Pelvic insufficiency fractures in women following radiation treatment: a case series
Introduction
An insufficiency fracture is a particular type of stress fracture that occurs when a normal load is applied to bone that has been weakened through demineralization or decreased elastic resistance (1). Radiotherapy can result in damage to osteoblasts, osteocytes, and osteoclasts, which are the three key cells that compose bone (1). Osteoblasts produce bone matrix, the components of which are essential to giving bones their strength (1). Thus, osteopenia may result after radiation, making it difficult for bones to support normal loads (1). In addition, devascularization of the bone due to radiation contributes to increased fracture risk by depriving bone cells of essential nutrients in the blood and inducing further bone loss (2).
Patients who have received radiotherapy for treatment of anal, prostate, cervical, or rectal cancers may be at increased risk of developing insufficiency fractures in the pelvic region, as treatment fields tend to include nearby weight-bearing bones. However, the threshold dose that may cause fractures is unclear (3-5). One study by Baxter et al. observed that the risk of pelvic fractures in female anal cancer patients increased three-fold (HR =3.16) after undergoing radiotherapy in the pelvic region. In female cervical cancer and rectal cancer patients, the impact of irradiation was not as apparent (cervical cancer HR =1.66, rectal cancer HR =1.65) as treatment fields for these sites do not always involve irradiation of the femoral head (3). In males treated with external beam radiotherapy for prostate cancer, the risk of hip fracture has been shown to increase by 76% (6). We present two cases in which female patients received radiation treatment to the rectum and subsequently developed pelvic insufficiency fractures.
Case presentation
Case 1
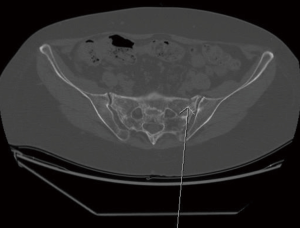
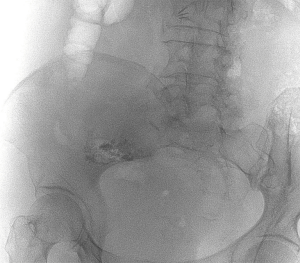
In early March of 2016, a 67-year-old female with a history of rectal adenocarcinoma was referred to a fracture clinic at the Sunnybrook Health Sciences Centre. A computed tomography (CT) scan completed in December revealed a sacral insufficiency, most likely induced by radiation, at high risk of fracture. Then, a bone scan in early January revealed that this had progressed into bilateral sacral insufficiency fractures on a background of post-radiation changes. The patient was treated with 5,040 cGy in 28 fractions to the rectum in March of 2013, followed by surgical resection and adjuvant chemotherapy. The patient had an extensive history of lower back pain centered on the sacrum that progressed after radiation treatment to the rectum. Another CT scan was ordered to assess whether a surgical approach would be required to treat the insufficiency fractures. This scan revealed bilateral sclerosis in the sacrum and transverse elements of S1 and S2, in keeping with healing of the fractures (Figure 1). When the patient was reassessed in early April, she expressed that her pain and mobility had improved. As such, the orthopedic surgeon felt that there was no role for surgery or sacroplasty and encouraged the patient to continue on bone strengthening agents.
Case 2
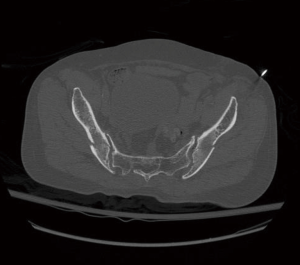
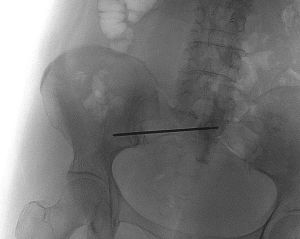
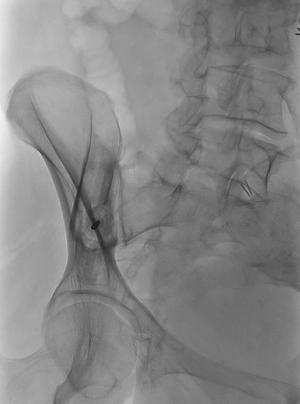
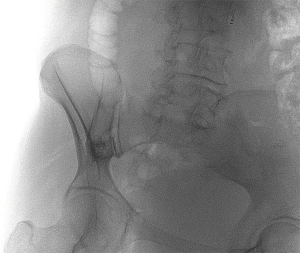
A 70-year-old female with rectal cancer was referred to a palliative oncology clinic at the Sunnybrook Odette Cancer Centre in January 2016. The patient presented with right groin pain from bilateral fractures of both iliac crests proximal to the sacroiliac (SI) joint. The patient had received radical radiation treatment of 5,040 cGy in 28 fractions to the rectum in June of 2011. As recommended by the radiologist, an MRI of the pelvis was performed to better characterize the fractures. The MRI revealed multiple insufficiency fractures in the bilateral iliac wings, left pubis, and left anterior superior iliac spine (Figure 2). After assessment by the orthopedic surgeon, the patient was referred for cementoplasty, which was completed in April 2016 (Figures 3-6). The patient experienced significant pain relief after the procedure.
Discussion
Insufficiency fractures in the pelvic region may be difficult to diagnose due to their similarities to bone metastases in clinical presentation (7). Bone scintigraphy has been shown to have high sensitivity in the diagnosis of pelvic insufficiency fractures, with H-shaped uptake of radioactive agents being a good indicator of this although its incidence is only around 42% (8,9). CT scans are useful for depicting fracture lines, but may not be as sensitive in distinguishing pathological from insufficiency fractures when compared to other modes of imaging (9,10). On MRI, bone marrow changes indicated by T1 hypointense and T2 hyperintense areas near the SI joints after pelvic radiation may be caused by metastases or insufficiency fractures (7,10). Bilateral lesions most likely coincide with radiation-induced insufficiency fractures as it is uncommon that bone metastases develop symmetrically. However, for unilateral lesions, other clinical factors should be considered to differentiate between the two (7). For example, the absence of other metastatic disease and presence of other fractures have been used by other studies to exclude bone metastases (8). In one of the cases presented above, it was not immediately apparent whether a pelvic fracture was pathologic or due to insufficiency, therefore it had to be characterized further with an MRI scan.
There are several predispositions for pelvic insufficiency fractures, the most notable being osteoporosis induced by post-menopausal changes in women (4,11). A study conducted by Blomlie et al. observed that of 121 patients with sacral insufficiency fractures reported in the literature, 115 were postmenopausal women (11). In women, age also plays an important role in predicting the susceptibility of patients to insufficiency fractures, as shown in studies by Tokumaru et al. (5) and Oh et al. (4). Additionally, these studies reported that low body weight was significantly correlated to increased risk of insufficiency fractures (4,5). Other predisposing factors for osteoporosis include rheumatoid arthritis, corticosteroid-therapy, smoking history, and hyperthyroidism (12). Pelvic insufficiency fractures following radiotherapy are not rare occurrences. The study by Tokumaru et al. reported a 2-year incidence rate of 36.9% and Oh et al. saw a 5-year incidence rate of 19.7% in cervical cancer patients (4,5). Therefore, it is imperative that patients are aware of these predispositions before radiotherapy and are provided with methods of minimizing risk of fracture.
In addition to these predisposing factors, the dose, fractionation, and radiation treatment field can influence the amount of toxicity experienced by patients. Spreading the total dose of radiation over greater numbers of fractions can reduce toxicity as this allows for smaller doses per fraction (4). One study reported that a total dose above 4,000 cGy may be related to an increased incidence of insufficiency fractures (13). To reduce risk of fracture, the pelvis may be shielded from radiation treatment without compromising the target volume by using a multiple beam CT planning approach (14). Furthermore, several studies have shown that intensity-modulated radiotherapy (IMRT) can be used to decrease radiation toxicity and potentially reduce risk of insufficiency fractures (15).
Pelvic fractures have significant implications on patient QOL by inducing pain and limiting ambulatory capacity, thus making it extremely difficult to live independently. In a study by Miller, less than 50% of patients with pelvic fractures were able to return to their ambulatory status before the fracture (16). Increased morbidity and mortality has also been associated with pelvic fractures particularly in elderly patients (17). One study suggested that the risk of death increases 2.4 times due to pelvic fractures and that this higher mortality rate extends over a period of at least 3 years (17).
It is important that health care professionals and patients are aware of the increased risk of pelvic insufficiency fractures due to radiotherapy so that the corresponding symptoms can be closely monitored and appropriate imaging routinely performed. Preventative measures should also be taken including regular monitoring of osteoporosis or osteopenia in patients using bone mineral density (BMD) tests (1). Bone density may also be increased through preventative therapies such as bisphosphonates or calcitonin (4). In addition, supportive services and patient education in fall prevention may be beneficial (4).
Cementoplasty is an effective method of palliation in cancer patients with pelvic insufficiency fractures. A cementoplasty involves injecting bone cement into a fracture using a thin needle in order to stabilize and strengthen the bone, whether the fracture was pathologic or due to insufficiency (18). However, cementoplasty runs the small risk of cement leaking from the fracture line. In order to reduce the risk of leakage, cement should ideally be injected at a slow rate with real-time, good quality imaging (19). If the cement does happen to leak, patients are typically asymptomatic and the leakage often does not hinder pain relief or quality of life (20). A majority of patients receive conservative, non-surgical treatment in which weight-bearing is avoided and medications for bone density are prescribed in hope that the fracture will spontaneously heal (4).
Pelvic insufficiency fractures induced by radiation treatment may be mistaken for pathologic fractures in cancer patients. Thorough investigations should be conducted to properly identify insufficiency fractures such that appropriate treatment can be prescribed. In addition, measures should be taken to reduce the risk of insufficiency fractures in patients receiving radiation treatment near the pelvis. In particular for post-menopausal women, this includes investigations using BMD scans and prescribing bone strengthening medications.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from both patients for publication of this case report and any accompanying images.
References
- Matcuk GR Jr, Mahanty SR, Skalski MR, et al. Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol 2016;23:365-75. [Crossref] [PubMed]
- Oh D, Huh SJ. Insufficiency fracture after radiation therapy. Radiat Oncol J 2014;32:213-20. [Crossref] [PubMed]
- Baxter NN, Habermann EB, Tepper JE, et al. Risk of pelvic fractures in older women following pelvic irradiation. JAMA 2005;294:2587-93. [Crossref] [PubMed]
- Oh D, Huh SJ, Nam H, et al. Pelvic insufficiency fracture after pelvic radiotherapy for cervical cancer: analysis of risk factors. Int J Radiat Oncol Biol Phys 2008;70:1183-8. [Crossref] [PubMed]
- Tokumaru S, Toita T, Oguchi M, et al. Insufficiency fractures after pelvic radiation therapy for uterine cervical cancer: an analysis of subjects in a prospective multi-institutional trial, and cooperative study of the Japan Radiation Oncology Group (JAROG) and Japanese Radiation Oncology Study Group (JROSG). Int J Radiat Oncol Biol Phys 2012;84:e195-200. [Crossref] [PubMed]
- Elliott SP, Jarosek SL, Alanee SR, et al. Three-dimensional external beam radiotherapy for prostate cancer increases the risk of hip fracture. Cancer 2011;117:4557-65. [Crossref] [PubMed]
- Kanberoglu K, Mihmanli I, Kurugoglu S, et al. Bone marrow changes adjacent to the sacroiliac joints after pelvic radiotherapy mimicking metastases on MRI. Eur Radiol 2001;11:1748-52. [Crossref] [PubMed]
- Fujii M, Abe K, Hayashi K, et al. Honda sign and variants in patients suspected of having a sacral insufficiency fracture. Clin Nucl Med 2005;30:165-9. [Crossref] [PubMed]
- Gotis-Graham I, McGuigan L, Diamond T, et al. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br 1994;76:882-6. [PubMed]
- Cabarrus MC, Ambekar A, Lu Y, et al. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am J Roentgenol 2008;191:995-1001. [Crossref] [PubMed]
- Blomlie V, Rofstad EK, Talle K, et al. Incidence of radiation-induced insufficiency fractures of the female pelvis: evaluation with MR imaging. AJR Am J Roentgenol 1996;167:1205-10. [Crossref] [PubMed]
- Eastell R. Treatment of postmenopausal osteoporosis. N Engl J Med 1998;338:736-46. [Crossref] [PubMed]
- Fu AL, Greven KM, Maruyama Y. Radiation osteitis and insufficiency fractures after pelvic irradiation for gynecologic malignancies. Am J Clin Oncol 1994;17:248-54. [Crossref] [PubMed]
- Ogino I, Okamoto N, Ono Y, et al. Pelvic insufficiency fractures in postmenopausal woman with advanced cervical cancer treated by radiotherapy. Radiother Oncol 2003;68:61-7. [Crossref] [PubMed]
- Zelefsky MJ, Fuks Z, Happersett L, et al. Clinical experience with intensity modulated radiation therapy (IMRT) in prostate cancer. Radiother Oncol 2000;55:241-9. [Crossref] [PubMed]
- Miller CW. Survival and ambulation following hip fracture. J Bone Joint Surg Am 1978;60:930-4. [PubMed]
- Prieto-Alhambra D, Avilés FF, Judge A, et al. Burden of pelvis fracture: a population-based study of incidence, hospitalisation and mortality. Osteoporos Int 2012;23:2797-803. [Crossref] [PubMed]
- Moussazadeh N, Laufer I, Werner T, et al. Sacroplasty for cancer-associated insufficiency fractures. Neurosurgery 2015;76:446-50; discussion 450. [Crossref] [PubMed]
- Deschamps F, de Baere T. Cementoplasty of bone metastases. Diagn Interv Imaging 2012;93:685-9. [Crossref] [PubMed]
- Sun G, Jin P, Liu XW, et al. Cementoplasty for managing painful bone metastases outside the spine. Eur Radiol 2014;24:731-7. [Crossref] [PubMed]