
Fully-immersive virtual reality instrumental activities of daily living training for mild dementia: a feasibility study
Highlight box
Key findings
• Fully-immersive, virtual reality-based, instrumental activities of daily living (I-ADL) training is feasible for people with mild dementia and provides them with a high level of satisfaction and immersion.
What is known and what is new?
• Most of the VR studies in people with mild dementia have been developed for cognitive improvement. However, this study is focused on the I-ADL. This is the first study to directly provide I-ADL contents for participants who were having difficulties carrying out their daily life activities.
What is the implication, and what should change now?
• Although the maintenance of I-ADL is important for people with mild dementia, I-ADL training is not easy to implement in a resource-limited environment, such as a hospital. Therefore, we believe that this study on the intervention using VR can be of great help in the future.
Introduction
According to the World Alzheimer Report of 2018, 50 million people worldwide live with dementia, and the number increases every year (1).
This disorder is most common in older people. It is recognized as one of the greatest problems of the 21st century (2). Disability, particularly the loss of ability to perform activities of daily living (ADL), is a defining feature leading to a higher caregiver burden and eventually the need for alternative care or nursing home placement (3).
The Instrumental Activities of Daily Living (I-ADL) performance provides reliable measures of functional levels and dementia severity (4).
It is possible that I-ADL impairment may accelerate decline in the cognitive functioning of people with dementia (3).
The most important goal of rehabilitation is, therefore, to maintain independent daily living as long as possible through I-ADL training, even after the onset of cognitive deficiency. Hence, the onset of mild dementia, is a good time to begin training. This is because cognitive rehabilitation is based on relatively well-preserved cognitive abilities (5). Consequently, such individuals may benefit from interventions.
I-ADL training in hospitals is limited due to constraints on time and space. Although it would be best for clinicians to observe and evaluate their performances of the I-ADL, they currently have to rely on surveys of patients and care givers.
Multisensory virtual reality (VR) platforms, which help people experience real-life situations, are advanced, adaptable, and easy to use (6-10). These technologies can be used for cognitive rehabilitation in people with dementia (11,12).
It has been reported that immersive VR can improve cognitive functioning (13-15) because it presents goal-oriented tasks and enhances neuroplasticity by means of repetition (16).
However, only a few studies have been conducted on cognitive training using fully-immersive type for people with mild dementia (7,17). Moreover, most VR studies focused on cognitive improvement, but not on improving the I-ADL (18).
The purpose of this study is, therefore, to confirm whether VR is safe, feasible, and effective in I-ADL training. We present the following article in accordance with the TREND reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-847/rc).
Methods
Participants
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of the Asan Medical Center (No. 2020-1861) and informed consent was taken from all the patients. Based on previous studies (19,20), an estimate of at least seven to ten participants are needed to confirm feasibility.
From July 2021 to February 2022, people with mild dementia who visited the outpatient clinic in the Department of Rehabilitation Medicine at the Asan Medical Center were prospectively enrolled.
Participants were included on the basis of: (I) a Korean mini-mental state examination (K-MMSE) score >17, or a Global Deterioration Scale (GDS) score of 2–5; (II) a mild dementia diagnosis by a neuropsychological assessment conducted by a neuropsychologist; and (III) the physical ability to perform the VR training (Berg balance scale score >41, with a minimum of one good grade result for an upper extremity manual muscle test).
A total of seven participants were enrolled and underwent the screening process.
Intervention
This study evaluated the feasibility of a fully-immersive VR I-ADL training program.
Our research team and bHaptics jointly developed this training program. We presented the contents of the most necessary tasks for people with mild dementia based on the items outlined in the I-ADL. On the other hand, bHaptics was in charge of the technical implementation.
Participants were subjected to 10 sessions (2 or 3 times a week) of fully-immersive I-ADL training over 4 weeks. Each session lasted for 70 min, including instruction time regarding VR devices and resting time between VR training, as described in Figure 1.

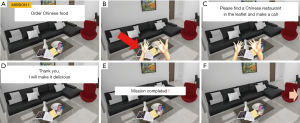
The program was led by an occupational therapist. Participants were presented with missions that related to daily activities corresponding to items in the I-ADL. Each mission had subtasks for the participants to perform. Five different VR missions were used (Figure 2). Participants could choose those with which they struggled in daily life.

If a participant failed to perform a task during their mission, a hint was provided. If the participant was successful, he or she moved on to the next task (Figure 3).
The I-ADL factors relating to the composition of each mission are described in Table 1.
Table 1
| Missions | Places | Factor of I-ADL | Stage of mission | Sub-task |
|---|---|---|---|---|
| Cleaning | House (kitchen, living room) | Home establishment and management | 3 | Separate garbage; wipe the table; tidy up the desk |
| Grocery shopping | Grocery store | Shopping; financial management | 4 | Getting ready to go grocery shopping; grocery shopping; pay money; organization purchased things |
| Cooking (instant noodle) | House (kitchen) | Home establishment and management; meal preparation and clean up | 4–5 (the stage is different by grade) | Ready to cook instant noodle; boiling water; cooking instant noodle; table setting; washing and organizing dishes |
| Going to the hospital | House | Health management and maintenance | 4 | Choosing the right clothes for the season; picking seasonal items; choosing essential things; do a safety check |
| Ordering food | Food court | Shopping; financial management | 2 | Ordering food; importing ordered food to seat |
I-ADL, instrumental activities of daily living.
VR program
A 360-degree video allowed participants to look in every direction to maximize the realism of situations.
A Valve Index (Valve Corporation, Bellevue, WA, USA) VR head-mounted display with Valve Index Controllers were used throughout the experiment. The controller was particularly appropriate for the experiment because it allowed the participants to grab and release virtual objects more naturally with their hands, rather than by pressing buttons. Various objects could be manipulated using Valve Index Controllers It allowed participants to interact with the environment and move animated objects through their hand and arm movements.
The participants were seated next to the therapist to prevent safety problems during the VR sessions.
Feasibility
We evaluated the participants’ satisfaction with the VR I-ADL training using a self-report questionnaire based on a 10-point Likert-type scale. There were four items in the questionnaire: overall satisfaction, motivation, stability, and fatigue. Higher scores indicated more positive results.
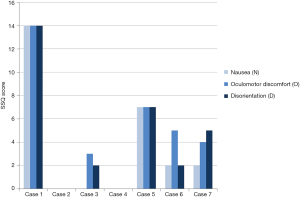
To assess immersion, researchers asked the participants to respond to a presence questionnaire that consisted of nine items, each scored out of seven points (Appendix 1). To evaluate the participants’ tolerance for VR, the researchers measured adherence, which was calculated as average actual execution time [actual duration of execution (min)/20 min (1 session) × 100 (%)] for all sessions. We also asked the participants to respond to the Simulator Sickness Questionnaire (SSQ) (Appendix 2) that determined the subjective severity ratings of 16 symptoms on a scale from 0 (no perception) to 3 (severe perception) after the VR intervention. The ratings for the individual symptoms were grouped into three non-mutually exclusive categories representing symptoms for nausea (N), oculomotor disturbance (O), and disorientation (D). The score of each category was defined as the sum of its symptom scores. Higher scores indicated stronger perceptions of the symptoms. Based on a large sample of SSQ data gathered from military pilots, it is suggested that total scores can be associated with negligible [<5], minimal [5–10], significant [10–15], or concerning [15–20] symptoms (21-23).
Outcome
Cognitive functioning was assessed by psychology specialists according to standardized methods. Global cognitive functioning was assessed with the K-MMSE (24).
Cognitive functioning was evaluated in detail with the Korean Version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD-K), which is a reliable and valid equivalent of the English version of the CERAD clinical and neuropsychological assessment batteries (25). The battery includes verbal fluency, Boston naming test, word list memory, constructional praxis, word list recall, word list recognition, constructional recall, and trail making tests.
The Seoul-IADL (S-IADL) was used for the I-ADL evaluation. It is a reliable assessment for the functional disabilities of Korean people with dementia. Particularly, the S-IADL has a higher sensitivity and greater specificity than other I-ADL instruments, making it useful for the early detection of dementia (26). S-IADL consists of 15 I-ADL items, and each item is rated from 0 (no impairment) to 3 (severe impairment), with a highest possible total score of 45 points. Both participants and caregivers answered the questionnaire.
Each participant’s mood was assessed by the Beck Depression Index (BDI), which contains 21 items that are rated on a four-point scale from 0 (symptom absent) to 3 (symptom severe) (27).
Statistical analysis
Baseline characteristics and assessment data are expressed in terms of the mean and standard deviation (SD) for continuous variables. The Wilcoxon signed-ranks test was used to evaluate differences in the I-ADL, and BDI, both pre- and post-intervention. A P value <0.05 was considered statistically significant. SPSS Statistics 25.0 for Windows (IBM Corp, Armonk, NY) was used for all analyses.
Results
A total of seven participants with mild dementia were enrolled in this study.
There were no dropouts with serious side effects.
Table 2 describes the demographics of the study population, dementia type, global cognitive functioning, and baseline physical functioning.
Table 2
| No. | Age (years) | Gender | Dementia type | K-MMSE | GDS | BBS | MMT |
|---|---|---|---|---|---|---|---|
| 1 | 76 | Male | Vascular | 18 | 4 | 51 | N/N |
| 2 | 57 | Male | Vascular | 28 | 3 | 49 | N/N |
| 3 | 67 | Male | Vascular | 22 | 4 | 53 | N/N |
| 4 | 69 | Male | Alzheimer | 25 | 4 | 51 | N/N |
| 5 | 69 | Female | Frontotemporal | 22 | 4 | 50 | N/N |
| 6 | 73 | Male | Vascular | 24 | 5 | 50 | N/N |
| 7 | 86 | Female | Alzheimer | 21 | 3 | 49 | N/N |
K-MMSE, Korean version of the Mini-Mental-State-Exam; GDS, Global Deterioration Scale; BBS, Berg Balance Scale; MMT, Manual Muscle Test.
Feasibility
During the VR program, the researchers observed the participants’ acceptability, immersion, and tolerance (Table 3). The acceptability score (emotion, motivation, security, fatigue) was evaluated as high. The mean immersion score was 50.42±7.89 points. The mean adherence (an indicator of VR tolerance) was 83.71±6.10 points. In the SSQ, another indicator of tolerance, only one participant revealed a moderate motion sickness side effect, and six participants exhibited minimal or negligible side effects (Figure 4).
Table 3
| No. | Acceptability | Presence | Adherence | |||
|---|---|---|---|---|---|---|
| Satisfaction | Motivation | Stability | Fatigue | |||
| 1 | 9 | 9 | 9 | 9 | 54 | 94 |
| 2 | 9 | 9 | 10 | 9 | 33 | 82 |
| 3 | 9 | 9 | 9 | 9 | 52 | 81 |
| 4 | 10 | 10 | 10 | 10 | 54 | 75 |
| 5 | 9 | 8 | 9 | 8 | 55 | 83 |
| 6 | 9 | 9 | 8 | 7 | 50 | 89 |
| 7 | 7 | 7 | 5 | 7 | 55 | 82 |
| Mean ± SD | 8.85±0.89 | 8.71±0.95 | 8.57±1.71 | 8.42±1.13 | 50.42±7.89 | 83.71±6.10 |
| Range | 7–10 | 7–10 | 5–10 | 7–10 | 33–55 | 75–94 |
VR, virtual reality; I-ADL, instrumental activities of daily living; SD, standard deviation.
Outcome
The answers to each item of the I-ADL were consistent between the caregiver and participant. I-ADL scores improved significantly after VR training. Positive changes were also observed on the BDI (Table 4).
Table 4
| No. | I-ADL | BDI | |||
|---|---|---|---|---|---|
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | ||
| 1 | 36 | 36 | 14 | 12 | |
| 2† | 19 | 8 | 31 | 14 | |
| 3 | 15 | 10 | 10 | 4 | |
| 4 | 14 | 12 | 11 | 8 | |
| 5 | 36 | 36 | 9 | 2 | |
| 6 | 17 | 14 | 11 | 5 | |
| 7 | 19 | 14 | 9 | 7 | |
| Mean ± SD | 22.28±9.55 | 18.57±12.09 | 13.57±7.87 | 7.42±4.31 | |
| Range | 14–36 | 8–36 | 9–31 | 2–14 | |
| P value | 0.042* | 0.018* | |||
†, participant with marked improvement in particular. Wilcoxon signed-ranks between pre- and post-intervention; *, a significant difference between the pre-intervention and post-intervention. I-ADL, instrumental activities of daily living; BDI, Beck Depression Index; VR, virtual reality; SD, standard deviation.
In the CERAD-K, improvement was observed in Word List Delayed Recall test and the Trail Making Test-B (TMT-B) between the pre- and post-intervention in all participants (Table 5). Two participants, however, failed to complete the TMT-B test due to impairments in their cognitive functioning. Thus, only five people successfully completed the TMT-B test. There were no significant differences in other parameters, between pre- and post-intervention performances.
Table 5
| Subset | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |||||||
| Boston naming (−/15 score) | 3 | 1 | 11 | 12 | 10 | 9 | 10 | 10 | 7 | 9 | 13 | 14 | 7 | 6 | ||||||
| Verbal fluency (score) | 0 | 0 | 9 | 7 | 21 | 16 | 13 | 15 | 3 | 0 | 9 | 7 | 7 | 7 | ||||||
| Constructional praxis (−/11 score) | 11 | 11 | 11 | 11 | 11 | 11 | 11 | 10 | 11 | 11 | 10 | 9 | 8 | 7 | ||||||
| Wordlist learning (−/30 score) | 5 | 2 | 22 | 21 | 18 | 22 | 19 | 19 | 2 | 0 | 14 | 12 | 11 | 10 | ||||||
| Wordlist delayed recall (−/10 score) | 0 | 1 | 8 | 10 | 8 | 9 | 2 | 4 | 0 | 0 | 4 | 5 | 0 | 1 | ||||||
| Wordlist instruction (−/10 score) | 2 | 1 | 10 | 10 | 10 | 10 | 8 | 7 | 0 | 0 | 8 | 8 | 8 | 6 | ||||||
| Visuo-construction recall (−/11 score) | 7 | 5 | 8 | 11 | 8 | 11 | 4 | 2 | 0 | 0 | 10 | 10 | 0 | 0 | ||||||
| TMT-A§ (s) | 164 | 178 | 37 | 32 | 47 | 45 | 50 | 33 | 72 | 68 | 66 | 66 | 120 | 165 | ||||||
| TMT-B§ (s) | NA‡ | NA‡ | 100 | 80 | 267 | 207 | 105 | 101 | NA‡ | NA‡ | 180 | 163 | 267 | 207 | ||||||
‡, the test could not be performed due to cognitive decline. §, improvement was observed between the pre-intervention and post-intervention in all participants. CERAD-K, Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet; VR, virtual reality; TMT A, trail making test A; TMT B, trail making test B; NA, not available.
Discussion
We developed an I-ADL training program using a fully-immersive VR program for people with mild dementia.
We found that a 4-week course of fully-immersive VR I-ADL training was feasible and produced functional and cognitive gains.
Motivation is the most important part of rehabilitation for people with dementia (28). Hence, high satisfaction with VR treatment and good adherence is a great advantage. Manera et al. (7,29) reported that people with Alzheimer’s disease had higher levels of satisfaction with VR exercises than with conventional exercises.
While most previous studies used semi-immersive VR techniques (30), this study showed that fully immersive VR, which utilizes an environment that is closer to reality, also shows similarly high levels of satisfaction.
In addition, most previous VR studies focused on contents that stimulated cognitive functioning (31). However, this study focused on improving I-ADL. Hence, this study is the first to provide the I-ADL contents that the participants were having difficulties with in daily life. In this study, I-ADL were significantly improved by the VR program, indicating that this training might help people with mild dementia maintain independence in daily life as long as possible. However, due to the small number and absence of a control group, the statistical significance may be overestimated in this study. Case 2 (Table 4) showed significantly improved I-ADL and BDI scores compared to other cases, which may have affected the statistical significance. The high improvement levels in this participant may be due to his relatively younger age (57 years old) and higher initial MMSE score of 28, compared to other participants. Also, given that the initial BDI was high (score: 31), pseudodementia cannot be excluded. However, considering that there is no marked improvement in the CERAD items in case 2, the improvement in I-ADL seems to be due to the effects of intervention rather than mood improvement.
Another strength of this study is that the intervention was task specific and gave the participants a meaningful task. It is known that such task specific intervention can stimulate cortical reorganization and improve functioning (20,32).
Motion sickness is a common side effect of the VR system, especially when using fully-immersive VR. This limitation has been an obstacle in applying VR training to certain people (33).
In this study, although one participant had moderate motion sickness, six participants showed minimal or negligible side effects. The participant with moderate side effects complained of symptoms only at the beginning and adapted over time. It is well known that VR is safe and acceptable in people with mild cognitive impairment and dementia. However, in a review by Papaioannou et al., most studies utilized a non-immersive type (30). There is not much data on the fully-immersive type. In addition, it is known that susceptibility to motion sickness may increase with aging (34). This can be a serious problem for people with dementia. Thus, in this study, to minimize these risks, participants sat down in a chair and the therapist helped them reduce unnecessary movements while performing the VR intervention. Because it is known that side effects may be reduced by minimizing factors that cause motion sickness such as standing and head movements (35,36).
Regarding cognition, improvement was observed in Word List Delayed Recall test and TMT-B in all participants. This is in line with the results of a systematic review (37). A recent VR study has also reported improvements in executive functioning (38) after a VR intervention. Executive functioning is usually measurable by the TMT (39). TMT-A measures psychomotor speed and visual scanning, and TMT-B measures working memory (40-42). Our results showed improvements in TMT-B but not in TMT-A, which is consistent with a previous report (43). However, two participants failed the TMT-B test due to cognitive decline. In addition, due to the small number and the multiple comparison problem, statistical significance could not be presented. Further research is needed to present statistical values with a larger number of participants. After the VR intervention, the improvements evident on the BDI scale, suggest that it might, furthermore, be helpful in improving the moods of people with mild dementia. This finding is in line with previous studies stating that psychosocial interventions through multisensory stimulation induced not only emotional and social benefits but also a conserved sense of identity for those with these disorders (44-46).
Limitations
This study has certain limitations. First, it cannot demonstrate the usefulness of VR I-ADL training in people with mild dementia. Because the sample number was small, and it was not a comparative study. Further studies including control groups are needed to verify effectiveness. Second, some participants had difficulty using controllers. To solve this problem, time was required to explain the use of the controller in every session. Third, there is no procedure to check the validation for each VR task. However, the most necessary task for people with mild dementia was determined by referring to the S-IADL item and feasibility was checked through this study. Fourth, a positive change in mood was seen in all participants. These changes may have affected cognition and function as a secondary gain. In the future, it will be necessary to analyze the correlation of each factor. Finally, in this study, heterogenous participants were analyzed. Since the progress and prognosis of the disease is different depending on the dementia type, it is necessary to analyze the effect of the dementia type and various factors such as age, sex, and dementia severity in future studies.
Conclusions
Fully-immersive VR I-ADL training is feasible and may improve functioning, mood, and cognition in people with mild dementia. However, further studies are needed to compare conventional treatments with VR treatment.
Acknowledgments
Funding: This research was funded by bHaptics Inc. The funder had no role in the study design, data collection, data analysis, interpretation of data, presentation of results, or decision to submit for publication
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-847/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-847/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-847/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-847/coif). KUG is an employee of bHaptics Inc. All authors report the funding from bHaptics Inc. The authors have no other conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- The state of the art of dementia research: new frontiers. Alzheimer’s Disease International, London (UK). 2018. Available online: https://www.alzint.org/resource/world-alzheimer-report-2018/. Accessed Jul 11 2022.
- Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet 2017;390:2673-734. [Crossref] [PubMed]
- Rajan KB, Hebert LE, Scherr PA, et al. Disability in basic and instrumental activities of daily living is associated with faster rate of decline in cognitive function of older adults. J Gerontol A Biol Sci Med Sci 2013;68:624-30. [Crossref] [PubMed]
- Desai AK, Grossberg GT, Sheth DN. Activities of daily living in patients with dementia: clinical relevance, methods of assessment and effects of treatment. CNS Drugs 2004;18:853-75. [Crossref] [PubMed]
- Kudlicka A, Martyr A, Bahar-Fuchs A, et al. Cognitive rehabilitation for people with mild to moderate dementia. Cochrane Database Syst Rev 2019;2019:CD013388. [Crossref]
- Anderson AP, Mayer MD, Fellows AM, et al. Relaxation with Immersive Natural Scenes Presented Using Virtual Reality. Aerosp Med Hum Perform 2017;88:520-6. [Crossref] [PubMed]
- Manera V, Chapoulie E, Bourgeois J, et al. A Feasibility Study with Image-Based Rendered Virtual Reality in Patients with Mild Cognitive Impairment and Dementia. PLoS One 2016;11:e0151487. [Crossref] [PubMed]
- McEwen D, Taillon-Hobson A, Bilodeau M, et al. Two-week virtual reality training for dementia: Single case feasibility study. J Rehabil Res Dev 2014;51:1069-76. [Crossref] [PubMed]
- Moyle W, Jones C, Dwan T, et al. Effectiveness of a Virtual Reality Forest on People With Dementia: A Mixed Methods Pilot Study. Gerontologist 2018;58:478-87. [Crossref] [PubMed]
- Zygouris S, Ntovas K, Giakoumis D, et al. A Preliminary Study on the Feasibility of Using a Virtual Reality Cognitive Training Application for Remote Detection of Mild Cognitive Impairment. J Alzheimers Dis 2017;56:619-27. [Crossref] [PubMed]
- Jeong B. Current status and implications of virtual reality ecosystem. ICT & Media Policy 2016;28:1-23.
- de Vries AW, Willaert J, Jonkers I, et al. Virtual Reality Balance Games Provide Little Muscular Challenge to Prevent Muscle Weakness in Healthy Older Adults. Games Health J 2020;9:227-36. [Crossref] [PubMed]
- Baker R, Bell S, Baker E, et al. A randomized controlled trial of the effects of multi-sensory stimulation (MSS) for people with dementia. Br J Clin Psychol 2001;40:81-96. [Crossref] [PubMed]
- Verkaik R, van Weert JC, Francke AL. The effects of psychosocial methods on depressed, aggressive and apathetic behaviors of people with dementia: a systematic review. Int J Geriatr Psychiatry 2005;20:301-14. [Crossref] [PubMed]
- Sánchez A, Millán-Calenti JC, Lorenzo-López L, et al. Multisensory stimulation for people with dementia: a review of the literature. Am J Alzheimers Dis Other Demen 2013;28:7-14. [Crossref] [PubMed]
- Levin MF. Can virtual reality offer enriched environments for rehabilitation? Expert Rev Neurother 2011;11:153-5. [Crossref] [PubMed]
- Collins KM, Onwuegbuzie A, Jiao QG. A mixed methods investigation of mixed methods sampling designs in social and health science research. Journal of Mixed Methods Research 2007;1:267-94. [Crossref]
- Zhu S, Sui Y, Shen Y, et al. Effects of Virtual Reality Intervention on Cognition and Motor Function in Older Adults With Mild Cognitive Impairment or Dementia: A Systematic Review and Meta-Analysis. Front Aging Neurosci 2021;13:586999. [Crossref] [PubMed]
- Hodge J, Balaam M, Hastings S, et al. Exploring the design of tailored virtual reality experiences for people with dementia. Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems; 2018.
- Kim JH, Park S, Lim H. Developing a virtual reality for people with dementia in nursing homes based on their psychological needs: a feasibility study. BMC Geriatr 2021;21:167. [Crossref] [PubMed]
- Bimberg P, Weissker T, Kulik A. On the usage of the simulator sickness questionnaire for virtual reality research. In: 2020 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW); 2020 Mar 22–26; Atlanta, GA.
- Kennedy RS, Lane NE, Berbaum KS, et al. Simulator sickness questionnaire: An enhanced method for quantifying simulator sickness. Int J Aviat Psychol 1993;3:203-20. [Crossref]
- Stanney KM, Kennedy RS, Drexler JM. Cybersickness is not simulator sickness. Proc Hum Fact Ergon Soc Annu Meet 1997;41:1138-42.
- Kim TH, Jhoo JH, Park JH, et al. Korean version of mini mental status examination for dementia screening and its' short form. Psychiatry Investig 2010;7:102-8. [Crossref] [PubMed]
- Lee JH, Lee KU, Lee DY, et al. Development of the Korean version of the Consortium to Establish a Registry for Alzheimer’s Disease Assessment Packet (CERAD-K): clinical and neuropsychological assessment batteries. J Gerontol B Psychol Sci Soc Sci 2002;57:47-53. [Crossref] [PubMed]
- Ku HM, Kim JH, Kwon EJ, et al. A study on the reliability and validity of Seoul-Instrumental Activities of Daily Living (S-IADL). J Korean Neuropsychiatr Assoc 2004;43:189-99.
- Jackson-Koku G. Beck Depression Inventory. Occup Med (Lond) 2016;66:174-5. [Crossref] [PubMed]
- Williams AK. Motivation and dementia. Topics in Geriatric Rehabilitation 2005;21:123-6. [Crossref]
- Manera V, Petit PD, Derreumaux A, et al. 'Kitchen and cooking,' a serious game for mild cognitive impairment and Alzheimer's disease: a pilot study. Front Aging Neurosci 2015;7:24. [Crossref] [PubMed]
- Papaioannou T, Voinescu A, Petrini K, et al. Efficacy and Moderators of Virtual Reality for Cognitive Training in People with Dementia and Mild Cognitive Impairment: A Systematic Review and Meta-Analysis. J Alzheimers Dis 2022;88:1341-70. [Crossref] [PubMed]
- Tang YM, Chau KY, Kwok APK, et al. A systematic review of immersive technology applications for medical practice and education - trends, application areas, recipients, teaching contents, evaluation methods, and performance. Educ Res Rev 2021;35:100429. [Crossref]
- Fong KN, Tang YM, Sie K, et al. Task-specific virtual reality training on hemiparetic upper extremity in patients with stroke. Virtual Reality 2022;26:453-64. [Crossref]
- Crosbie JH, Lennon S, McNeill MD, et al. Virtual reality in the rehabilitation of the upper limb after stroke: the user's perspective. Cyberpsychol Behav 2006;9:137-41. [Crossref] [PubMed]
- Huygelier H, Schraepen B, van Ee R, et al. Acceptance of immersive head-mounted virtual reality in older adults. Sci Rep 2019;9:4519. [Crossref] [PubMed]
- Merhi O, Faugloire E, Flanagan M, et al. Motion sickness, console video games, and head-mounted displays. Hum Factors 2007;49:920-34. [Crossref] [PubMed]
- Lee SH, Jung HY, Yun SJ, et al. Upper Extremity Rehabilitation Using Fully Immersive Virtual Reality Games With a Head Mount Display: A Feasibility Study. PM R 2020;12:257-62. [Crossref] [PubMed]
- Coyle H, Traynor V, Solowij N. Computerized and virtual reality cognitive training for individuals at high risk of cognitive decline: systematic review of the literature. Am J Geriatr Psychiatry 2015;23:335-59. [Crossref] [PubMed]
- Liao YY, Chen IH, Lin YJ, et al. Effects of Virtual Reality-Based Physical and Cognitive Training on Executive Function and Dual-Task Gait Performance in Older Adults With Mild Cognitive Impairment: A Randomized Control Trial. Front Aging Neurosci 2019;11:162. [Crossref] [PubMed]
- Mahurin RK, Velligan DI, Hazleton B, et al. Trail making test errors and executive function in schizophrenia and depression. Clin Neuropsychol 2006;20:271-88. [Crossref] [PubMed]
- Sánchez-Cubillo I, Periáñez JA, Adrover-Roig D, et al. Construct validity of the Trail Making Test: role of task-switching, working memory, inhibition/interference control, and visuomotor abilities. J Int Neuropsychol Soc 2009;15:438-50. [Crossref] [PubMed]
- Budson AE, Solomon PR. Memory loss, Alzheimer's disease, and dementia: a practical guide for clinicians. 3rd ed. Philadelphia, PA: Elsevier; 2021.
- Llinàs-Reglà J, Vilalta-Franch J, López-Pousa S, et al. The Trail Making Test. Assessment 2017;24:183-96. [Crossref] [PubMed]
- Thapa N, Park HJ, Yang JG, et al. The Effect of a Virtual Reality-Based Intervention Program on Cognition in Older Adults with Mild Cognitive Impairment: A Randomized Control Trial. J Clin Med 2020;9:1283. [Crossref] [PubMed]
- Goodall G, Ciobanu I, Broekx R, et al. Using adaptive immersive environments to stimulate emotional expression and connection in dementia care: insights from user perspectives towards SENSE-GARDEN. In: Folds DJ, Berndt JO, editors. HUSO 2018: Fourth International Conference on Human and Social Analytics; 2018 Jun 24-28; Venice (IT). Red Hook, NY: Curran Associates; 2018: 37-42.
- Yun SJ, Kang MG, Yang D, et al. Cognitive Training Using Fully Immersive, Enriched Environment Virtual Reality for Patients With Mild Cognitive Impairment and Mild Dementia: Feasibility and Usability Study. JMIR Serious Games 2020;8:e18127. [Crossref] [PubMed]
- D'Cunha NM, Nguyen D, Naumovski N, et al. A Mini-Review of Virtual Reality-Based Interventions to Promote Well-Being for People Living with Dementia and Mild Cognitive Impairment. Gerontology 2019;65:430-40. [Crossref] [PubMed]


