
Need for inpatient rehabilitation and skilled nursing services in COVID-19 patients post hospitalization: a retrospective cohort study
Highlight box
Key findings
• A considerable number of patients hospitalized with COVID-19 needed skilled rehabilitation/nursing services post hospitalization. old age, male sex, longer hospital stays, and need for certain interventions or an acute stroke during admission, were the factors associated discharge to a facility post-hospitalization.
What is known and what is new?
• Need for rehabilitation and skilled nursing services for COVID-19 survivors has been speculated from the beginning of the pandemic. However, real-world data describing utilization of these services post COVID-19 hospitalization and factors associated with the same is limited. This study describes the utilization of inpatient rehabilitation/nursing services post-hospitalization among COVID-19 patients.
What is the implication, and what should change now?
• Knowledge regarding the utilization of skilled rehabilitation and nursing services post hospitalization in COVID-19 patients can facilitate efficient discharge planning and resource allocation. Such efforts can improve the long-term care of COVID-19 patients along with assisting in future pandemic preparedness.
Introduction
Coronavirus disease 2019 (COVID-19) has affected more than 560 million individuals globally and resulted in the loss of 6.37 million lives as of July 15, 2022 (1). The current global pandemic has impacted every aspect of human life. With numerous lockdowns, school shutdowns, travel bans, approval of vaccines, massive vaccination drives around the world, the urge to return to normalcy is ubiquitous. Much of the literature on the patients hospitalized with COVID-19 has focused on mortality and other severe disease outcomes such as intensive care admission and the need for mechanical ventilation (2-7). A relatively high number of patients hospitalized with COVID-19 require intensive care unit (ICU) admission and mechanical ventilation. The rates of mortality in hospitalized patients in the United States have been reported to be between 9.06% to 15.65% (8) and a study from the United Kingdom noted a reduction in mortality from 41.4% in March 2020 to 24.8% in June 2020 (9).
Studies have reported decreased in-hospital mortality, lower severity of disease, and a reduced need for ICU in the subsequent waves of the COVID-19 pandemic (10,11). The struggle of different nations with the immediate impact of the COVID-19 and the significant concern about the long-term morbidity in critically ill COVID-19 patients has been documented. Experts have been concerned about an increased probability of a high incidence of post-ICU morbidity in COVID-19 patients and the challenges in effective rehabilitation of these patients (12,13).
Since the beginning of the pandemic, it has been recognized that skilled rehabilitation services would play a vital role in assisting the individuals recovering from COVID-19 associated critical illness (14,15). Experts have speculated that skilled services would be required by COVID-19 survivors, especially those who needed hospitalization, to optimize functional independence and reintegration into the community (16). However, little data is available regarding the utilization of inpatient rehabilitation/skilled nursing services post COVID-19 hospitalization.
The current pandemic has severely strained the health care resources throughout the world, especially during the surges. During the second wave of COVID-19 in Michigan, rates of COVID-19 hospitalization increased from 4.5 per 100,000 population in early October 2020 to peak of 29.7 per 100,000 population in early December 2020, plateauing to 21 per 100,000 population in late March 2021 (17). Different health care settings responded to the pandemic by setting up temporary field hospitals and expanding the capacity of ICUs. However, there is minimal information regarding the ability of rehabilitation units to meet the increasing demand caused by COVID-19. A study from Italy highlights the increased costs of setting up a COVID-19 rehabilitation unit compared to the regular rehabilitation units (18) and noted better outcomes among COVID-19 patients admitted to rehabiliation units (19).
A number of COVID-19 vaccines are now available worldwide and in the United States the three major types of vaccines are messenger RNA (mRNA) vaccines, protein subunit vaccines and viral vector vaccines (20). Two dose mRNA vaccines have been shown to decrease risk of hospitalization by 85% for alpha and delta variants and 65% for the omicron variant (21). As of August 2022, 67.5% of the world population has received at least 1 dose of the COVID-19 vaccine and 12.51 billion doses have been administered globally (22). With effective vaccines and better understanding of the disease process resulting in reduced mortality from COVID-19, the focus is now shifting towards the development of more comprehensive treatment and rehabilitation plans for COVID-19 survivors to minimize the long-term effects of the infection (23-27).
The primary objective of this study was to identify the number of hospitalized COVID-19 patients who were discharged to inpatient rehabilitation or skilled nursing facilities following acute inpatient hospitalization during the second wave of the pandemic in the state of Michigan. The secondary aim was to explore the factors associated with discharge to a facility among the COVID-19 survivors who were living in their homes before hospitalization. We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-858/rc).
Methods
Study design
This was a retrospective cohort analysis conducted on 559 adult patients diagnosed and hospitalized with COVID-19 infection during the second wave of the pandemic in the state of Michigan. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Detroit Medical Center (DMC) and Wayne State University (WSU) Institutional Review Board (IRB application # 21-03-3286) and individual consent for this retrospective analysis was waived. All research was performed in accordance with the relevant guidelines/regulations. This study did not receive any funding from external resources.
Study site and patient population
This study was conducted on the data from two hospitals (Detroit Receiving Hospital and Harper University Hospital) in a large academic center, catering to an underserved, majority Black population. Study participants were adult patients (≥18 years of age) with a confirmed COVID-19 diagnosis who required hospitalization.
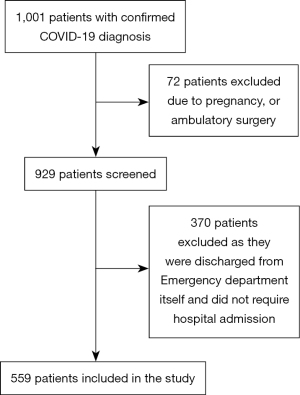
Data collection
A list of all consecutive adult hospitalized patients (n=1,001) with a laboratory confirmed COVID-19 diagnosis (by polymerase chain reaction) between October 1, 2020, and March 28, 2021 was collected. This period coincides with the second wave of the COVID-19 pandemic in the state of Michigan (28). During the initial period of this study (October 1, 2020 to mid-January, 2021) the original variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was predominant in Michigan. The first case of Alpha variant (B.1.1.7) in Michigan was identified on January 16, 2021. Thereby, the study includes the patients affected by original or alpha variant of the SARS-CoV-2 virus (29). All ambulatory surgery patients, pregnant patients and patients discharged from the emergency department (ED) itself (n=370) not requiring hospitalization were excluded from the study. A total of 559 patients were included in the study following these exclusions, as shown in Figure 1.
Data were collected and coded for all patients meeting the eligibility criteria via a review of each patient’s medical electronic medical records. Randomly selected patient charts were additionally verified by the principal investigator to ensure data integrity and accuracy. Variables collected from patient charts included age, sex, race, insurance status, body mass index (BMI), smoking status and comorbidities. The comorbidities (as defined in Table S1) included diabetes mellitus (DM), hypertension, coronary artery disease (CAD), congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), asthma, obstructive sleep apnea (OSA), chronic liver disease, chronic kidney disease (CKD), end stage renal disease (ESRD) on dialysis, human immunodeficiency virus (HIV), hyperlipidemia, history of cancer, and history of prior stroke.
Whenever available in the medical records, the time from the symptom onset to the day of presentation to the hospital was also noted for each patient. Days from the onset of symptoms to the presentation were classified as less than 5, 6–10,11–15, and 16 or more days. We also noted the setting that each patient presented to the ED from, i.e., home, inpatient rehabilitation facility (IRF), skilled nursing facility (SNF), long-term acute care (LTAC), or adult foster care (AFC). The clinical course and outcomes of the patient’s hospitalization were also noted. The CURB-65 score was calculated for each patient by using age, systolic and diastolic blood pressure, respiratory rate, blood urea nitrogen (BUN), confusion at the time of admission. CURB-65 is a clinical prediction score helpful in predicting mortality in patients with community acquired pneumonia. It is calculated based upon presence of the following: confusion, blood urea nitrogen >7 mmol/L, respiratory rate ≥30, blood pressure (systolic <90 mmHg or diastolic ≤60 mmHg) and age ≥65 years. Higher CURB-65 score indicates higher risk of mortality (30). Information regarding the need for a new tracheostomy, new percutaneous endoscopic gastrostomy (PEG) tube, new hemodialysis, or continuous renal replacement therapy (CRRT) during hospitalization was noted as well. It was also noted if the patient developed acute stroke during the course of hospitalization. Clinical variables were chosen based on the previous studies reporting the factors associated with COVID-19 clinical outcomes in the early part of the pandemic and common outcome measure set for COVID-19 clinical research proposed by World Health Organization (3-5,31-33). Mortality during hospitalization, need for mechanical ventilation, and ICU admission was also noted for each patient. It was also documented if the patient was transferred to another facility for extracorporeal membrane oxygenation (ECMO) therapy. The discharge notes were screened to note the discharge disposition for each patient. The discharge disposition for each patient hospitalized in our system is decided by a multi-disciplinary team consisting of the treating physician, physical therapist, occupational therapist, speech pathologist, case manager, social worker, and physiatrist as needed as per the Centers for Medicare and Medicaid Services guidelines for discharging patient to a facility (34). It was noted whether the patient was discharged to home, IRF, SNF, LTAC, or AFC. In a small number of patients for whom, the admission or discharge disposition could not be reliably collected from the records, it was mentioned as unknown. For the purpose of statistical regression model, a facility was defined as any setting excluding home, to where the patient was discharged because of the need for skilled nursing/rehabilitation services. A documented acute care endpoint (mortality/discharged status) was available for all patients included in the study at the time of data collection.
Statistical analysis
The continuous variables were tested for normal distribution using the Shapiro-Wilk test. All the continuous variables had non-normal distribution and have been described as the median and interquartile range (IQR) and the categorical variables as frequency and percentages. Descriptive data has been rounded off to one decimal place for ease of presentation. In the patients who presented from a home setting and survived hospitalization, binary logistic regression using the forced entry approach was conducted to identify the factors that had a significant association with the discharge to a facility. The variables included in the regression model were age, sex, race, days from symptom onset to presentation, BMI, CURB-65 score, smoking status, insurance, complications during admission (need for new PEG, tracheostomy, hemodialysis/CRRT, or new stroke during hospital stay), need for ICU or mechanical ventilation during admission, length of stay, comorbidities which include COPD, asthma, OSA, hypertension, HIV, CAD, DM, CKD, ESRD on dialysis, CHF, any cancer, chronic liver disease, hyperlipidemia and history of previous stroke. A 2-tailed P value <0.05 was considered to be significant. No imputations were done for the missing data since none of the variables were missing more than 5% of the values. IBM SPSS Statistics software (version 26) was used to do the analyses.
Results
Baseline characteristics
There were 559 hospitalized patients with a laboratory-confirmed COVID-19 diagnosis included in the study between October 1, 2020, and March 28, 2021, the period that coincided with the second wave of COVID-19 pandemic in the state of Michigan. The median age of the patients was 64 years (IQR 53–73 years). About 48.5% of the patients were males (n=271). More than 67.6% of the patients were Blacks (n=378), followed by Caucasians (16.8%, n=94) and Asians (5.0%, n=28). Close to 50% of the patients (n=277) were obese with a BMI of greater than 30 kg/m2. Hypertension (66.4%, n=371) was the most common comorbidity followed by DM (36.0%, n=201). More than 51% of the patients (n=287) had medicare insurance. Almost 73% patients (n=409) presented to the hospital within 5 days of the onset of symptoms. Around 85% (n=475) of the hospitalized patients were admitted to the hospital from home and around 12% (n=67) were transferred to the hospital from another facility [10.8% patients (n=59) from SNF, 0.5% (n=3) from IRF, 0.4% (n=2) from LTAC, and 0.5% (n=3) from AFC home]. Admission disposition (whether admitted from home or a facility) could not be reliably collected for 17 patients. Further details on baseline characteristics have been summarized in Table 1.
Table 1
| Characteristics | Total cohort (n=559) | Admitted from home (n=475) | Admitted from facility (n=67) |
|---|---|---|---|
| Age, (years) n (%) | |||
| Median [interquartile range] | 64 [53–73] | 62 [51–71] | 77 [68–86] |
| 18–30 | 24 (4.3) | 22 (4.6) | 0 |
| 31–45 | 64 (11.4) | 60 (12.6) | 0 |
| 46–64 | 218 (39.0) | 199 (41.9) | 12 (17.9) |
| ≥65 | 253 (45.3) | 194 (40.8) | 55 (82.1) |
| Sex, n (%) | |||
| Male | 271 (48.5) | 230 (48.4) | 31 (46.3) |
| Female | 288 (51.5) | 245 (51.6) | 36 (53.7) |
| Race/ethnicity, n (%) | |||
| Black | 378 (67.6) | 338 (71.2) | 33 (49.3) |
| Caucasian | 94 (16.8) | 56 (11.8) | 30 (44.8) |
| Asian | 28 (5.0) | 27 (5.7) | 0 |
| Middle Eastern | 25 (4.5) | 23 (4.8) | 1 (1.5) |
| Hispanic | 23 (4.1) | 22 (4.6) | 1 (1.5) |
| Cannot determine | 11 (2.0) | 9 (1.9) | 2 (3.0) |
| Body mass index, n (%) | |||
| Median (interquartile range) | 30.05 (25.2–36) | 30.4 (25.7–36.85) | 26.4 (23.1–31.28) |
| <18.5 (underweight) | 21 (3.8) | 15 (3.2) | 4 (6.0) |
| 18.5–24.9 (normal) | 106 (19.0) | 83 (17.5) | 18 (26.9) |
| 25–29.9 (overweight) | 146 (26.1) | 121 (25.5) | 21 (31.3) |
| ≥30 (obese) | 277 (49.6) | 250 (52.6) | 21 (31.3) |
| Missing | 9 (1.6) | 6 (1.3) | 3 (4.5) |
| Comorbidities, n (%) | |||
| Hypertension | 371 (66.4) | 310 (65.3) | 51 (76.1) |
| Diabetes mellitus | 201 (36.0) | 172 (36.2) | 27 (40.3) |
| Smoking | 186 (33.3) | 162 (34.1) | 17 (25.4) |
| Hyperlipidemia | 126 (22.5) | 102 (21.5) | 22 (32.8) |
| Coronary artery disease | 113 (20.2) | 89 (18.7) | 21 (31.3) |
| Chronic obstructive pulmonary disease | 86 (15.4) | 67 (14.1) | 14 (20.9) |
| Congestive heart failure | 82 (14.7) | 67 (14.1) | 13 (19.4) |
| Cancer | 66 (11.8) | 57 (12.0) | 9 (13.4) |
| Chronic kidney disease | 63 (11.3) | 55 (11.6) | 7 (10.4) |
| Asthma | 42 (7.5) | 41 (8.6) | 0 |
| Stroke | 41 (7.3) | 32 (6.7) | 9 (13.4) |
| End stage renal disease on dialysis | 31 (5.5) | 29 (6.1) | 2 (3.0) |
| Obstructive sleep apnea | 30 (5.4) | 26 (5.5) | 3 (4.5) |
| Chronic liver disease | 12 (2.1) | 10 (2.1) | 1 (1.5) |
| Human immunodeficiency virus | 6 (1.1) | 6 (1.3) | 0 |
| Insurance, n (%) | |||
| Medicare | 287 (51.3) | 221 (46.5) | 60 (89.6) |
| Medicaid | 170 (30.4) | 159 (33.5) | 6 (9.0) |
| Private | 86 (15.4) | 81 (17.1) | 1 (1.5) |
| Uninsured | 16 (2.9) | 14 (2.9) | 0 |
| Days from symptom onset to hospital presentation, n (%) | |||
| 0–5 | 409 (73.2) | 341 (71.8) | 55 (82.1) |
| 6–10 | 114 (20.4) | 104 (21.9) | 7 (10.4) |
| 11–15 | 34 (6.1) | 28 (5.9) | 5 (7.5) |
| 16+ | 2 (0.4) | 2 (0.4) | 0 |
| CURB-65 at presentation, n (%) | |||
| 1 | 192 (34.3) | 179 (37.7) | 4 (6.0) |
| 2 | 169 (30.2) | 150 (31.6) | 13 (19.4) |
| 3 | 148 (26.5) | 119 (25.1) | 27 (40.3) |
| 4 | 43 (7.7) | 22 (4.6) | 21 (31.3) |
| 5 | 3 (0.5) | 1 (0.2) | 2 (3.0) |
| Cannot determine | 4 (0.7) | 4 (0.8) | 0 |
Clinical course of the patients
Of the total of 559 patients who were hospitalized, 113 (20.2%) were admitted straight to ICU from the ED while 446 (79.8%) were admitted to the inpatient floors. During hospitalization, another 41 patients from the medical floors were transferred to the ICU. A total of 154 patients (27.5%) needed ICU during their hospitalization and 103 (18.4%) patients needed mechanical ventilation. During the hospitalization, 14 (2.5%) patients had an acute stroke, while 9 (1.6%) patients required a new PEG tube. Around 1.4% (n=8) of the patients needed a new tracheostomy. More than 9% of the patients (n=52) were initiated on hemodialysis or CRRT during hospitalization. More than 73% (n=411) received corticosteroids during their hospitalization and 33.1% (n=185) received remdesivir. Further details on the clinical course of hospitalization have been summarized in Table 2.
Table 2
| Characteristics | Cohort (n=559) | Admitted from home (n=475) | Admitted from facility (n=67) |
|---|---|---|---|
| Mortality, n (%) | 97 (17.4) | 64 (13.5) | 30 (44.8) |
| Mechanical ventilation, n (%) | 103 (18.4) | 75 (15.8) | 25 (37.3) |
| ICU admission, n (%) | 154 (27.5) | 114 (24.0) | 35 (52.2) |
| Admission disposition, n (%) | |||
| Inpatient admission | 446 (79.8) | 397 (83.6) | 36 (53.7) |
| Direct ED to ICU admission | 113 (20.2) | 78 (16.4) | 31 (46.3) |
| Treatment during admission, n (%) | |||
| Corticosteroids | 411 (73.5) | 353 (74.3) | 49 (73.1) |
| Remdesivir | 185 (33.1) | 172 (36.2) | 12 (17.9) |
| Anticoagulation | 195 (34.9) | 162 (34.1) | 28 (41.8) |
| Antibiotics | 283 (50.6) | 232 (48.8) | 45 (67.2) |
| Tocilizumab | 1 (0.2) | 1 (0.2) | 0 |
| Complications during admission, n (%) | |||
| PEG tube | 9 (1.6) | 5 (1.1) | 4 (6.0) |
| Tracheostomy | 8 (1.4) | 6 (1.3) | 2 (3.0) |
| New HD or CRRT | 52 (9.3) | 36 (7.6) | 15 (22.4) |
| Stroke during admission | 14 (2.5) | 10 (2.1) | 4 (6.0) |
| Discharge disposition, n (%) | |||
| Home | 365 (65.3) | 359 (75.6) | 1 (1.5) |
| Skilled nursing facility | 51 (9.1) | 25 (5.3) | 25 (37.3) |
| Inpatient rehabilitation facility | 5 (0.9) | 2 (0.4) | 3 (4.5) |
| LTAC | 9 (1.6) | 8 (1.7) | 1 (1.5) |
| AFC home | 5 (0.9) | 1 (0.2) | 3 (4.5) |
| Transfer to another hospital for ECMO | 2 (0.4) | 1 (0.2) | 1 (1.5) |
| Death | 97 (17.4) | 64 (13.5) | 30 (44.8) |
| Unknown | 25 (4.5) | 15 (3.2) | 3 (4.5) |
ICU, intensive care unit; ED, emergency department; PEG, percutaneous endoscopic gastrostomy; HD, hemodialysis; CRRT, continuous renal replacement therapy; LTAC, long term acute care; AFC home, adult foster care home; ECMO, extracorporeal membrane oxygenation therapy.
Discharge disposition from the hospital
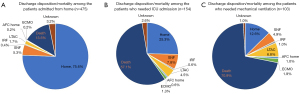
Around 17.4% of the patients (n=97) had in-hospital mortality. Close to 65% (n=365) of all the hospitalized COVID-19 patients were discharged home whereas 70 patients (12.5%) were discharged to a facility due to the need for inpatient rehabilitation or skilled nursing services. Only 2 patients required transfer to another medical facility for ECMO. About 9.1% of the patients (n=51) were discharged to SNF, 0.9% (n=5) to IRF, 1.6% (n=9) to LTAC, 0.9% (n=5) to AFC home and in 4.5% (n=25) the discharge disposition was missing from the clinical notes.
Of the 475 patients who presented to the hospital from home, only 75.6% (n=259) were discharged home. Approximately, only three out of every four COVID-19 patients who were hospitalized from home, were discharged back home. About 13.5 % of the patients died during hospitalization while 7.6% (n=36) required discharge to a facility due to the need for inpatient skilled rehabilitation or skilled nursing services and 1 patient required transfer to another medical facility for ECMO. About 5.3% of the patients admitted from home (n=25) were discharged to SNF, while 1.7% (n=8) were discharged to LTAC, and an additional 0.4% (n=2) were transferred to IRF (Figure 2A). Among patients who were admitted from a facility (n=67), approximately 44.8 % (n=30) died during hospitalization and 37.3% of the patients (n=25) required discharge to a SNF facility. Further details on the discharge disposition of the patients have been summarized in Table 2. Among the patients who required ICU admission, only 1 in every 4 patients were discharged home, 57.1% died, and the remaining were discharged to a facility (Figure 2B). Among the COVID-19 patients who needed mechanical ventilation, only about 1 in every 8 patients were discharged home from the hospital (Figure 2C).
In the logistic regression model of the patients who were living at home prior to hospitalization, older patients (OR, 1.07; 95% CI, 1.01–1.13; P=0.02), and those with a longer hospital stay (OR, 1.07; 95% CI, 1.04–1.11; P<0.001) were more likely to be discharged to a facility instead of home. For each additional day the patient needed to stay in the hospital, the odds of his discharge to a facility increased by 7%. Patients who experienced the need for a new PEG tube, tracheostomy, initiation of hemodialysis or CRRT or new stroke during admission were also more likely to be discharged to a facility post-hospitalization (OR, 15.25; 95% CI, 1.96–118.65; P=0.01). Female patients were less likely to be discharged to a facility compared to males (OR, 0.30; 95% CI, 0.10–0.86; P=0.03). These details have been summarized in Table 3.
Table 3
| Characteristic | OR (95% CI) | P value |
|---|---|---|
| Female sex | 0.30 (0.10–0.86) | 0.03 |
| Length of stay | 1.07 (1.04–1.11) | <0.001 |
| Age | 1.07 (1.01–1.13) | 0.02 |
| New PEG, tracheotomy, hemodialysis/CRRT or stroke during admission | 15.25 (1.96–118.65) | 0.01 |
Variables included in the model: age, sex, race, body mass index, insurance, days to presentation, CURB-65, smoking, complications during admission (need for new PEG, tracheostomy, hemodialysis/CRRT, new stroke at admission), need for ICU or mechanical ventilation during admission, length of stay, comorbidities which include COPD, asthma, OSA, hypertension, HIV, coronary artery disease, diabetes mellitus, chronic kidney disease, ESRD on dialysis, congestive heart failure, any cancer, chronic liver disease, hyperlipidemia and history of previous stroke. OR, odds ratio; CI, confidence interval; PEG, percutaneous endoscopic gastrostomy; CRRT, continuous renal replacement therapy; ICU, intensive care unit; COPD, chronic obstructive pulmonary disease; OSA, obstructive sleep apnea; HIV, human immunodeficiency virus; ESRD, end stage renal disease.
Discussion
In this study conducted at two hospitals of an inner-city academic medical center during the second wave of the pandemic, we noted that a considerable number of patients (12.5%) required inpatient rehabilitation or skilled nursing services post-hospitalization for COVID-19. Among the patients admitted from home, roughly only 3 in every 4 patients were discharged back home post-hospitalization. While a majority of the literature on COVID-19 presents data from the early part of the pandemic, this study reports mortality, severe disease outcomes as well as the need for inpatient skilled rehabilitation or nursing services during the second wave of COVID-19. Though the outcomes of hospitalized COVID-19 patients have been reported to be better during the subsequent waves of the pandemic (10), the findings of this study demonstrate that even during the second wave, more than a quarter of hospitalized COVID-19 patients needed ICU admission and roughly 1 in every 5 to 6 patients needed mechanical ventilation, which might have contributed to a significant number of patients needing inpatient rehabilitation/nursing services post-hospitalization. In a study conducted during the earlier part of the pandemic (March–June 2020) in New York (35), 5% of the patients were discharged to SNF compared to 9.1% of the patients in our cohort, whereas 6.8% were discharged to IRF compared to 0.9% in our cohort. This difference can, in part, be explained due to the executive orders in New York during the early part of the pandemic prohibiting the transfer of COVID-19 patients to SNF and expanded eligibility of the patients who could be transferred to IRF. In Michigan, however, per the executive orders, a long-term care facility could not prohibit admission or readmission of a resident based on COVID-19 testing requirements or results (36).
The findings of this study point to significant morbidity in COVID-19 patients post-discharge from the hospital and the need for continued inpatient skilled services at rehabilitation and nursing facilities, even during the second wave of the pandemic. Long COVID symptoms have been a burgeoning health concern for both hospitalized and non-hospitalized COVID-19 patients. A meta-analysis of the studies following up on the patient’s post-hospitalization for COVID-19 reported persistent breathlessness in 37% of patients and persistent fatigue in 52% of the patients 1–3 months post-discharge from the hospital (37). Another recent meta-analysis reported a wide spectrum of COVID-19 sequelae in previously hospitalized COVID-19 patients with symptoms like fatigue and sleeping disorders persisting up to a year (38). COVID-19 patients should have long-term access to multidisciplinary health care, including rehabilitation services post discharge (39). With the emergence of new variants and unrelenting burden of acute COVID-19 hospitalizations, despite advent of successful vaccination, consideration should be given to addressing the need for inpatient and subsequently outpatient rehabilitation facilities for optimal long-term care of COVID-19 patients. This study provides useful baseline information regarding the actual utilization of inpatient rehabilitation and skilled nursing facilities in COVID-19 and paves way for future research on allocation of resources in subsequent surges and for future pandemic preparedness.
This study also reports the factors associated with discharge to a facility in the patients who lived in their home before hospitalization for COVID-19. Among the COVID-19 survivors who presented to the hospital from home, older patients, males, and those with a longer length of stay in the hospital were more likely to be discharged to a facility, instead of home. The immobility associated with hospital stay has been linked to the loss of muscle mass, deterioration of the functional exercise capacity as well reduced endurance towards activities of daily living, especially in older individuals (40,41). This study also reports the data on the need for a new PEG tube, tracheostomy, initiation of hemodialysis or CRRT, and the occurrence of stroke during the admission in hospitalized COVID-19 patients. Patients who had either of these complications during the admission were 15 times more likely to be discharged to a facility. PEG tube placement has been reported to be an independent predictor for all-cause, unplanned hospital readmissions associated with reduced quality of life (42). To our knowledge, this is the first study reporting that 1.6% of all the hospitalized COVID-19 patients (n=9), or 5.2% of the critically ill COVID-19 patients needing ICU admission required a new PEG tube for enteral nutrition. A previous study from 2017 by Brodsky et al. (43) reported that roughly a third of patients experience dysphagia post-intubation after ARDS and dysphagia has been reported in 3% to 62% of the patients recovering after critical illness (44). About 45.6% (n=47) of the mechanically ventilated patients in our study cohort were initiated on hemodialysis or CRRT. Acute kidney injury has been reported very frequently (24–57%) among patients hospitalized with COVID-19 in the United States (3,45-47) and the study by Hirsch et al. (46) reported that 23.2% of mechanically ventilated patients required renal replacement therapy during their admission. About 2.5% of the patients in our study cohort developed stroke during admission. Ntaios et al. (48) reported that COVID-19 associated ischemic strokes are more severe with worse functional outcomes than non-COVID-19 ischemic strokes.
A recent large sample study reports that COVID-19 survivors are more likely to use healthcare resources, exhibit broad clinical manifestations, and have poor general wellbeing with a substantial burden of health loss. The risk and burden of post-acute sequelae were found to be higher in hospitalized COVID-19 patients (49). Improved quality of life and recovery of functional independence can be achieved in patients with Long COVID-19 syndrome by an early identification of the targeted populations needing rehabilitation services (50). Hence the knowledge of the factors associated with discharge to a facility can ensure efficient discharge planning to minimize the burden of permanent health loss in COVID-19 survivors.
There are some limitations of this study that need to be acknowledged. This study only looked at the patients discharged to inpatient nursing or rehabilitation facilities. Besides this, a significant number of patients who were discharged home might have also sought home-based or outpatient rehabilitation services, which were not explored in this study. Secondly, this study was conducted on the data from two hospitals serving the underserved population, limiting the generalization of the results. Moreover, there is a possibility that some of the patients who were recommended discharge to inpatient rehabilitation or skilled nursing facility might have refused the recommendation and chosen to be discharged home. Also, data on frailty and cognitive ability prior to admission and functional status at the time of discharge were not available. Lastly, during the surges, the discharge disposition might have also been affected by the availability of beds in the inpatient rehabilitation and nursing facilities. Large multicenter studies such as the ongoing CO-FLOW trials (51) are needed to identify the need and utilization of rehabilitation and nursing services among COVID-19 survivors, so that appropriate resources can be allocated to ensure the best long-term outcomes.
Conclusions
This study reports the number of patients admitted from home who needed discharge to a facility for inpatient rehabilitation/nursing services post-hospitalization for COVID-19. The information regarding utilization of these services can assist further research on appropriate resource allocation for future pandemic preparedness. Older patients, males and those with a longer hospital stay, along with the patients who needed a new PEG tube, tracheostomy, initiation of hemodialysis or CRRT, or had an acute stroke during the admission were more likely to require inpatient skilled services warranting discharge to a facility post-hospitalization. These findings can facilitate efficient discharge planning and help optimize the long-term care of COVID-19 survivors.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-858/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-858/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-858/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-858/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Detroit Medical Center (DMC) and Wayne State University Institutional Review Board (No. 21-03-3286), and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization [Internet]. WHO Coronavirus (COVID-19) Dashboard [cited 2022, July 15]. Available online: https://covid19.who.int
- Gupta S, Hayek SS, Wang W, et al. Factors Associated With Death in Critically Ill Patients With Coronavirus Disease 2019 in the US. JAMA Intern Med 2020;180:1436-47. [Crossref] [PubMed]
- Richardson S, Hirsch JS, Narasimhan M, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020;323:2052-9. [Crossref] [PubMed]
- Lohia P, Kapur S, Benjaram S, et al. Metabolic syndrome and clinical outcomes in patients infected with COVID-19: Does age, sex, and race of the patient with metabolic syndrome matter? J Diabetes 2021; Epub ahead of print. [Crossref] [PubMed]
- Lohia P, Sreeram K, Nguyen P, et al. Preexisting respiratory diseases and clinical outcomes in COVID-19: a multihospital cohort study on predominantly African American population. Respir Res 2021;22:37. [Crossref] [PubMed]
- Woolf SH, Chapman DA, Lee JH. COVID-19 as the Leading Cause of Death in the United States. JAMA 2021;325:123-4. [Crossref] [PubMed]
- Zhao Z, Chen A, Hou W, et al. Prediction model and risk scores of ICU admission and mortality in COVID-19. PLoS One 2020;15:e0236618. [Crossref] [PubMed]
- Asch DA, Sheils NE, Islam MN, et al. Variation in US Hospital Mortality Rates for Patients Admitted With COVID-19 During the First 6 Months of the Pandemic. JAMA Intern Med 2021;181:471-8. [Crossref] [PubMed]
- Dennis JM, McGovern AP, Vollmer SJ, et al. Improving Survival of Critical Care Patients With Coronavirus Disease 2019 in England: A National Cohort Study, March to June 2020. Crit Care Med 2021;49:209-14. [Crossref] [PubMed]
- Vahidy FS, Drews AL, Masud FN, et al. Characteristics and Outcomes of COVID-19 Patients During Initial Peak and Resurgence in the Houston Metropolitan Area. JAMA 2020;324:998-1000. [Crossref] [PubMed]
- Saito S, Asai Y, Matsunaga N, et al. First and second COVID-19 waves in Japan: A comparison of disease severity and characteristics. J Infect 2021;82:84-123. [Crossref] [PubMed]
- Tan SC, Haines K, Zhang N. Beyond the ventilator: Rehabilitation for critically ill patients with coronavirus disease 2019. Aust Crit Care 2020;33:485-7. [Crossref] [PubMed]
- Yu P, Wei Q, He C. Early Rehabilitation for Critically Ill Patients With COVID-19: More Benefits Than Risks. Am J Phys Med Rehabil 2020;99:468-9. [Crossref] [PubMed]
- Sheehy LM. Considerations for Postacute Rehabilitation for Survivors of COVID-19. JMIR Public Health Surveill 2020;6:e19462. [Crossref] [PubMed]
- Gutenbrunner C, Stokes EK, Dreinhöfer K, et al. Why Rehabilitation must have priority during and after the COVID-19-pandemic: A position statement of the Global Rehabilitation Alliance. J Rehabil Med 2020;52:jrm00081. [Crossref] [PubMed]
- Simpson R, Robinson L. Rehabilitation After Critical Illness in People With COVID-19 Infection. Am J Phys Med Rehabil 2020;99:470-4. [Crossref] [PubMed]
- Centers for Disease Control and Prevention [Internet]. COVID-NET A weekly summary of U.S. COVID-19 hospitalization data 2022 [cited 2022, January 11]. Available online: https://gis.cdc.gov/grasp/COVIDNet/COVID19_3.html
- Iannaccone S, Alemanno F, Houdayer E, et al. COVID-19 rehabilitation units are twice as expensive as regular rehabilitation units. J Rehabil Med 2020;52:jrm00073. [Crossref] [PubMed]
- Iannaccone S, Castellazzi P, Tettamanti A, et al. Role of Rehabilitation Department for Adult Individuals With COVID-19: The Experience of the San Raffaele Hospital of Milan. Arch Phys Med Rehabil 2020;101:1656-61. [Crossref] [PubMed]
- Centers for Disease Control and Prevention [Internet]. Overview of COVID-19 Vaccines. [cited 2022, August 24]. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/overview-COVID-19-vaccines.html
- Lauring AS, Tenforde MW, Chappell JD, et al. Clinical severity of, and effectiveness of mRNA vaccines against, covid-19 from omicron, delta, and alpha SARS-CoV-2 variants in the United States: prospective observational study. BMJ 2022;376:e069761. [Crossref] [PubMed]
- Our world in date [Internet]. Coronavirus (COVID-19) Vaccinations [cited 2022, August 25]. Available online: https://ourworldindata.org/covid-vaccinations
- National Institutes of Health [internet]. NIH launches new initiative to study “Long COVID” [cited 2022, August 20]. Available online: https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid
- Huang YZ, Kuan CC. Vaccination to reduce severe COVID-19 and mortality in COVID-19 patients: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci 2022;26:1770-6. [PubMed]
- Suthar AB, Wang J, Seffren V, et al. Public health impact of covid-19 vaccines in the US: observational study. BMJ 2022;377:e069317. [Crossref] [PubMed]
- Watson OJ, Barnsley G, Toor J, et al. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis 2022;22:1293-302. [Crossref] [PubMed]
- Fugazzaro S, Contri A, Esseroukh O, et al. Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int J Environ Res Public Health 2022; [Crossref] [PubMed]
- The New York Times [Internet]. Tracking Coronavirus cases in Michigan: Latest map and case count [cited 2021, July 10]. Available online: https://www.nytimes.com/interactive/2021/us/michigan-covid-cases.html
- Michigan Department of Health and Human Services [Internet]. MDHHS identifies first Michigan case of new COVID-19 variant, B.1.1.7. in Washtenaw County [cited 2022, August 21]. Available online: https://www.michigan.gov/coronavirus/news/2021/01/16/mdhhs-identifies-first-michigan-case-of-new-covid-19-variant-b-1-1-7--in-washtenaw-county
- Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax 2003;58:377-82. [Crossref] [PubMed]
- Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J Infect 2020;81:e16-25. [Crossref] [PubMed]
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020;323:1061-9. [Crossref] [PubMed]
- A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis 2020;20:e192-7. [Crossref] [PubMed]
- American Academy of Physical Medicine and Rehabilitation [Internet]. AAPM&R Post-Acute Care (PAC) Toolkit [cited 2022, August 27]. Available online: https://www.aapmr.org/quality-practice/aapm-r-post-acute-care-(pac)-toolkit/patient-eligibility
- Levin SR, Gitkind AI, Bartels MN. Effect of the COVID-19 Pandemic on Postacute Care Decision Making. Arch Phys Med Rehabil 2021;102:323-30. [Crossref] [PubMed]
- State of Michigan [Internet]. Enhanced protections for residents and staff of long-tern care facilities during the COVID-19 pandemic [cited 2021, december 12]. Available online: https://www.legislature.mi.gov/documents/2019-2020/executiveorder/pdf/2020-EO-191.pdf
- Cares-Marambio K, Montenegro-Jiménez Y, Torres-Castro R, et al. Prevalence of potential respiratory symptoms in survivors of hospital admission after coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Chron Respir Dis 2021;18:14799731211002240. [Crossref] [PubMed]
- Yang T, Yan MZ, Li X, et al. Sequelae of COVID-19 among previously hospitalized patients up to 1 year after discharge: a systematic review and meta-analysis. Infection 2022;50:1067-109. [Crossref] [PubMed]
- The Lancet. Facing up to long COVID. Lancet 2020;396:1861. [Crossref] [PubMed]
- Solverson KJ, Grant C, Doig CJ. Assessment and predictors of physical functioning post-hospital discharge in survivors of critical illness. Ann Intensive Care 2016;6:92. [Crossref] [PubMed]
- Pfoh ER, Wozniak AW, Colantuoni E, et al. Physical declines occurring after hospital discharge in ARDS survivors: a 5-year longitudinal study. Intensive Care Med 2016;42:1557-66. [Crossref] [PubMed]
- Wilmskoetter J, Simpson AN, Logan SL, et al. Impact of Gastrostomy Feeding Tube Placement on the 1-Year Trajectory of Care in Patients After Stroke. Nutr Clin Pract 2018;33:553-66. [Crossref] [PubMed]
- Brodsky MB, Huang M, Shanholtz C, et al. Recovery from Dysphagia Symptoms after Oral Endotracheal Intubation in Acute Respiratory Distress Syndrome Survivors. A 5-Year Longitudinal Study. Ann Am Thorac Soc 2017;14:376-83. [Crossref] [PubMed]
- Macht M, Wimbish T, Bodine C, et al. ICU-acquired swallowing disorders. Crit Care Med 2013;41:2396-405. [Crossref] [PubMed]
- Fisher M, Neugarten J, Bellin E, et al. AKI in Hospitalized Patients with and without COVID-19: A Comparison Study. J Am Soc Nephrol 2020;31:2145-57. [Crossref] [PubMed]
- Hirsch JS, Ng JH, Ross DW, et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int 2020;98:209-18. [Crossref] [PubMed]
- Chan L, Chaudhary K, Saha A, et al. AKI in Hospitalized Patients with COVID-19. J Am Soc Nephrol 2021;32:151-60. [Crossref] [PubMed]
- Ntaios G, Michel P, Georgiopoulos G, et al. Characteristics and Outcomes in Patients With COVID-19 and Acute Ischemic Stroke: The Global COVID-19 Stroke Registry. Stroke 2020;51:e254-8. [Crossref] [PubMed]
- Al-Aly Z, Xie Y, Bowe B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 2021;594:259-64. [Crossref] [PubMed]
- Yan Z, Yang M, Lai CL. Long COVID-19 Syndrome: A Comprehensive Review of Its Effect on Various Organ Systems and Recommendation on Rehabilitation Plans. Biomedicines 2021; [Crossref] [PubMed]
- Bek LM, Berentschot JC, Hellemons ME, et al. CO-FLOW: COvid-19 Follow-up care paths and Long-term Outcomes Within the Dutch health care system: study protocol of a multicenter prospective cohort study following patients 2 years after hospital discharge. BMC Health Serv Res 2021;21:847. [Crossref] [PubMed]


