’ social support, anxiety, and hope and cognitive bias, we evaluated the levels of social support, anxiety, and hope and cognitive bias among all participants. As shown in Table 2, the PSSS score of patients with nasogastric/nasoenteric tubes was (66.20±7.26), GAD-7 score was (4.88±3.54), hope score was (36.04±4.57), and cognitive bias score was (42.29±9.08).
Table 2
| Variable | Number of items | Total score (points), mean ± SD | Average score on the items (points), mean ± SD |
|---|---|---|---|
| Social support | 12 | 66.20±7.26 | 5.52±0.61 |
| Anxiety | 7 | 4.88±3.54 | 0.70±0.51 |
| Hope | 12 | 36.04±4.57 | 3.00±0.38 |
| Cognitive bias | 15 | 42.29±9.08 | 2.82±0.61 |
SD, standard deviation.
Correlation analysis of cognitive bias with anxiety, social support, and hope levels
To evaluate the strength of linearity between anxiety, social support, and hope and cognitive bias, we performed Pearson correlation analysis among the 4 variables. Results of Pearson correlation analysis showed that social support was negatively correlated with anxiety and cognitive bias in patients with nasogastric/nasoenteric tubes. Social support was positively correlated with hope level, and anxiety was positively correlated with cognitive bias (P<0.01). Hope level was negatively correlated with cognitive bias (P<0.01) (Table 3). These results met the premise of mediating effect test.
Table 3
| Variable | Social support | Anxiety | Hope | Cognitive bias |
|---|---|---|---|---|
| Social support | 1.000 | −0.270* | 0.425* | −0.395* |
| Anxiety | – | 1.000 | −0.246* | 0.446* |
| Hope | – | – | 1.000 | −0.427* |
| Cognitive bias | – | – | – | 1.000 |
*, 2-sided test, P<0.01.
Pathway analysis of cognitive bias, anxiety, social support, and hope levels
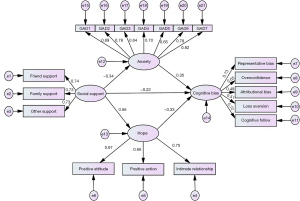
To analyze the impact path and extent of social support, anxiety, and hope level on patients’ cognitive bias, we performed pathway analysis. Based on this study and the results of previous studies, a hypothesis model was established with social support as an independent variable, anxiety and hope level as mediating variables, and cognitive bias as the dependent variable. The fitting of model data showed that the chi-square degree of freedom ratio was 1.521, the goodness of fit index (GFI) was 0.954, the adjusted goodness of fit index (AGFI) was 0.940, the comparative fit indices (CFI) was 0.976, and the root-mean-square error of approximation (RMSEA) was 0.035. The above data showed that the model is suitable for pathway analysis. Furthermore, the pathway coefficients of the model were statistically significant (P<0.05), indicating that the model was valid.
The mediating effect test results showed that anxiety had a direct positive effect on cognitive bias, and the standardized estimated value of its pathway coefficient was 0.35 (P<0.001). Hope had a direct negative effect on cognitive bias, and the standardized estimate of its pathway coefficient was −0.33 (P<0.001). Social support had a direct negative effect on cognitive bias and an indirect effect on cognitive bias through anxiety and hope levels. The standardized estimated values of the pathway coefficients were −0.22, −0.12, and −0.19 (P<0.001), for social support, anxiety, and hope, respectively (Table 4). The model of the relationships among social support, anxiety, and hope levels and cognitive bias in patients with nasogastric/nasoenteric tubes is shown in Figure 1. The population model explained 46.2% of the variation in cognitive bias.
Table 4
| Relationship between variables | Path | Effect value | 95% CI |
|---|---|---|---|
| Direct relationship | Social support → cognitive bias | −0.22 | −0.364 to −0.065 |
| Indirect relationship | Social support → anxiety → cognitive bias | −0.12 | −0.179 to −0.073 |
| Social support → hope → cognitive bias | −0.19 | −0.303 to −0.108 |
CI, confidence interval
Discussion
Impact of participant characteristics on cognitive bias
The results in our present study showed that the average cognitive bias score of patients with nasogastric/nasoenteric tubes was 2.82±0.61 points, which reflects a moderate level. The results of this study also showed that compared with young people, elderly patients were more prone to cognitive bias in the process of receiving new information (14). This study also showed that cancer patients had more cognitive bias. Studies have found that cancer patients experience changes in cognitive functions during or after treatment, such as memory function, thought process, attention, and executive function (15,16). A cross-sectional study by Bilenduke et al. (17) showed that breast cancer patients undergoing chemotherapy had higher cognitive function injury and a high incidence of depressive symptoms compared with healthy controls, suggesting that both cancer itself and its treatment may affect the cognitive function and emotional changes of the patients. Studies have also shown that many patients with advanced cancer are affected by cognitive biases that may be exacerbated by increased levels of hope (18). Besides, the quality of sleep quality was identified as an important factor affecting patients’ cognitive bias, which aligned with previous research results (19,20). Studies also have found that acute sleep deprivation can cause individuals to fall into a state of insufficient cognitive resources (21).
The influence of anxiety on cognitive bias of patients with nasogastric/nasoenteric tubes
The results of this study showed that the anxiety of patients with nasogastric/nasoenteric tubes had a direct positive impact on their cognitive bias, and the effect value was 0.35. Gerlach et al. (22) and Sherman et al. (23) also found that an individual’s anxiety level was significantly positively correlated with cognitive bias. This finding indicates that the greater the patient’s anxiety, the more serious the cognitive bias. This finding may be attributed to the fact that patients with anxiety will selectively pay attention to the negative aspects of stress events, perceive more dangers, and use them to evaluate and predict the developmental trajectory of events (24). Therefore, patients can make irrational or illogical inferences about the outcome of the stressful event, thus, cognitive bias occurs. Bahcivan et al. (25) found that mindfulness training can effectively relieve individual anxiety. It has been suggested to implement mindfulness-based intervention training with blended aromatherapy using lavender and damask rose oil at the same time in patients with nasogastric intubation to reduce the patients’ anxiety symptoms (26), thereby reducing the patients’ cognitive bias. Anxiety will affect the patient’s behavior, and peer support will ease the patient’s anxiety. Encourage patients to talk about their feelings about catheterization, invite individuals who have had good compliance and recovery of nasogastric/nasoenteric tubes to share their experience, and give encouragement to patients’ partners to facilitate acceptance of the nasogastric/nasoenteric tubes (27).
The influence of hope level on cognitive bias of patients with nasogastric/nasoenteric tubes
The results of this study showed that the patients’ hope level was significantly negatively correlated with their cognitive bias, and the patients’ hope level had a direct impact on their cognitive bias with effect value of −0.33. Thus, in the face of the stressful event of nasogastric/nasoenteric tubes, the lower the level of hope, the more severe the cognitive deviation. Hope is an effective coping strategy. Studies have shown that hope can help patients with actively facing diseases and uncomfortable treatments under uncertain and painful conditions (28-30), and encourage them to continuously educate themselves about their diseases and corresponding treatments to correct their cognitive bias. Studies have found that hope therapy (31,32) and the focused solution model (33) can improve patients’ hope level. Therefore, medical staff can use hope therapy for psychological intervention of patients, instill hope, and set up expected goals in patients, promote patients’ courage to overcome the disease, or use the focused solution model to intervene to maximize the enthusiasm and initiative of patients to improve their hope level.
The influence of social support on cognitive bias of patients with nasogastric/nasoenteric tubes
This study also found that the level of social support in patients with nasogastric/nasoenteric tubes had a direct or indirect effect on their cognitive bias, and the total effect value was 0.53. If the patient does not perceive being cared for or supported by others and the perceived social support cannot meet their needs, they will look at the problem in a negative manner when facing a stressful event (34,35), resulting in cognitive bias. Medical staff can improve the patient’s perception of social support by holding health lectures and meetings with other patients to correct patients’ cognitive bias (36). However, it should be noted that inappropriate social support not only fails to provide assistance to patients but also makes patients feel as if they are a burden. Excessive support and protection of patients can make patients feel that they are not understood, and they are often unwilling to accept or even reject such support (37,38). Therefore, when conducting social support interventions for patients with nasogastric/nasoenteric tubes, we should first assess the needs of patients, clarify the types of social support that patients need, and consider their social and cultural background to provide them with more effective social support. In addition, some patients with nasogastric/nasoenteric tubes require long-term catheterization. How to provide patients with effective, continuous, and dynamic social support in different periods of disease is worthy of in-depth discussion.
We also found that social support can indirectly affect cognitive bias through anxiety and hope level. Good social support could effectively relieve psychological pressure to a certain extent, reduce the adverse mood caused by stress events, and improve the symptoms of anxiety. These results were consistent with previous studies: Li et al. (39) and Kaya et al. (40) found that the level of perceived social support was related to anxiety symptoms. Patients with more social support would receive more help when facing various stress situations and can easily regain confidence with the help of family members and friends, thus alleviating patients’ fear of catheterization and improving their hope levels (41-43). Therefore, nursing staff should strengthen the support for the patients. In addition, the patients’ family members of patients should be completely aware of the effects of family social support on patients’ negative emotions, such as anxiety, hope level and cognitive bias. Simultaneously, patients should be encouraged to believe in their own abilities, conduct self-care management, actively cooperate with treatments, seek correct and effective social support, and improve their utilization of social support, and then improve their cognitive bias.
The results of this study also showed that social support, anxiety, and hope level could jointly explain the 46.2% variation in cognitive bias in patients, indicating that the generation of cognitive bias is complex and affected by other factors, which requires further exploration and research.
Limitations
This study had regional limitations, and the relationship among social support, anxiety, and hope level and cognitive bias of patients in hospitals in different regions still needs to be further studied. Meanwhile, it did not involve longer-term enteral/gastric tube feeding versus daytime use, which will be the direction of our future research. In conclusion, giving full play to the role of medical and social support system and providing more physical, mental, and social support to patients could improve the psychological state of patients and thus improve their cognitive bias.
Conclusions
In this study, we found that the anxiety and hope levels of patients with nasogastric/nasoenteric tubes directly affect their cognitive bias, and that social support can directly or indirectly affect the cognitive bias of patients through regulation of the anxiety and hope levels. Improving the level of social support and hope and reducing anxiety levels for patients with nasogastric/nasoenteric tubes is of great significance to improving patients’ cognitive bias. Nursing staff should regularly assess the anxiety and hope levels of these patients, and mobilize resources from all aspects of society to improve their level of social support.
Acknowledgments
Funding: This work was supported by the grant from Science and Technology Project of Suzhou (No. sys2018036).
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-932/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-932/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-932/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-932/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of The First Affiliated Hospital of Soochow University (Approval No. [2020]131) and informed consent was provided by all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nair V, Smith H. Phased Quality Improvement Interventions in Reducing Unplanned Extubation in the Neonatal ICU. Respir Care 2020;65:1511-8. [Crossref] [PubMed]
- Galazzi A, Adamini I, Consonni D, et al. Accidental removal of devices in intensive care unit: An eight-year observational study. Intensive Crit Care Nurs 2019;54:34-8. [Crossref] [PubMed]
- Lucas da Silva PS, Fonseca MCM. Incidence and Risk Factors for Cardiovascular Collapse After Unplanned Extubations in the Pediatric ICU. Respir Care 2017;62:896-903. [Crossref] [PubMed]
- Li CM, Ho YR, Chen WL, et al. Nasogastric Tube Dislodgment Detection in Rehabilitation Patients Based on Fog Computing with Warning Sensors and Fuzzy Petri Net. Sensor Mater 2019;31:117-30. [Crossref]
- Li P, Sun Z, Xu J. Unplanned extubation among critically ill adults: A systematic review and meta-analysis. Intensive Crit Care Nurs 2022;70:103219. [Crossref] [PubMed]
- Edwards DJ. Ensuring Effective Public Health Communication: Insights and Modeling Efforts From Theories of Behavioral Economics, Heuristics, and Behavioral Analysis for Decision Making Under Risk. Front Psychol 2021;12:715159. [Crossref] [PubMed]
- Gheondea-Eladi A. Patient decision aids: a content analysis based on a decision tree structure. BMC Med Inform Decis Mak 2019;19:137. [Crossref] [PubMed]
- Songco A, Booth C, Spiegler O, et al. Anxiety and Depressive Symptom Trajectories in Adolescence and the Co-Occurring Development of Cognitive Biases: Evidence from the CogBIAS Longitudinal Study. J Abnorm Child Psychol 2020;48:1617-33. [Crossref] [PubMed]
- Meldgaard J, Jespersen LN, Andersen TH, et al. Exploring protective factors through positive psychology and salutogenesis in Danish families with type 2 diabetes. Health Promot Int 2022;37:daab156. [Crossref] [PubMed]
- Smith EM, Reynolds S, Orchard F, et al. Cognitive biases predict symptoms of depression, anxiety and wellbeing above and beyond neuroticism in adolescence. J Affect Disord 2018;241:446-53. [Crossref] [PubMed]
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. [Crossref] [PubMed]
- Zimet GD, Powell SS, Farley GK, et al. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess 1990;55:610-7. [Crossref] [PubMed]
- Herth K. Abbreviated instrument to measure hope: development and psychometric evaluation. J Adv Nurs 1992;17:1251-9. [Crossref] [PubMed]
- Krok-Schoen JL, Palmer-Wackerly AL, Dailey PM, et al. Age Differences in Cancer Treatment Decision Making and Social Support. J Aging Health 2017;29:187-205. [Crossref] [PubMed]
- Lange M, Joly F, Vardy J, et al. Cancer-related cognitive impairment: an update on state of the art, detection, and management strategies in cancer survivors. Ann Oncol 2019;30:1925-40. [Crossref] [PubMed]
- Karschnia P, Parsons MW, Dietrich J. Pharmacologic management of cognitive impairment induced by cancer therapy. Lancet Oncol 2019;20:e92-e102. [Crossref] [PubMed]
- Bilenduke E, Sterrett JD, Ranby KW, et al. Impacts of breast cancer and chemotherapy on gut microbiome, cognitive functioning, and mood relative to healthy controls. Sci Rep 2022;12:19547. [Crossref] [PubMed]
- Finkelstein EA, Baid D, Cheung YB, et al. Hope, bias and survival expectations of advanced cancer patients: A cross-sectional study. Psychooncology 2021;30:780-8. [Crossref] [PubMed]
- Ochab JK, Szwed J, Oleś K, et al. Observing changes in human functioning during induced sleep deficiency and recovery periods. PLoS One 2021;16:e0255771. [Crossref] [PubMed]
- Short MA, Chee MWL. Adolescent sleep restriction effects on cognition and mood. Prog Brain Res 2019;246:55-71. [Crossref] [PubMed]
- Hudson AN, Van Dongen HPA, Honn KA. Sleep deprivation, vigilant attention, and brain function: a review. Neuropsychopharmacology 2020;45:21-30. [Crossref] [PubMed]
- Gerlach F, Ehring T, Werner GG, et al. Insomnia-related interpretational bias is associated with pre-sleep worry. J Sleep Res 2020;29:e12938. [Crossref] [PubMed]
- Sherman JA, Ehrenreich-May J. Ethnicity’s Role in the Relationship Between Anxiety and Negative Interpretation Bias Among Clinically Anxious Youth: A Pilot Study. Child Psychiatry Hum Dev 2018;49:396-408. [PubMed]
- Gay MC, Bungener C, Thomas S, et al. Anxiety, emotional processing and depression in people with multiple sclerosis. BMC Neurol 2017;17:43. [Crossref] [PubMed]
- Bahcivan O, Estapé T, Gutierrez-Maldonado J. Efficacy of New Mindfulness-Based Swinging Technique Intervention: A Pilot Randomised Controlled Trial Among Women With Breast Cancer. Front Psychol 2022;13:863857. [Crossref] [PubMed]
- Hashemi N, Nazari F, Faghih A, et al. Effects of blended aromatherapy using lavender and damask rose oils on the test anxiety of nursing students. J Educ Health Promot 2021;10:349. [Crossref] [PubMed]
- Ebrahimi H, Abbasi A, Bagheri H, et al. The role of peer support education model on the quality of life and self-care behaviors of patients with myocardial infarction. Patient Educ Couns 2021;104:130-5. [Crossref] [PubMed]
- Costa DT, Silva DMRD, Cavalcanti IDL, et al. Religious/spiritual coping and level of hope in patients with cancer in chemotherapy. Rev Bras Enferm 2019;72:640-5. [Crossref] [PubMed]
- Sajadi SA, Farsi Z, Akbari R, et al. Investigating the relationship between quality of life and hope in family caregivers of hemodialysis patients and related factors. BMC Nephrol 2021;22:383. [Crossref] [PubMed]
- Bareket-Bojmel L, Shahar G, Abu-Kaf S, et al. Perceived social support, loneliness, and hope during the COVID-19 Pandemic: Testing a mediating model in the UK, USA, and Israel. Br J Clin Psychol 2021;60:133-48. [Crossref] [PubMed]
- Sadeghi H, Ebrahimi L, Vatandoust L. Effectiveness of Hope Therapy Protocol on Depression and Hope in Amphetamine Users. Int J High Risk Behav Addict 2015;4:e21905. [Crossref] [PubMed]
- Esfahani NN, Talakoub S, Jafari-Mianaei S, et al. Effect of group hope therapy on self-efficacy of adolescents with type 1 diabetes. Rev Assoc Med Bras (1992) 2021;67:1816-20. [PubMed]
- Zhang A, Ji Q, Currin-McCulloch J, et al. The effectiveness of solution-focused brief therapy for psychological distress among Chinese parents of children with a cancer diagnosis: a pilot randomized controlled trial. Support Care Cancer 2018;26:2901-10. [Crossref] [PubMed]
- Joyce J, Ryan J, Owen A, et al. Social isolation, social support, and loneliness and their relationship with cognitive health and dementia. Int J Geriatr Psychiatry 2021; Epub ahead of print. [Crossref] [PubMed]
- Abdoli N, Salari N, Darvishi N, et al. The global prevalence of major depressive disorder (MDD) among the elderly: A systematic review and meta-analysis. Neurosci Biobehav Rev 2022;132:1067-73. [Crossref] [PubMed]
- Li X, Wang B, Tan D, et al. Effectiveness of comprehensive social support interventions among elderly patients with tuberculosis in communities in China: a community-based trial. J Epidemiol Community Health 2018;72:369-75. [Crossref] [PubMed]
- Eadie T, Kapsner-Smith M, Bolt S, et al. Relationship between perceived social support and patient-reported communication outcomes across communication disorders: a systematic review. Int J Lang Commun Disord 2018;53:1059-77. [Crossref] [PubMed]
- Fischbeck S, Weyer-Elberich V, Zeissig SR, et al. Determinants of illness-specific social support and its relation to distress in long-term melanoma survivors. BMC Public Health 2018;18:511. [Crossref] [PubMed]
- Li Y, Peng J. Does social support matter? The mediating links with coping strategy and anxiety among Chinese college students in a cross-sectional study of COVID-19 pandemic. BMC Public Health 2021;21:1298. [Crossref] [PubMed]
- Kaya H, Ayık B, Tasdelen R, et al. Social Support Promotes Mental Health During the COVID-19 Outbreak: A Cross-Sectional Study from Turkey. Psychiatr Danub 2021;33:217-24. [Crossref] [PubMed]
- Bao Y, Li L, Guan Y, et al. Is the relationship between social support and depressive symptoms mediated by hope among Chinese central nervous system tumor patients? Support Care Cancer 2019;27:257-63. [Crossref] [PubMed]
- Liu C, Zhang Y, Jiang H, et al. Association between social support and post-traumatic stress disorder symptoms among Chinese patients with ovarian cancer: A multiple mediation model. PLoS One 2017;12:e0177055. [Crossref] [PubMed]
- Hu CW, Chang KH, Hsish HC, et al. Social Support as a Mediator of the Relationship between Hope and Decisional Conflict in Patients Deciding Whether to Receive Dialysis. J Healthc Eng 2021;2021:5607219. [Crossref] [PubMed]
(English Language Editor: J. Jones)


