
Effect of plan-do-check-active method combined with air pressure wave therapy on the prevention of deep venous thrombosis in critically ill patients in neurosurgery
Introduction
Compared with patients in other departments, critically ill patients in neurosurgery are in a more serious condition that progresses rapidly, changes rapidly, prolongs bed rest and results in a longer recovery period. Recently, increased numbers of traffic accidents, and high-altitude operations, in China has led to increased numbers of patients in neurosurgical Intensive Care Unit (ICU), with implications for their physical and mental health and quality of life (QOL) (1-3). The prolonged bed rest and high volumes of fluid therapy result in abnormal hemorheology and increased risk of postoperative deep vein thrombosis (DVT) (4,5), which can seriously affect the patient’s recovery, causing limb pain, swelling, and increased skin temperature (6-8). Without timely treatment, DVT has many adverse events, and can affect the recovery of activities of daily living (ADL) (9,10). In severe cases, life-threatening pulmonary embolism (PE) can occur (11). The development of DVT in a critically ill patient in neurosurgery results in prolonged hospital stay, increased treatment costs, and increased financial and psychological burden on both the patient and the family (12,13).
The short-term goal of thrombolysis is to prevent rapid growth of the thrombus, and the long-term goal is to prevent both DVT recurrence and PE, as well as preventing DVT complications such as post-venous thromboembolism syndrome (14). The commonly used clinical thrombolytic treatments include physical thrombolytic therapy, oral anticoagulant, heparin therapy, direct thrombolytic therapy with percutaneous catheterization, and surgical thrombectomy (15-18). Physical therapy includes graded compression stockings or intermittent air pressure therapy and exercises to reduce pain and swelling (19). Anticoagulant therapy mainly includes anticoagulants (such as aspirin and warfarin), low-dose common heparin, and low-molecular-weight (LMW) heparin (such as enoxaparin and sodium dalteparin). LMW heparin has become the recognized drug of choice for anticoagulation treatment and prevention of DVT in the lower limbs, because compared with unfractionated heparin, it has less bleeding risk, does not require routine testing, is not metabolized by the liver, so can be used by patients with liver disease and in special populations such as pregnant women, newborns, and children (20-24).
The clinical characteristics of DVT and the particularity of treatment determine the main goal is prevention. Therefore, correct understanding of the causes of postoperative DVT and taking active and effective preventive and nursing measures are the key to preventing DVT (25-27). The Plan-Do-Check-Action (PDCA) approach is a quality management cycle program devised in the USA. PDCA processes the results of the summary inspection, affirms successful experiences and appropriately promotes and standardizes them, summarizes the lessons of failure, and puts unresolved problems into the next PDCA cycle. These four processes do not end after the initial cycle, but are carried out repeatedly, because as one cycle completes, some problems are solved, and the unresolved problems enter the next cycle. The essence and core are to achieve continuous quality improvement (28,29). Air wave pressure therapy instrument is a kind of physical therapy, mainly through the sequence of repeated filling and deflating of the multi-chamber air bag, the formation of circulation pressure to the limbs and tissues. It should evenly and orderly squeeze the distal end of the limb to the proximal end of the limb, promote the flow of blood and lymph and improve the microcirculation, accelerate the fluid reflux of the limb tissue. It is helpful to prevent the formation of thrombosis, prevent limb edema, and directly or indirectly treat many diseases related to hemolymph circulation. This is due to the effect of passive and uniform massage, with the acceleration of blood circulation, which can accelerate the absorption of metabolic waste in the blood, inflammatory factors, and pain factors. It can prevent muscle atrophy, prevent muscle fibrosis, strengthen the oxygen content of the limbs, and help to solve the diseases caused by blood circulation disorders (such as bone femoral head ring death, etc.) (30).
We analyzed the preventive effect of PDCA combined with air pressure wave (APW) therapy on the development of DVT in critically ill neurosurgical patients to provide a reference for ensuring their QOL. We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1198/rc).
Methods
Research subjects
We enrolled 98 critically ill patients in neurosurgery who were admitted to the Huizhou Municipal Central Hospital between January 2020 and June 2021. The study design was described as follows. All patients were given routine nursing, including condition observation, medication guidance, specialist nursing and psychological nursing, etc. At the same time, PDCA cycle nursing and treatment were carried out. On the basis of PDCA cycle treatment, air pressure wave treatment was carried out. This work was conducted in accordance with the Declaration of Helsinki (revised in 2013). This work was approved by the Medical Ethics Committee of Huizhou Municipal Central Hospital (No. kyll2021102). Informed consent was obtained from all patients or their next of kin. In the work, the purpose, process, precautions, and legitimacy of the study were explained specifically for the patients. No harm to patients was guaranteed during the study. In addition, the research subjects and private data obtained were confidential and were only for research use, and may not be used for other purposes.
The inclusion criteria were: Glasgow Coma Scale score of 5–10 points; traumatic brain injury; age <70 years; diagnosed by magnetic resonance imaging and computerized tomography.
The exclusion criteria were: intracranial tumor, multiple organ failure, hematological disease; unstable hypertension and pulmonary edema; unable to tolerate APW therapy.
PDCA
PDCA involved setting up an intervention team, assessment of nursing staff for operation of the APW therapy instrument, knowledge of neurosurgery-related nursing, and formulation of nursing procedures, evaluation standards, supervision and evaluation systems, and work systems according to the patient’s condition, and regular meetings at which the data and suggestions provided by the nursing staff were discussed to determine the best solution for patients prone to infection or DVT and other related factors. Implementation of the solutions was regularly checked, evaluated, and summarized for timely correction. The health status of the nursing and medical staff was evaluated in accordance with relevant implementation standards to ensure strict implementation of nursing measures, reduction of related risk factors, and delivery of quality nursing. Finally, the inspection results of each link and each stage were summarized, existing problems were analyzed, and solutions and prevention measures sought. Unresolved or newly discovered problems become the target of the next round of PDCA to lower the incidence of DVT.
APW therapy
The role of APW therapy and its significance in preventing DVT was explained in detail to each patient. While lying supine on the treatment bed, the patient’s affected limb was placed in the isolation sleeve and the pressure adjusted according to the patient’s body condition and tolerance (usually 60–80 mmHg). The recommended treatment was 30 min/time, twice daily, for a total of 14 days.
Indicators of DVT development
Related indicators of coagulation (prothrombin time, fibrinogen, and thrombin time), and hemorheology [plasma viscosity, high and low blood viscosity (HBV, LBV)], circumference of lower limb (15 cm above and below patella), and Barthel index (BI) score were measured before and after the intervention and any changes were analyzed.
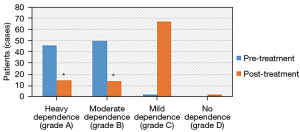
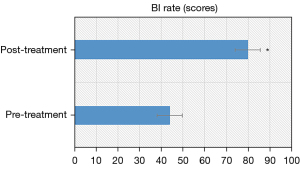
The coagulation and hemorheological indicators in fasting venous blood (5 mL) were measured by the respective automated analyzers according to the manufacturer’s instructions. The circumference of the lower limb at 15 cm above and below the patella was measured with a soft ruler. The BI score was used to assess the ADL of the patient in terms of eating, bathing, grooming, dressing, toilet habits, bed and chair transfer, walking on the ground, and going up and down stairs, with a total score of 100 points. The patient’s self-care ability was divided into four levels: severe dependence A (<40 points), moderate dependence B (41–60 points), mild dependence C (61–99 points), and no dependence D (100 points). DVT was determined by vascular Doppler ultrasound.
Statistical analysis
All experimental data were statistically analyzed by SPSS 24.0 software. Measurement data were expressed as mean ± standard deviation (), and enumeration data were statistically inferred using the χ2 test. Measurement data were in line with normal distribution, and t-test was used. Statistical significance was defined as P<0.05.
Results
Clinical baseline characteristics of the patients
The baseline clinical characteristics of all patients tested were shown in Table 1.
Table 1
| Clinical features | Patients |
|---|---|
| Duration of disease (years), Mean ± SD | 5.73±2.62 |
| Cerebral hemorrhage patient, N | 33 |
| Patients with cerebral infarction, N | 41 |
| Hemiplegic (left/right/bilateral), N | 20 (7/11/2) |
| Patients with hypertension, N | 79 |
| Patients with diabetes, N | 62 |
| Patients with hyperlipidemia, N | 43 |
Coagulation indicators
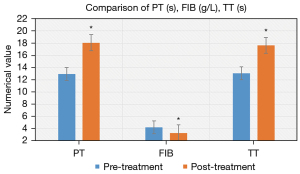
The prothrombin and thrombin times of the patients after treatment were 18.09 s and 17.66 s, respectively, which were much higher than before treatment. In addition, the fibrinogen level was lower, and there was a significant statistical difference compared with before treatment (P<0.05). The specific results are shown in Figure 1.
Hemorheology indicators
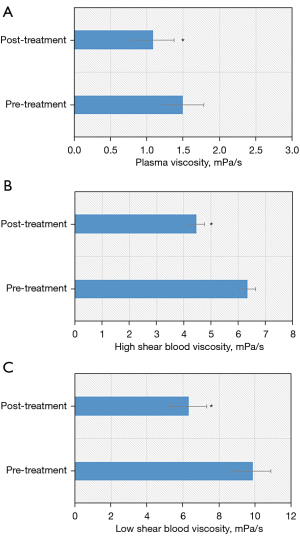
Plasma viscosity, HBV, and LBV of the patients after treatment were all reduced compared with before treatment, with statistical difference (P<0.05). The specific results are shown in Figure 2.
Circumference of the lower limb
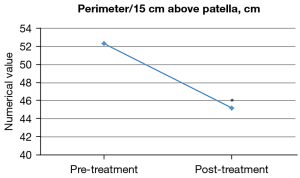
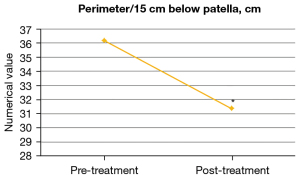
After PDCA combined with APW therapy, the circumference of lower limb was significantly reduced (P<0.05). The specific results are shown in Figures 3,4.
BI scores
According to the BI scores, the number of patients in severe dependence (grade A) and moderate dependence (grade B) after treatment was greatly reduced (P<0.05). In addition, the average BI score after the combined therapy was much higher compared with before treatment (P<0.05). The specific results are shown in Figures 5,6.
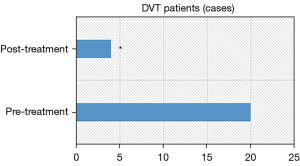
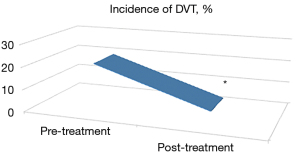
Change in the incidence of DVT
The number of people developing DVT and the incidence of DVT decreased after PDCA combined with APW therapy, with significant statistical difference (P<0.05). The specific results are illustrated in Figures 7,8.
Discussion
Patients in the neurosurgical ICU are seriously ill, requiring prolonged bed rest and recovery that results in abnormal hemorheological status and susceptibility to DVT. Active and effective prevention and care measures are the key to clinical prevention and treatment of DVT. In modern medicine, there are higher requirements for the quality of services, not only to have better treatments, but also to strengthen nursing interventions, which requires clinical nursing to strengthen management measures (31). The application of PDCA in the nursing care of critically ill neurosurgical patients can change the traditional modes of working. Through scientific planning and process control, the influence of various risk factors can be avoided. Based on continuous improvement of nursing measures, PDCA can effectively improve the quality of clinical care, thus reducing the occurrence of both nosocomial infections and DVT, which has great significance for improving the prognosis (32). APW therapy stimulates muscle contraction through the intermittent pressure and decompression process, which accelerates blood flow and increases the shear force on blood vessel walls, leading to upregulation of nitric oxide (NO) synthesis and release. NO expands blood vessels, promotes the microcirculation, and improves hemorheology (33).
We analyzed the preventive effect of combining PDCA with APW therapy on DVT incidence in the neurosurgical ICU. A previous study has shown that PDCA management can reduce the risk of infections and improve the prognosis of patients (34), which is consistent with the results of this study. In addition, the combined approach effectively restored the ability of patients to perform ADL, which can encourage patients to return to normal social and family life as soon as possible, lessening the physical and mental burden, and improving outcomes.
Conclusions
The limitation of this study was that small sample size in a single center may restrict the applicability of the results. In subsequent studies, multiple centers, multiple types of patients, and large sample sizes should be considered, and a control group should be set up for comparative analysis. However, this study has provided a practical and effective reference for the application of PDCA combined with APW in the prevention and treatment of DVT in critically ill neurosurgical patients.
Acknowledgments
Funding: This work was supported by the 2021 Huizhou Science and Technology Research and Development Program (self-funded by the medical and health sector) (Project No. 2021 WC0106442).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1198/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1198/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1198/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This work was conducted in accordance with the Declaration of Helsinki (revised in 2013). This work was approved by the Medical Ethics Committee of Huizhou Municipal Central Hospital (No. kyll2021102), and informed consent was obtained from all patients or their next of kin.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Goeren D, John S, Meskill K, et al. Quiet Time: A Noise Reduction Initiative in a Neurosurgical Intensive Care Unit. Crit Care Nurse 2018;38:38-44. [Crossref] [PubMed]
- Altun Ugras G, Yüksel S, Isik MT, et al. Effect of abdominal massage on bowel evacuation in neurosurgical intensive care patients. Nurs Crit Care 2022;27:558-66. [Crossref] [PubMed]
- Podkovik S, Toor H, Gattupalli M, et al. Prevalence of Catheter-Associated Urinary Tract Infections in Neurosurgical Intensive Care Patients - The Overdiagnosis of Urinary Tract Infections. Cureus 2019;11:e5494. [Crossref] [PubMed]
- Kruger PC, Eikelboom JW, Douketis JD, et al. Deep vein thrombosis: update on diagnosis and management. Med J Aust 2019;210:516-24. [Crossref] [PubMed]
- Zhang Y, Xia H, Wang Y, et al. The rate of missed diagnosis of lower-limb DVT by ultrasound amounts to 50% or so in patients without symptoms of DVT: A meta-analysis. Medicine (Baltimore) 2019;98:e17103. [Crossref] [PubMed]
- Diana Yap FS, Ng ZY, Wong CY, et al. Appropriateness of deep vein thrombosis (DVT) prophylaxis use among medical inpatients: a DVT risk alert tool (DRAT) study. Med J Malaysia 2019;74:45-50. [PubMed]
- Panpikoon T, Chuntaroj S, Treesit T, et al. Lower-Extremity Venous Ultrasound in DVT-Unlikely Patients with Positive D-Dimer Test. Acad Radiol 2022;29:S1076-6332(20)30406-2.
- Hansrani V, Khanbhai M, McCollum C. The Diagnosis and Management of Early Deep Vein Thrombosis. Adv Exp Med Biol 2017;906:23-31. [Crossref] [PubMed]
- Tarazi M, Bashir A, Khan K, et al. A Literature Review and Case Series of DVT Patients with Absent IVC Treated with Thrombolysis. Ann Vasc Surg 2020;67:S0890-5096(20)30258-2.
- Audu CO, Wakefield TW, Coleman DM. Pediatric deep venous thrombosis. J Vasc Surg Venous Lymphat Disord 2019;7:S2213-333X(19)30069-1.
- Plancher KD, Chan JJ, Bishai SK, et al. DVT and Pulmonary Embolism Following Knee Arthroscopy: The Role of Genetic Predisposition and Autoimmune Antibodies: A Report of 3 Cases. JBJS Case Connect 2020;10:e0514. [Crossref] [PubMed]
- Devis P, Knuttinen MG. Deep venous thrombosis in pregnancy: incidence, pathogenesis and endovascular management. Cardiovasc Diagn Ther 2017;7:S309-19. [Crossref] [PubMed]
- Sachdeva A, Dalton M, Lees T. Graduated compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev 2018;11:CD001484. [Crossref] [PubMed]
- Borsi SH, Khanjani N, Nejad HY, et al. Air pollution and hospital admissions due to deep vein thrombosis (DVT) in Ahvaz, Iran. Heliyon 2020;6:e04814. [Crossref] [PubMed]
- Wang H, Pei H, Ding W, et al. Risk factors of postoperative deep vein thrombosis (DVT) under low molecular weight heparin (LMWH) prophylaxis in patients with thoracolumbar fractures caused by high-energy injuries. J Thromb Thrombolysis 2021;51:397-404. [Crossref] [PubMed]
- Barrosse-Antle ME, Patel KH, Kramer JA, et al. Point-of-Care Ultrasound for Bedside Diagnosis of Lower Extremity DVT. Chest 2021;160:S0012-3692(21)01330-1.
- Sforza M, Husein R, Saghir R, et al. Deep Vein Thrombosis (DVT) and Abdominoplasty: A Holistic 8-Point Protocol-Based Approach to Prevent DVT. Aesthet Surg J 2021;41:NP1310-20. [Crossref] [PubMed]
- Zhang W, Huai Y, Wang W, et al. A Retrospective cohort study on the risk factors of deep vein thrombosis (DVT) for patients with traumatic fracture at Honghui Hospital. BMJ Open 2019;9:e024247. [Crossref] [PubMed]
- Mazetto BM, Orsi FLA, Silveira SAF, et al. Residual Vein Thrombosis Echogenicity Is Associated to the Risk of DVT Recurrence: A Cohort Study. Clin Appl Thromb Hemost 2018;24:477-82. [Crossref] [PubMed]
- Meng H, Zhu Y, Zhang J, et al. Incidence and risk factor for preoperative deep vein thrombosis (DVT) in isolated calcaneal fracture, a prospective cohort study. Foot Ankle Surg 2021;27:S1268-7731(20)30116-8.
- Kabashneh S, Singh V, Alkassis S. A Comprehensive Literature Review on the Management of Distal Deep Vein Thrombosis. Cureus 2020;12:e8048. [Crossref] [PubMed]
- Niu S, Li J, Zhao Y, et al. Preoperative deep venous thrombosis (DVT) after femoral neck fracture in the elderly, the incidence, timing, location and related risk factors. BMC Musculoskelet Disord 2021;22:264. [Crossref] [PubMed]
- Tamura S, Yamamoto M, Kitagawa A, et al. Deep Vein Thrombosis (DVT) Prophylactic Team Activity to Support DVT Prevention Protocol for the Purpose of the Prophylaxis of Pulmonary Thromboembolism (PTE) and Operation. Ann Vasc Dis 2021;14:99-107. [Crossref] [PubMed]
- Gambhir S, Inaba CS, Alizadeh RF, et al. Venous thromboembolism risk for the contemporary bariatric surgeon. Surg Endosc 2020;34:3521-6. [Crossref] [PubMed]
- The rate of missed diagnosis of lower-limb DVT by ultrasound amounts to 50% or so in patients without symptoms of DVT: A meta-analysis Medicine (Baltimore) 2019;98:e18469. Erratum. [Crossref] [PubMed]
- Baker M, Anjum F, dela Cruz J. Deep Venous Thrombosis Ultrasound Evaluation. In: StatPearls. Treasure Island (FL): StatPearls Publishing; June 19, 2022.
- Jorge A, Sanchez PG, Hayanga JWA, et al. Routine deep vein thrombosis screening after lung transplantation: Incidence and risk factors. J Thorac Cardiovasc Surg 2020;159:S0022-5223(19)31754-4.
- Hanawa T, Momo K. PDCA Cycle for the Development of Clinical Formulation Thinking in Actual Example. Yakugaku Zasshi 2019;139:1267-8. [Crossref] [PubMed]
- Wei Y, Xu M, Wang W, et al. Effect analysis of Plan-do-check-act cycle method applied in nursing management of disinfection supply room. Panminerva Med 2022;64:127-9. [Crossref] [PubMed]
- Hu H, Chen Y, Ye J, et al. Design of Treatment System for Poor Peripheral Circulation Using Air Wave Pressure Based on STM32 Microprocessor. Zhongguo Yi Liao Qi Xie Za Zhi 2020;44:42-6. [PubMed]
- Nielsen S Jr, O'Connor D, Kaul S, et al. Early Detection of Deep Venous Thrombosis in Trauma Patients. Cureus 2020;12:e9370. [Crossref] [PubMed]
- Leitmann A, Reinert S, Weise H. Surgical suture course for dental students with the Peyton-4-step approach versus the PDCA cycle using video assisted self-monitoring. BMC Oral Health 2020;20:365. [Crossref] [PubMed]
- Pawlowski C, Rincón-Hekking J, Awasthi S, et al. Cerebral Venous Sinus Thrombosis is not Significantly Linked to COVID-19 Vaccines or Non-COVID Vaccines in a Large Multi-State Health System. J Stroke Cerebrovasc Dis 2021;30:S1052-3057(21)00326-8.
- Hua G, Wang Q. Analysis of the application value of PDCA circulation in nursing management of disinfection and supply room. Minerva Surg 2022;77:294-6. [Crossref] [PubMed]


