
Balloon kyphoplasty combined with percutaneous pedicle screw (PPS) for the treatment of osteoporotic thoracolumbar fractures has minimum correction loss 2 years after surgery: compared to vertebroplasty using hydroxyapatite block combined with PPS
Highlight box
Key findings
• Balloon kyphoplasty combined with percutaneous pedicle screw (BKP + PPS) for the treatment of osteoporotic thoracolumbar fractures (TLOVF), is minimally invasive, and has minimum correction loss 2 years after surgery.
What is known and what is new?
• BKP + PPS was shown to be an effective treatment for TLOVF, and has advantages such as less blood loss, short operation time, and rapid recovery.
• The purpose of this study was to compare the clinical outcomes of two different surgical procedures, BKP + PPS and HAVP + PPS, by the same surgeon for TLOVF in elderly patients more than 2 years postoperatively.
What is the implication, and what should change now?
• The limitations of this study are that the postoperative follow-up period is short and its retrospective nature. Long term follow-up and studies of larger sample size are needed to determine the value of the proposed method.
Introduction
Therapeutic strategies are widely different for the management of osteoporotic vertebral body fractures. Conservative therapy is the first choice unless there is nerve palsy for the fresh cases of osteoporotic vertebral fractures (OVF). Bed rest during the acute phase of OVF can prevent the progression of vertebral body collapse (1). However, disuse syndrome and dementia caused by long-term bed rest in the elderly have been pointed out, and early leaving of bed and discharge from hospital have been encouraged. As a result, in recent years, the number of cases is increasing in which a relatively simple ready-made orthosis is worn to get out of bed early.
On the other hand, despite conservative therapy, the onset of vertebral non-union, the residual pain, and spinal deformity due to the progress of vertebral body collapse, and the delayed paralysis may occur. The presence of an intravertebral cleft and instability of the affected vertebra represent risk factors for vertebral collapse with neurological deficit, requiring careful observation (2).
The ideal treatment for OVF is early demobilization and healing without vertebral body collapse and progressive kyphosis.
Katsumi et al. (3) reported the clinical outcomes and limitations after vertebroplasty with posterior open spinal fusion (VP + PSF) without neural decompression for osteoporotic vertebral collapse. In that report, short-segment open VP + PSF can achieve a high union rate of collapsed vertebra and provide a significant improvement in back pain or neurological status with less invasive surgery, but has a limit of kyphosis correction.
Balloon kyphoplasty (BKP) is an extremely useful treatment commonly performed in patients with painful OVFs, with its efficacy and safety having previously been reported (4). However, in cases with large intra-vertebral clefts and cases with posterior spinal tissue damage, adjacent vertebral body fractures (AVFs), and cement migration may occur early after BKP, which may be a factor for poor results. Major complications of BKP occur in <1% of patients treated for OVFs (5).
Minamide et al. (6) reported that a series of BKP for painful OVFs within 4 weeks after injury and 4 weeks after injury, low back pain score, better alignment, and lower risk of AVF obtained by performing BKP earlier than 4 weeks after injury. However, there is currently no indication of BKP generally at the early stage of painful OVF in our country.
Revision surgery after BKP is relatively rare. Takahashi et al. (7) reported that a split type fracture, angular motion ≥14° and large endplate deficit (>3 mm) are risk factors for revision surgery after BKP. Nakamae et al. (8) reported that cement loosening in PVP was associated with intra-vertebral instability, Parkinson’s disease, spinous process fracture, and split type fracture. In our opinion, these Risk factors are also considered to match the case of BKP.
The incidence of AVF is relatively high, ranging from 11% to 29% after BKP (9,10). Bone metabolism and 25 (OH) D levels seem to play a role in the occurrence of post-kyphoplasty recurrent vertebral compression fractures (11). Severe wedge angle before BKP, correction degree, old OVF presence, and thoracolumbar level were predictive factors for AVF after BKP (9).
There is a report that treatment of OVF with BKP and percutaneous pedicle screw (PPS) combined alleviated the decrease in kyphosis and vertebral body height 2 years after surgery (12).
In this study, we report the clinical results of BKP and PPS simultaneously (BKP + PPS) for painful TLOVF (TLOVF) and compare it with our percutaneous previous vertebroplasty with hydroxyapatite (HA) block + PPS (HAVP + PPS). We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1024/rc).
Methods
The protocol for this study was reviewed and approved by the ethics committee of our institution named—“Funabashi orthopaedic hospital ethics committee”; approval number: 2019036; approval date: 2019.09.26. Individual consent for this retrospective analysis was waived. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). From May 2013 to June 2020, out of 39 cases (8 males, 31 females, average age at surgery 76.6 years) who performed VP and posterior fixation with PPS by the same operator for painful TLOVF (T11 to L2), the subjects were 28 patients (2 males, 26 females, mean age at surgery 77.3 years) who could be followed up more than 2 years after surgery.
The surgical procedure is PVP for 1 vertebral body and posterior stabilization with PPS (without decompression) for painful TLOVF. We divided these into 14 cases of HAVP + PPS (group H) and 14 cases of BKP + PPS (group B) according to the operation timing and investigated the clinical results.
The indications for surgery are as follows: (I) burst fracture with posterior wall injury of vertebral body without neurological symptoms (not indicated for BKP alone), (II) the presence of posterior spinal supportive tissue (spinous process and/or posterior ligamentous complex; PLC) injury, (III) diffuse idiopathic skeletal hyperostosis (DISH) case, (IV) standing or sitting lateral radiograph, vertebral body wedge ratio (anterior/posterior wall) 30% or more, (V) large vertebral body cleft [with magnetic resonance imaging (MRI) T2-weighted image showing fluid retention in vertebral body]. Out of these 5 items, the cases that satisfy two or more of them are surgically adapted cases.
Group H (HAVP + PPS) are cases from May 2013 to March 2017, and group B (BKP + PPS) are cases from July 2017 to June 2020. Since May 2017, the national medical insurance system has allowed the simultaneous use of BKP and spinal instrumentation. Hence we have adopted HAVP + PPS before April 2017 and BKP + PPS after May 2017 for cases with surgical indications. All patients underwent MRI and the lumbar spine bone mineral density (BMD) was measured by dual-energy X-ray absorptiometry (DXA). prior to surgery. Patient demographic, including age, gender, and BMD (% young adult mean; YAM) was shown in Table 1. We evaluated time from injury to surgery, pre- and post-operative visual analogue scale (VAS) of low back pain, wedging angle of fractured vertebra from X-ray photograph, duration of operation, intraoperative blood loss, number of instrumented vertebra, and length of stay at hospital. There was no significant difference in age, gender, BMD, time from injury to surgery, preoperative VAS of low back pain or preoperative wedging angle of fractured vertebra between groups H and B.
Table 1
| Clinical data | Group H (n=14) | Group B (n=14) | P value |
|---|---|---|---|
| Age (years) | 75.8±3.8 | 78.8±4.2 | 0.094 |
| Gender (female/male) | 13/1 | 13/1 | 1 |
| Bone mineral density (% young adult mean) | 67.3±8.1 | 69.9±8.4 | 0.216 |
| Fracture level | |||
| T11 | 0 | 2 | |
| T12 | 4 | 2 | |
| L1 | 9 | 6 | |
| L2 | 1 | 4 | |
| AO spine classification | |||
| B2 | 1 | 1 | |
| A3 | 10 | 9 | |
| A4 | 3 | 4 | |
| Time from injury to surgery (weeks) | 7.4±5.2 | 9.4±6.9 | 0.197 |
| Preoperative visual analogue scale | 7.8±0.9 | 8.2±1.1 | 0.137 |
| Preoperative wedging angle (degree) | 20.9±8.1 | 20.9±8.5 | 1 |
Group H, HAVP + PPS; Group B, BKP + PPS. Data are presented as number or mean ± standard deviation. HAVP, vertebroplasty with hydroxyapatite; PPS, percutaneous pedicle screw; BKP, balloon kyphoplasty.
Surgical procedure
Place the patient in the prone position on the hall frame, and confirm the pedicles of the fractured vertebral body and PPS-inserted vertebral body in the perspective antero-postero (AP) view, and design with a felt-tip pen on the skin. Then, the presence or absence of dynamic fracture mobility of the fractured vertebral body is confirmed by fluoroscopic lateral view. First, percutaneous vertebroplasty (PVP) is performed by a small skin incision, and then PPS is inserted. After making a 20-mm long vertical incision and opening the myofascia, PPS placement points were determined via finger navigation. The lateral side of facet joint, the intersection of lateral side of superior vertebral notch, and base point of transverse process were identified by the surgeon’s fingertip; then, the probe was out on the point after checking its shape. If the tip of probe was located at the lateral side of pedicle by checking with AP view of fluoroscopy, the probe could be inserted into the pedicle. Next, a cannulated probe or Jamshidi needle was used to make a screw hole for guide wire insertion (13). After guide wire insertion, PPS was implanted to the vertebra. Preoperative anteroposterior and lateral X-rays and computed tomography (CT) scans through the pedicles of the vertebral body to be instrumented are studied to determine the correct angle of entry in both the coronal and sagittal planes.
In group H, PVP and PPS-and-rod reduction and fixation (EXPEDIUM, Depuy Spine, Raynham, Massachusetts, USA; Voyager, Medtronic, Memphis, Tennessee, USA; and ES 2, Stryker Spine, Bordeaux, Cestas, France) were performed under general anesthesia. For the PVP procedure, hydroxyapatite block (HA block, HOYA, Tokyo, Japan) was inserted under constant fluoroscopy into the target vertebral body. In the VP, after inserting a thin-diameter thoracic HA block funnel into the fractured vertebral body using a bilateral transpedicular approach, 30–50 thoracic HA blocks are filled. In PVP with HA, the reduction is in situ fixation only by reduction with dynamic fracture mobility. And, after all the HA blocks are filled, the PPSs of the upper and lower vertebral bodies is sequentially inserted.
In group B, BKP and PPS-and-rod reduction and fixation (Viper PRIME, Depuy Spine; MUST, Medacta and, CD Horizon Solera Voyager, Medtronic; and ES 2, Stryker Spine, Bordeaux) were performed under general anesthesia. BKP was performed using the Kyphon Inc system (Medtronic Spine LLC, Sunnyvale, CA, USA). After the pedicle access needle insertion to the fractured vertebral body for guide wire insertion using a bilateral transpedicular approach, a deflated balloon was inserted into the fractured vertebral body, and inflated to restore the fractured vertebral body to its normal height position, and to create an internal cavity. The balloon was then deflated and removed. The remaining cavity was filled with polymethylmethacrylate (PMMA). Then, the PPSs of the upper and lower vertebral bodies are sequentially inserted until the cement hardens. Antibiotic prophylaxis (2 g of cefazoline during surgery and 2 g two times in the following 24 h) was used in both groups. After surgery, the patient was instructed to wear a custom-made soft brace (lumbosacral corset) in order to rest the soft tissues around the spine and to prevent malposition when getting out of bed. All patients received analgesics, physiotherapy, rehabilitation, and gait aids as needed. Physical therapy was started on the first day after surgery to facilitate walking. After discharge, the patient was encouraged to resume daily life and follow-up as an outpatient at the clinic.
Statistical analysis
Statistical analyses were performed with chi-squared (χ2) test for categorical data and the Mann-Whitney U test and Student t-test for surgical results to compare the two groups. Statistical test results were considered significant at P<0.05. All P values were two-sided. All statistical analyses of recorded data were performed using the Excel Statistical Software Package (Ekuseru-Toukei 2012; Social Survey Research Information Co., Ltd., Tokyo, Japan).
Results
There was no significant difference in age, gender, BMD, time from injury to surgery, preoperative VAS of low back pain or preoperative wedging angle of fractured vertebra between groups H and B (Table 1). Table 2 shows comparison of clinical results between two groups. Number of instrumented vertebrae is 3.1±0.6 in H group and 2.6±1.3 in B group, there was no difference between the two groups. The average operation time was 94.5±21.3 minutes in group H, 69.4±31.6 minutes in group B (P=0.011), and the average intraoperative blood loss was 100.0±43.0 g in group H and 62.9±25.8 g in group B (P=0.006). The average hospital length was 19.3±8.1 days in group H, 8.0±3.9 days in group B (P=0.000). There was a significant difference about the average operation time, the average intraoperative blood loss and the average hospital length between the two groups.
Table 2
| Clinical results | Group H | Group B | P value |
|---|---|---|---|
| Duration of operation (minutes) | 94.5±21.3 | 69.4±31.6 | 0.011 |
| Intraoperative blood loss (grams) | 100.0±43.0 | 62.9±25.8 | 0.006 |
| Number of instrumented vertebrae | 3.1±0.6 | 2.6±1.3 | 0.095 |
| Stay at hospital (days) | 19.3±8.1 | 8.0±3.9 | 0.000 |
Group H, HAVP + PPS; Group B, BKP + PPS. Data are presented as mean ± standard deviation. HAVP, vertebroplasty with hydroxyapatite; PPS, percutaneous pedicle screw; BKP, balloon kyphoplasty.
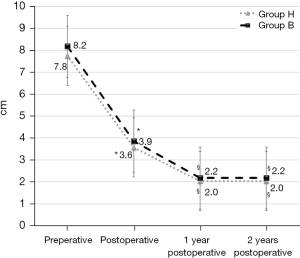
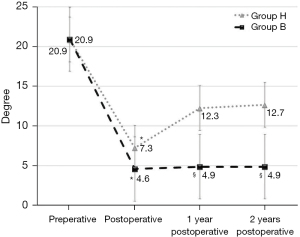
As shown in Figure 1, there was no significant difference before, immediately after surgery and one- and two-year after surgery between the two groups about changes of pre- and post-operative VAS for low back pain. The VAS immediately after surgery was significantly lower (P<0.005) than that of before surgery in two groups. The VAS at one- and two-year after surgery was significantly decreased (P<0.05) in two groups. As shown in Figure 2, there was no significant difference before, immediately after surgery between the two groups about changes of pre- and post-operative wedging angle of fractured vertebra. The wedging angle of fractured vertebra immediately after surgery was significantly lower (P<0.005) than that of before surgery in two groups. The wedging angle of fractured vertebra immediately after surgery was 7.3±6.1 degrees in group H and 4.6±3.5 degrees in group B, but no difference was observed. The wedging angle of fractured vertebra of one- and two-year after surgery was significantly higher (P<0.05) than that of immediately after surgery in group H, however, there is no difference in group B. The wedging angle of fractured vertebra one-year after surgery was 12.3±7.2 degrees in the H group and 4.9±3.4 degrees in the B group, showing a significant correction loss in the H group (P=0.002). The wedging angle of fractured vertebra two-year after surgery was 12.7±7.2 degrees in the H group and 4.9±3.4 degrees in the B group, showing a significant correction loss in the H group (P=0.002). In both groups, bone union was obtained in all cases one-year after surgery. None of the patients were found to have any postoperative neurological complications. None of the patients were performed implant removal within this follow up period.
Case report
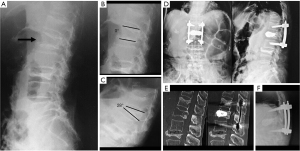
Figure 3 shows a case presentation of L1 painful OVF with wedging angle of fractured vertebra (28°) in an 84-year-old woman who experienced pain for 6 weeks.
Discussion
BKP + PPS for the treatment of TLOVF have minimum correction loss 2 years after surgery compared to HAVP + PPS. BKP and PVP are both safe and effective surgical procedures in treating OVF (14-17). BKP contributes especially to decreasing the mean difference of kyphotic wedge angle and risk of cement leakage and increasing the vertebral body height when compared with PVP (15). Others report that there were no differences in back pain or disability pain scores at any time point between PVP and BKP. There was no difference in the rate of symptomatic cement leakage, but BKP was associated with a lower rate of overall cement leakage and greater kyphosis correction (16).
The incidence of AVF is relatively high after BKP (9,10). Takahashi et al. (9) reported that more severe wedge angle before surgery; correction degree, old OVF presence, and thoracolumbar level were predictive factors for AVF.
Matsuura et al. reported in a study using finite element models (FEM) and quantitative computerized tomography (QCT) that the predicted vertebral body failure load was greater with PMMA reinforcement compared to that of the copolymer, negative group, and intact group, with a similar trend in predicted stiffness, with QCT/FEM was successful for predicting fracture loads of metastatic, polymer-augmented vertebral bodies (18). The greater the amount of cement injected to the fractured vertebral body with BKP, the greater the load on the upper adjacent vertebral body, but in cases of large vertebral instability, such as those with large intravertebral clefts, it is necessary to increase the amount of cement injected to restore of vertebral body height.
On the other hand, VP with HA block for OVF is safer with less fatal complications such as pulmonary thromboembolism compared with PMMA VP, and good results have been reported (19). In our experience, it is of concern that the procedure for filling the HA block into the fractured vertebral body is time-consuming and there is postoperative loss of vertebral height correction.
Minimally Invasive Spine Stabilization (MISt) is now widely used for spinal fractures, and PPS fixation is especially useful for fractures in the thoracolumbar region. Several studies have reported the advantages of PPS fixation (12,20,21). McAnany et al. (22) report a systematic literature review and meta-analysis comparing the surgical outcomes of open versus percutaneous fixation of traumatic thoracolumbar fractures. The advantages of MISt include relatively low intraoperative blood loss and operating time, which is especially important when percutaneous surgery treats multiple injured patients. Takami et al. (23) reported that they treated the patients of type A3 fresh thoracolumbar burst fractures in AO classification by combining percutaneous short pedicle screw (PS) fixation and VP with transpedicular intracorporeal HA blocks grafting, and this method is less invasive and can preserve the adjacent healthy mobile segment. Salle et al. (24) reported that the kyphosis treatment was more effective on Magerl A3 and B2 fractures than on those classified as A2.3, as well as for fractures with slight posterior wall protrusion on the spinal canal regarding the treatment of traumatic thoracolumbar fractures regarding minimally invasive percutaneous stabilization plus BKP. Salle et al. (25) also recommend using vertebral body stenting (VBS) rather than open surgery for A3.2 and A2 fractures at the thoracolumbar junction and in young patients.
For cases with large intravertebral instability, that is, cases with large intravertebral cleft, and cases with large intervertebral instability, that is, end plate injury and PLC injury. By kyphotic correction with a balloon and filling a sufficient amount of cement into the fractured vertebral body to obtain as much anterior strut reconstruction as possible due to PMMA augmentation in the vertebral body, and by performing posterior spinal stabilization with PPS. As a result of this series of procedures, the concept of BKP + PPS is to disperse the stress on the BKP vertebral body, the adjacent vertebral bodies and the adjacent intervertebral discs.
In addition, good results of other implant techniques for OVF have been reported in recent years. introduced vertebral augmentation techniques using intravertebral distraction devices, such as VBS, armed kyphoplasty and Spine Jack, could be effective in fracture reduction (25,26).
From the results of our study, BKP + PPS has less surgical time and intraoperative blood loss than HAVP + PPS, and short-term results are as good as HAVP + PPS. BKP + PPS is a minimally invasive and very useful method for elderly people with painful OVF. We believe that it can be considered as a palliative surgery for cases where hesitation in anterior fusion, which becomes more invasive depending on the age and general condition of the patient.
Fuentes et al. (27) reported that BKP and 1-above, 1-below PPS fixation were performed in patients with thoracolumbar burst fractures classified type A3 on the Magerl scale, and kyphosis correction and vertebral body height were maintained at 2 years after surgery, and similar vertebral height recovery and kyphosis correction rates to those obtained with open surgery.
Verlaan et al. (28) reported that BKP after posterior short segment reduction and fixation to treat traumatic burst fractures and showed that the technique was practical and effective.
Yan et al. (29) reported that BKP combined with posterior PS fixation was shown to be an effective treatment for osteoporotic thoracolumbar burst fractures. This procedure has advantages such as single approach, reconstruction of 3 spinal columns, less blood loss, short operation time, and rapid recovery.
Gu et al. (12) reported comparison of PVP alone and combination of PVP and posterior fixation with a PS via intramuscular approach without bone graft for acute OVF patient resulted PVP combined with PS had more vertebral body height and little correction loss of local kyphosis than PVP alone for an average 27 months follow-up. This suggests the usefulness of posterior fusion without bone graft.
Minimally invasive PS fixation combined with PVP is a good choice for the treatment of acute TLOVF, which can prevent secondary VCF after PVP (30).
Both HAVP + PPS and BKP + PPS are not a spinal fusion for the purpose of intervertebral fusion, but a stabilization technique that suppresses intervertebral mobility and an operation that promotes fusion of the fractured vertebral body. After that, as a general, it is a surgical procedure that is premised on implant removal in the future. Wild et al. (31) reported that in spinal surgery implant removal is performed for a number of indications, such as infection treatment, misplaced implants, implant failure, protruding instrumentation and routinely after fracture treatment with instrumentation of non-fused segments. Vanek et al. (32) reported that the instrumentation was removed from the mobile part of the lumbar spine (below L2) at 1 to 1.5 years after the surgery in the treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. However, there are many cases where intervertebral fusion is obtained by the bridging bony spur formation between the upper and lower vertebral bodies in the cases of OVFs, and in the cases of DISH patients (33), in our opinion, implant removal after PPS fixation is not necessary in such cases. Regarding the necessity and timing of implant removal after PPS fixation for OVF treatment, there is no clear consensus standard, however, we explain for the all patients that this method is not spinal fusion but spinal stabilization before surgery. If there is symptom due to a failure of instrumentation or if there is hope after the completion of bone union, we decide to remove the implants. In reality, the patient may not want implant removal because of their old age.
The reason that BKP + PPS has a shorter operation time than HAVP + PPS is that the PPS can be inserted after the fractured vertebral body is filled with cement and before the cement is sufficiently hardened. On the other hand, in HAVP + PPS, we think that it is because PPS can be inserted only after filling all HA blocks into the fractured vertebra. It takes longer to fill the HA block into the vertebrae one by one with HAVP than it takes to inflate the balloon with BKP. This is the reason why BKP is a shorter surgery.
From the results of this study, compared to HAVP + PPS, BKP + PPS maintained the wedge angle of the fractured vertebral body one year after surgery.
BKP contributed to immediate pain relief, but did not improve the global sagittal spinal alignment after OVF (34), on the other hand, there is also a report that percutaneous kyphoplasty can significantly improves the overall sagittal alignment (35). Since BKP + PPS can prevent local kyphosis due to collapse of fractured vertebral body, it may be possible to expect better global alignment than HAVP + PPS.
The results of the present study indicate that BKP + PPS is less invasive to the elderly because it has less surgery time, less intraoperative blood loss, compared with HAVP + PPS and good short-term results.
We recommend the indication of BKP + PPS for TLOVF in cases with large intra-vertebral instability and cases with inter-vertebral instability. There are cases of large instability in the vertebral body, such as cases with large clefts (10 degrees or more) and cases with vertebral anterior wall or lateral side wall defect.
And as a case with inter-vertebral instability, there are cases with end plate injury and intervertebral disc injury, and cases with posterior supporting tissue injury such as spinous process fractures. We also think that some cases of DISH are applicable.
The limitation of this study is that the postoperative follow-up period is short, at least two years. However, the bony fusion of vertebral body fracture is usually prolongation in 9 months and pseudo arthrosis in 12 months. In terms of determining bone union, we think the postoperative follow-up period of this study is reasonable. Staartjes et al. (36) showed that 1 year of follow-up may be sufficient to evaluate patient-reported postoperative outcomes of spine surgery. Masuda et al. (37) reported if the follow-up is longer than 1 year, factor unrelated to surgery may possibly influence of outcome. The second limitation of this study is its retrospective nature; another is the lack of preoperative and postoperative patient-oriented outcome measures even with a relatively large number of patients. However, due to the small number of patients and short follow-up period, long term follow-up and studies of larger sample size are needed to determine the value of the proposed method.
This method, BKP + PPS, is minimally invasive surgical treatment for the case of painful TLOVF, and we believe that it can be a palliative surgery for cases where the patient is very old and there are many comorbidities and hesitates to perform anterior spinal fusion. Furthermore, long-term follow-up is necessary to accumulate cases and to identify the indication cases of this method. In addition, further verification is needed in the future regarding the necessity of implant removal when bone fusion is obtained.
Conclusions
PPS fixation combined with percutaneous vertebral cement augmentation with BKP for unstable thoracolumbar osteoporotic vertebral fracture was suggested to be minimally invasive in the elderly. In addition, there is no correction loss of the fractured vertebral body after BKP, which is considered to be a useful surgical procedure. Further long-term follow-up and further verification are necessary, including the necessity of implant removal.
Acknowledgments
Funding: Tsutomu Akazawa received research support from Medtronic.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1024/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1024/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1024/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1024/coif). Tsutomu Akazawa received research support from Medtronic. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The protocol for this study was reviewed and approved by the ethics committee of our institution named—“Funabashi orthopaedic hospital ethics committee”; approval number: 2019036; approval date: 2019.09.26. Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kishikawa Y. Initial non-weight-bearing therapy is important for preventing vertebral body collapse in elderly patients with clinical vertebral fractures. Int J Gen Med 2012;5:373-80. [Crossref] [PubMed]
- Ito Y, Hasegawa Y, Toda K, et al. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J 2002;2:101-6. [Crossref] [PubMed]
- Katsumi K, Hirano T, Watanabe K, et al. Surgical treatment for osteoporotic thoracolumbar vertebral collapse using vertebroplasty with posterior spinal fusion: a prospective multicenter study. Int Orthop 2016;40:2309-15. [Crossref] [PubMed]
- Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a andomized controlled trial. Lancet 2009;373:1016-24. [Crossref] [PubMed]
- McGraw JK, Cardella J, Barr JD, et al. Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol 2003;14:827-31. [Crossref] [PubMed]
- Minamide A, Maeda T, Yamada H, et al. Early versus delayed kyphoplasty for thoracolumbar osteoporotic vertebral fractures: The effect of timing on clinical and radiographic outcomes and subsequent compression fractures. Clin Neurol Neurosurg 2018;173:176-81. [Crossref] [PubMed]
- Takahashi S, Hoshino M, Yasuda H, et al. Characteristic radiological findings for revision surgery after balloon kyphoplasty. Sci Rep 2019;9:18513. [Crossref] [PubMed]
- Nakamae T, Yamada K, Tsuchida Y, et al. Risk Factors for Cement Loosening after Vertebroplasty for Osteoporotic Vertebral Fracture with Intravertebral Cleft: A Retrospective Analysis. Asian Spine J 2018;12:935-42. [Crossref] [PubMed]
- Takahashi S, Hoshino M, Yasuda H, et al. Development of a scoring system for predicting adjacent vertebral fracture after balloon kyphoplasty. Spine J 2019;19:1194-201. [Crossref] [PubMed]
- Campbell PG, Harrop JS. Incidence of fracture in adjacent levels in patients treated with balloon kyphoplasty: a review of the literature. Curr Rev Musculoskelet Med 2008;1:61-4. [Crossref] [PubMed]
- Zafeiris CP, Lyritis GP, Papaioannou NA, et al. Hypovitaminosis D as a risk factor of subsequent vertebral fractures after kyphoplasty. Spine J 2012;12:304-12. [Crossref] [PubMed]
- Gu Y, Zhang F, Jiang X, et al. Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty in the surgical treatment of thoracolumbar osteoporosis fracture. J Neurosurg Spine 2013;18:634-40. [Crossref] [PubMed]
- Ishii K, Kaneko Y, Funao H, et al. A Novel Percutaneous Guide Wire (S-Wire) for Percutaneous Pedicle Screw Insertion: Its Development, Efficacy, and Safety. Surg Innov 2015;22:469-73. [Crossref] [PubMed]
- Chandra RV, Maingard J, Asadi H, et al. Vertebroplasty and Kyphoplasty for Osteoporotic Vertebral Fractures: What Are the Latest Data? AJNR Am J Neuroradiol 2018;39:798-806. [Crossref] [PubMed]
- Wang H, Sribastav SS, Ye F, et al. Comparison of Percutaneous Vertebroplasty and Balloon Kyphoplasty for the Treatment of Single Level Vertebral Compression Fractures: A Meta-analysis of the Literature. Pain Physician 2015;18:209-22. [PubMed]
- Wang B, Zhao CP, Song LX, et al. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: a meta-analysis and systematic review. J Orthop Surg Res 2018;13:264. [Crossref] [PubMed]
- Goldstein CL, Chutkan NB, Choma TJ, et al. Management of the Elderly With Vertebral Compression Fractures. Neurosurgery 2015;77:S33-45. [Crossref] [PubMed]
- Matsuura Y, Giambini H, Ogawa Y, et al. Specimen-specific nonlinear finite element modeling to predict vertebrae fracture loads after vertebroplasty. Spine (Phila Pa 1976) 2014;39:E1291-6. [Crossref] [PubMed]
- Nishioka K, Imae S, Kitayama M, et al. Percutaneous vertebroplasty using hydroxyapatite blocks for the treatment of vertebral body fracture. Neurol Med Chir (Tokyo) 2009;49:501-6. [Crossref] [PubMed]
- Wang H, Zhou Y, Li C, et al. Comparison of Open Versus Percutaneous Pedicle Screw Fixation Using the Sextant System in the Treatment of Traumatic Thoracolumbar Fractures. Clin Spine Surg 2017;30:E239-46. [Crossref] [PubMed]
- Sun XY, Zhang XN, Hai Y. Percutaneous versus traditional and paraspinal posterior open approaches for treatment of thoracolumbar fractures without neurologic deficit: a meta-analysis. Eur Spine J 2017;26:1418-31. [Crossref] [PubMed]
- McAnany SJ, Overley SC, Kim JS, et al. Open Versus Minimally Invasive Fixation Techniques for Thoracolumbar Trauma: A Meta-Analysis. Global Spine J 2016;6:186-94. [Crossref] [PubMed]
- Takami M, Yamada H, Nohda K, et al. A minimally invasive surgery combining temporary percutaneous pedicle screw fixation without fusion and vertebroplasty with transpedicular intracorporeal hydroxyapatite blocks grafting for fresh thoracolumbar burst fractures: prospective study. Eur J Orthop Surg Traumatol 2014;24:S159-65. [Crossref] [PubMed]
- Salle H, Meynard A, Auditeau E, et al. Treating traumatic thoracolumbar spine fractures using minimally invasive percutaneous stabilization plus balloon kyphoplasty: a 102-patient series. J Neurointerv Surg 2021;13:848-53. [Crossref] [PubMed]
- Salle H, Tran GV, Faure P, et al. Treatment of A3.2 and A2 traumatic thoracolumbar spine compression fractures using vertebral body stenting: a 63-patient series. J Neurointerv Surg 2023;15:86-90. [Crossref] [PubMed]
- Venier A, Roccatagliata L, Isalberti M, et al. Armed Kyphoplasty: An Indirect Central Canal Decompression Technique in Burst Fractures. AJNR Am J Neuroradiol 2019;40:1965-72. [Crossref] [PubMed]
- Fuentes S, Blondel B, Metellus P, et al. Percutaneous kyphoplasty and pedicle screw fixation for the management of thoraco-lumbar burst fractures. Eur Spine J 2010;19:1281-7. [Crossref] [PubMed]
- Verlaan JJ, Dhert WJ, Verbout AJ, et al. Balloon vertebroplasty in combination with pedicle screw instrumentation: a novel technique to treat thoracic and lumbar burst fractures. Spine (Phila Pa 1976) 2005;30:E73-9. [Crossref] [PubMed]
- Yan H, Ni M, Zhai W, et al. Balloon kyphoplasty combined with posterior pedicle screw fixation for the treatment of osteoporotic thoracolumbar burst fractures. Ann Palliat Med 2021;10:7514-24. [Crossref] [PubMed]
- Gu YT, Zhu DH, Liu HF, et al. Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty for preventing secondary fracture after vertebroplasty. J Orthop Surg Res 2015;10:31. [Crossref] [PubMed]
- Wild A, Pinto MR, Butler L, et al. Removal of lumbar instrumentation for the treatment of recurrent low back pain in the absence of pseudarthrosis. Arch Orthop Trauma Surg 2003;123:414-8. [Crossref] [PubMed]
- Vanek P, Bradac O, Konopkova R, et al. Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine 2014;20:150-6. [Crossref] [PubMed]
- Okada E, Shiono Y, Nishida M, et al. Spinal fractures in diffuse idiopathic skeletal hyperostosis: Advantages of percutaneous pedicle screw fixation. J Orthop Surg (Hong Kong) 2019;27:2309499019843407. [Crossref] [PubMed]
- Kanayama M, Oha F, Iwata A, et al. Does balloon kyphoplasty improve the global spinal alignment in osteoporotic vertebral fracture? Int Orthop 2015;39:1137-43. [Crossref] [PubMed]
- Cao Z, Wang G, Hui W, et al. Percutaneous kyphoplasty for osteoporotic vertebral compression fractures improves spino-pelvic alignment and global sagittal balance maximally in the thoracolumbar region. PloS One 2020;15:e0228341. [Crossref] [PubMed]
- Staartjes VE, Siccoli A, de Wispelaere MP, et al. Patient-reported outcomes unbiased by length of follow-up after lumbar degenerative spine surgery: Do we need 2 years of follow-up? Spine J 2019;19:637-44. [Crossref] [PubMed]
- Masuda S, Kanba Y, Kawai J, et al. Outcomes after decompression surgery without fusion for patients with lumbar spinal stenosis and substantial low back pain. Eur Spine J 2020;29:147-52. [Crossref] [PubMed]


