
Palliative surgery for malignant superior vena cava obstruction resistant to immunotherapy: a case report
IntroductionOther Section
A disease progression pattern in a limited number of sites, called oligoprogression, is relatively common in non-small cell lung cancer (NSCLC) patients during immune checkpoint inhibitor (ICI) treatments (1,2). Continuing ICI treatments beyond progressive disease (PD) is an effective treatment option in NSCLC patients with absence of tumor progression at critical anatomical sites (3,4). However, it is controversial how to manage clinically problematic oligoprogressive lesions, such as superior vena cava (SVC) obstruction during ICI treatments.
Here, we report a case that continuing ICI treatment after palliative surgery for a malignant SVC obstruction that was resistant to ICI led to long-term survival without disease progression. We present the following case in accordance with the CARE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-839/rc).
Case presentationOther Section
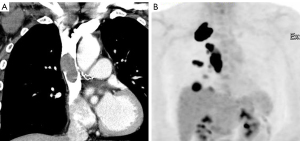
A 43-year-old man with a history of smoking presented with facial swelling and pain in the right shoulder. Contrast-enhanced computed tomography (CT) revealed a tumor (40×40 mm) at the apex of the right lung, pulmonary and pleural nodules, and swollen mediastinal lymph nodes. A swollen mediastinal lymph node directly invaded into the SVC (Figure 1A). 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) revealed FDG uptake in these lesions (Figure 1B). Pathological diagnosis with endobronchial ultrasound-guided transbronchial needle aspiration of the #4R lymph node revealed adenocarcinoma. On the basis of these findings, the patient was diagnosed with lung adenocarcinoma with SVC obstruction (cT3N2M1c; stage IVB). Next generation sequencing revealed negative results for all driver oncogenes. The programmed cell death ligand-1 (PD-L1) tumor proportion score was <1%.
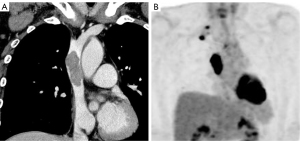
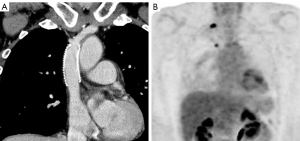
Treatment with carboplatin, pemetrexed, and pembrolizumab was initiated as the first-line chemotherapy. The size of the primary tumor, pulmonary and pleural metastases, and most mediastinal lymph node metastases reduced after four cycles of treatment, but only one lesion invading the SVC increased (Figure 2A). FDG-PET also showed increased FDG accumulation in only one lesion invading the SVC (Figure 2B). The pain in the right shoulder improved with the shrinking of the primary tumor, but facial swelling did not improve. Therefore, surgical resection of the lesion and vascular replacement were performed (Figure 3A,3B). The surgery was performed under general anesthesia and cardiopulmonary bypass, using propofol for sedation, remifentanil for analgesia, and rocuronium for relaxation. There were no differences in pathological findings and PD-L1 tumor proportion score (TPS) between the endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) and surgically resected samples. The facial swelling improved soon after surgery. Edoxaban (60 mg/day), an anticoagulant, was initiated postoperatively to prevent prosthetic graft occlusion. Since other tumor lesions continued to shrink, first-line chemotherapy was continued after surgery. At present, 22 months have passed since the surgery, and maintenance therapy with pemetrexed and pembrolizumab is ongoing, without disease progression nor any adverse events.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
DiscussionOther Section
A disease progression pattern in a limited number of sites, called oligoprogression, occurs in approximately 20–40% of NSCLC patients during immunotherapy and is associated with longer overall survival than systemic progression (1,2). As only one tumor invading the SVC increased and other lesions were reduced with immunotherapy, in our case, the progression pattern fitted the definition of oligoprogression. Appropriate management of oligoprogression during ICI treatment is extremely important for achieving long-term survival in NSCLC patients.
Recently, ICI treatments beyond PD have been shown to be effective in NSCLC patients with a stable performance status and absence of tumor progression at critical anatomical sites (3,4). Furthermore, when a limited number of tumor sites increase during ICI treatments, continuing immunotherapy following local therapy for such lesions can result in prolonged benefits (5). A recent study showed that neoadjuvant immunotherapy did not impede the feasibility of surgery and resulted in good clinical outcomes; nevertheless, eligible patients had resectable NSCLC (6). Therefore, surgical resection of an oligoprogressive lesion during immunotherapy may be a reasonable management option for local therapy.
The clinical course of the present case suggests that palliative surgery may be an effective management option for a clinically problematic lesion, such as SVC obstruction, which increases during immunotherapy. Although local therapies for SVC obstruction, such as stent insertion, radiotherapy, and surgical resection, or regimen change as second-line chemotherapy were considered management candidates in our case, surgical resection of the lesion causing SVC obstruction was selected for the following reasons. First, stent insertion was expected to provide only temporary relief of SVC obstruction. Although stent insertion is an effective and less-invasive management option for malignant SVC obstruction, re-obstruction remains a concern (7). In this particular case, since the tumor invading the SVC increased in size despite of the chemotherapy, surgical resection was considered more likely to achieve reliable and long-term relief of SVC obstruction. Second, intrathoracic radiotherapy could not be selected actively owing to concerns of pulmonary toxicity as the patient was undergoing immunotherapy. Intrathoracic radiotherapy was also considered as a local therapy for SVC obstruction, since the irradiation area would have been mainly in the mediastinum and the effects on the lung would be minimal. However, the safety of intrathoracic radiotherapy during immunotherapy remains unknown. Furthermore, inadequate response or recurrence occur with radiotherapy in some cases (7,8). Third, continuing immunotherapy seemed to be better than changing the regimen to achieve long-term survival, as other lesions, except for the one causing SVC obstruction, were reduced by the on-going immunotherapy regimen. Therefore, we decided to resect the lesion causing SVC obstruction and subsequently continue immunotherapy, which led to long-term survival without disease progression.
SVC obstruction due to malignancies has historically been considered an emergent condition; therefore, immediate radiotherapy was considered necessary for obstruction relief. However, recent guidelines recommend that stent insertion, radiotherapy, or chemotherapy should be considered in lung cancer patients with SVC obstruction, depending on the histopathological results (8). In the era of ICIs, immunotherapy combined with cytotoxic chemotherapy may be an effective treatment option for lung cancer patients with SVC obstruction, since it has a better response rate than conventional chemotherapy (9). In fact, a previous report showed that immunotherapy combined with cytotoxic chemotherapy was effective for such a patient (10). Surgical resection should be considered an effective local therapy when a clinically problematic lesion, such as SVC obstruction, is resistant to immunotherapy, as in the present case. It is important to discuss the appropriate treatment with a multidisciplinary team involving oncologists, surgeons, radiotherapists, and interventional radiologists.
ConclusionsOther Section
The clinical course of the case presented here suggests that palliative surgery may be an effective management option for a clinically problematic lesion, such as SVC obstruction, which increases during immunotherapy.
AcknowledgmentsOther Section
We are grateful to Masato Sasaki and Sawaka Tanabe for providing consultations and performing the surgery. We would like to thank Editage (www.editage.com) for providing English language editing assistance.
Funding: None.
FootnoteOther Section
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-839/rc
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-839/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-839/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Rheinheimer S, Heussel CP, Mayer P, et al. Oligoprogressive Non-Small-Cell Lung Cancer under Treatment with PD-(L)1 Inhibitors. Cancers (Basel) 2020;12:1046. [Crossref] [PubMed]
- Kagawa Y, Furuta H, Uemura T, et al. Efficacy of local therapy for oligoprogressive disease after programmed cell death 1 blockade in advanced non-small cell lung cancer. Cancer Sci 2020;111:4442-52. [Crossref] [PubMed]
- Gandara DR, von Pawel J, Mazieres J, et al. Atezolizumab Treatment Beyond Progression in Advanced NSCLC: Results From the Randomized, Phase III OAK Study. J Thorac Oncol 2018;13:1906-18. [Crossref] [PubMed]
- Ricciuti B, Genova C, Bassanelli M, et al. Safety and Efficacy of Nivolumab in Patients With Advanced Non-small-cell Lung Cancer Treated Beyond Progression. Clin Lung Cancer 2019;20:178-85.e2. [Crossref] [PubMed]
- Gettinger SN, Wurtz A, Goldberg SB, et al. Clinical Features and Management of Acquired Resistance to PD-1 Axis Inhibitors in 26 Patients With Advanced Non-Small Cell Lung Cancer. J Thorac Oncol 2018;13:831-9. [Crossref] [PubMed]
- Forde PM, Spicer J, Lu S, et al. Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer. N Engl J Med 2022;386:1973-85. [Crossref] [PubMed]
- Rowell NP, Gleeson FV. Steroids, radiotherapy, chemotherapy and stents for superior vena caval obstruction in carcinoma of the bronchus: a systematic review. Clin Oncol (R Coll Radiol) 2002;14:338-51. [Crossref] [PubMed]
- Kvale PA, Selecky PA, Prakash UB, et al. Palliative care in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:368S-403S.
- Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med 2018;378:2078-92. [Crossref] [PubMed]
- Guo L, Qu W, Wei Y, et al. Sintilimab plus chemotherapy achieved symptom relief in stage IV lung squamous cell carcinoma with superior vena cava syndrome: a case report. Ann Palliat Med 2022;11:401-6. [Crossref] [PubMed]



