
Characteristics and prognostic outcome factors between young and elderly peritoneal dialysis patients: a prospective cohort study
Introduction
Chronic kidney disease (CKD) is a global public health problem and becoming increasingly common. A survey in China found that patients with stage 3 CKD numbered almost 1.2 million in 2012, and the average age was 63.6 years (1). From its development to the end stage, peritoneal dialysis (PD) is one of the main renal replacement therapies and a better choice for elderly patients with endstage renal disease (ESRD), because of its lesser effect on hemodynamics, protection of residual renal function, low cost and simple operation (2).
In recent years, researchers from various countries have explored the risk factors of adverse outcomes of elderly PD patients. They found that elderly PD patients tended to have multiple comorbidities, including diabetes, hypertension, cardiovascular and cerebrovascular diseases (3), and this combined with age and nutritional deficiency could influence their clinical outcomes (4,5). Meanwhile peritonitis is the main risk factor for withdrawal from PD, and death is the main reason for ceasing PD (6,7). However, previous studies have been mainly retrospective, and the factors influencing mortality differ across countries. There also have been few reports in China about the reasons for withdrawal from PD, especially regarding transfer to hemodialysis (HD). How to screen out risk factors with high efficiency from many clinical indicators, especially indicators that are simple to use and conducive to prevent adverse outcome in elderly PD patients, is of great clinical significance.
In this study, we analyzed the characteristics, prognosis (death, transfer to HD) of elderly PD patients by comparison with a younger group, to assess the prognostic factors in elderly CKD patients. We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1008/rc).
Methods
Study groups
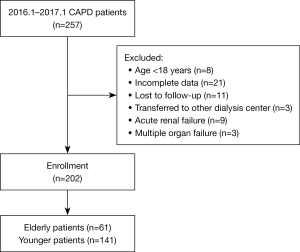
The prospective cohort study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the Ethics Committee of the Cangzhou Central Hospital in Cangzhou City, Hebei Province, China [approval number: 2020-257-01(Z)]. Written informed consent was given by each of the 202 patients undergoing continuous ambulatory PD between January 2016 and January 2017 in the Department of Nephrology of Cangzhou Central Hospital. Conventional PD solutions (Dianeal 1.5%, 2.5%, or 4.25% dextrose; Baxter Healthcare, Guangzhou, China), Y-sets, and twin-bag systems were used and patients did the exchange themselves after successful training by primary care nurses. According to age, the PD patients were divided into an elderly group (age ≥65 at PD initiation) and a younger group (age <65). The inclusion criteria were: age >18 years, first PD treatment and dialysis time >3 months, and complete data. The exclusion criteria included incomplete data, loss to follow-up or uncooperative with follow-up, or transfer to another dialysis center. Additionally, we did not include patients diagnosed as acute renal failure or multiple organ failure. Figure 1 is a flow chart of the enrolment. End of follow-up was defined as the day of the outcome (death or transfer to HD) or end of follow-up (January 2020). In this study, the mortality rate after follow-up was used as the main indicator to estimate the sample size. For two-sided test, the test level was 0.5, the degree of control was 80%, and the two groups were 1:1. According to a previous study (8), the mortality is about 56% in elderly PD patients, about 30% in young PD patients. PASS2008 was used to estimate that 53 pairs of effective patients were needed.
Demographic and clinical data
The demographic data included sex, age, body mass index (BMI), etiological diagnosis (diabetic nephropathy, hypertensive renal damage, primary glomerular disease), peritonitis or not, and bacterial culture results (gram-positive or gram-negative bacilli). We also recorded the outcomes of patients: continue PD, death, time and reason for transferring to HD, kidney transplantation, time and cause of death. The Charlson Comorbidity Index (CCI) was used to measure comorbidity (9). The following hemodynamic variables were recorded: white blood cells (WBC), red blood cells (RBC), and hemoglobin (Hb), platelets (PLT), albumin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin, direct bilirubin, serum creatinine, blood urea nitrogen, serum calcium, potassium, sodium, and ferritin, total Urea clearance index (Kt/V), residual Kt/V, weekly creatinine clearance rate (WCcr), residual creatinine clearance rate, normalized protein catabolic rate (nPCR), dialysis duration, use of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers (ACEI/ARB), and history of cerebrovascular disease, ischemic heart disease (ISD) and heart failure (HF).
Outcomes
Data are collected through the PD telemedicine App, a web-based data collection system and medical records. Patients were followed up until death, permanent transfer to hemodialysis (defined as more than 3 months), renal transplantation, loss to follow-up, or the end of study.
Statistical analysis
Data analyses were performed using SPSS23.0 and R 3.6.1 version. Results are expressed as mean ± standard deviation (SD), median and interquartile range or number and percentages (%), as appropriate. The Kolmogorov-Smirnov test was used to examine the normality of all numeric continuous variables. Independent sample t-tests were used if with a normal distribution, and nonparametric tests (Mann-Whitney U test) were used to examine variables without a normal distribution, when comparing between groups. Categorical data were compared between the elderly and younger groups by chi-square test. When there were <5 observations in a group-outcome combination, Fisher’s test was used. Kaplan-Meier survival curve analysis was performed to investigate the differences in survival and transferring to HD between the elderly and younger groups. Multivariate Cox regression analysis was used to screen the risk factors of mortality in elderly patients. Using the backward method, the entry probability was set to 0.05, and the removal probability was set to 0.10. All tests were two-sided, and P<0.05 was considered statistically significant.
Results
General characteristics of the elderly patients
We enrolled 202 PD patients (61 in the elderly group, 141 in the younger group) with a median follow-up of 44 months. Compared with the younger group, elderly patients were more likely to have lower albumin and nPCR, and more comorbidities, especially cardiovascular and cerebrovascular diseases. Diabetic nephropathy was common in elderly group, with a statistically significant difference (P<0.01). Table 1 shows the baseline characteristics of patients grouped by age.
Table 1
| Characteristics | All patients, n=202 | Elderly group, n=61 | Younger group, n=141 | P value |
|---|---|---|---|---|
| Demographic data | ||||
| Age, years | 57.00 (45.00, 65.00) | 72.00 (66.50, 76.00) | 50.00 (37.00, 57.50) | <0.001 |
| Male, n (%) | 121 (59.9) | 34 (55.7) | 87 (61.7) | 0.427 |
| Laboratory data | ||||
| BMI, kg/m2, mean ± SD | 23.97±4.33 | 23.92±3.54 | 24.00±4.64 | 0.903 |
| WBC, ×109/L | 6.64 (5.30, 8.11) | 7.13 (5.33, 9.32) | 6.40 (5.26, 7.77) | 0.158 |
| RBC, ×1012/L, mean ± SD | 3.46±0.59 | 3.36±0.69 | 3.50±0.54 | 0.159 |
| Hb, g/L | 102.00 (91.00, 116.00) | 100.00 (85.00, 115.50) | 103.00 (93.00, 116.00) | 0.279 |
| PLT, ×109/L | 209.50 (163.00, 251.25) | 202.00 (146.50, 252.00) | 212.00 (165.00, 251.00) | 0.281 |
| ALB, g/L | 33.70 (37.20, 40.10) | 35.60 (32.00, 38.00) | 38.40 (34.95, 41.00) | <0.001 |
| ALT, u/L | 12.60 (9.15, 17.15) | 13.00 (9.80, 16.90) | 12.45 (9.10, 17.38) | 0.153 |
| AST, u/L | 15.80 (12.00, 20.30) | 16.00 (12.10, 20.45) | 15.45 (12.00, 20.15) | 0.171 |
| TBIL, μmol/L | 4.10 (4.95, 6.60) | 3.90 (4.50, 6.10) | 4.38 (5.10, 6.60) | 0.151 |
| DBIL, μmol/L | 1.70 (1.20, 2.30) | 1.70 (1.20, 2.30) | 1.70 (1.20, 2.30) | 0.759 |
| Scr, μmol/L | 815.50 (587.50, 1,039.75) | 747.00 (541.00, 979.00) | 607.00 (828.00, 1,042.00) | 0.253 |
| BUN, mmol/L | 19.50 (14.78, 22.93) | 18.20 (13.90, 22.20) | 19.90 (15.50, 23.50) | 0.133 |
| Serum Ca, mmol/L | 2.16 (2.01, 2.31) | 2.12 (1.96, 2.29) | 2.17 (2.02, 2.33) | 0.135 |
| Serum K, mmol/L | 4.20 (3.70, 4.80) | 4.20 (3.60, 4.75) | 4.20 (3.80, 4.80) | 0.414 |
| Serum Na, mmol/L | 141.00 (138.00, 142.15) | 141.00 (137.00, 143.00) | 141.00 (139.00, 142.00) | 0.309 |
| Ferritin, ug/L | 269.70 (137.70, 573.50) | 300.00 (138.00, 514.45) | 257.00 (136.25, 584.80) | 0.725 |
| Total Kt/V | 1.72 (1.45, 2.04) | 1.69 (1.50, 2.04) | 1.73 (1.42, 2.04) | 0.784 |
| Residual Kt/V | 0.08 (0.00, 0.33) | 0.10 (0.01, 0.32) | 0.06 (0.00, 0.34) | 0.343 |
| Total WCcr, mL/min | 45.67 (39.89, 53.94) | 46.09 (40.77, 55.15) | 45.17 (39.58, 53.68) | 0.769 |
| Residual Ccr, mL/min | 2.00 (0.00, 9.79) | 2.82 (0.07, 15.07) | 1.19 (0.00, 10.29) | 0.235 |
| nPCR, g/kg/day | 0.82 (0.71, 0.92) | 0.74 (0.62, 0.85) | 0.85 (0.76, 0.93) | 0.003 |
| Dialysis time (months) | 26.00 (13.00, 49.00) | 21.00 (9.50, 46.00) | 27.00 (14.00, 51.00) | 0.279 |
| CCI score | 9.00 (5.00, 13.00) | 11.00 (6.50, 15.00) | 9.00 (5.00, 11.00) | 0.003 |
| Medical history, n (%) | ||||
| ISD | 58 (28.7) | 34 (55.7) | 24 (17.0) | <0.001 |
| HF | 73 (36.1) | 27 (44.3) | 46 (32.6) | 0.114 |
| Cerebrovascular disease | 40 (19.8) | 19 (31.1) | 21 (14.9) | 0.008 |
| PD-related Peritonitis | 88 (43.6) | 21 (34.4) | 67 (47.5) | 0.085 |
| Gram-positive | 32 (15.8) | 10 (16.4) | 22 (15.6) | 0.888 |
| Gram-negative | 20 (9.9) | 8 (13.1) | 12 (8.5) | 0.314 |
| ACEI/ARB use | 74 (36.6) | 18 (29.5) | 56 (39.7) | 0.167 |
| Primary disease, n (%) | ||||
| DN | 46 (22.8) | 22 (36.1) | 24 (20.6) | 0.003 |
| HRD | 27 (13.4) | 11 (18.0) | 16 (10.9) | 0.200 |
| CG | 30 (14.9) | 6 (9.8) | 24 (14.8) | 0.187 |
Data are presented as median (interquartile range), mean ± SD or frequency and percentage. PD, peritoneal dialysis; BMI, body mass index; SD, standard deviation; WBC, white blood cell; RBC, red blood cell; Hb, hemoglobin; PLT, platelet; ALB, albumin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; TBIL, total bilirubin; DBIL, direct bilirubin; Scr, serum creatinine; BUN, blood urea nitrogen; Kt/V, total Urea clearance index; WCcr, weekly creatinine clearance rate; nPCR, normalized protein catabolic rate; CCI, Charlson Comorbidity Index; ISD, ischemic heart disease; HF, heart failure; ACEI/ARB, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers; DN, diabetic nephropathy; HRD, hypertensive renal damage; CG, chronic glomerulonephritis.
Outcomes of elderly patients
To the end of the study, 121 (59.9%) patients continued to receive PD, 48 (23.8%) died, 25 (12.4%) were transferred to HD, and 8 (3.9%) underwent kidney transplantation. In the elderly group, 27 (44.3%) patients died, 2 (3.3%) were transferred to HD, and 1 (1.6%) received a kidney transplant. Due to small number of kidney transplantation patients in the elderly group, the reasons for kidney transplantation were not elaborated. Table 2 shows the outcomes of all PD patients.
Table 2
| Outcomes | All patients, n=202 | Elderly group, n=61 | Younger group, n=141 |
|---|---|---|---|
| Stay on PD, n (%) | 121 (59.9) | 31 (50.8) | 90 (63.8) |
| Death, n (%) | 48 (23.8) | 27 (44.3) | 21 (14.9) |
| Transferred to HD, n (%) | 25 (12.4) | 2 (3.3) | 23 (16.3) |
| Kidney transplant, n (%) | 8 (3.9) | 1 (1.6) | 7 (5.0) |
PD, peritoneal dialysis; HD, hemodialysis.
Mortality of PD patients
A total of 27 (44.3%) elderly patients and 21 (14.3%) younger patients died (Figure 2). The survival time of the elderly group was significantly lower than that of the younger group. The 1-, 2-, 3- and 4-year survival rates were 81.97%, 70.49%, 60.66% and 55.74%, respectively. The main cause of death in the elderly group was cardiovascular disease, while in younger group it was infection (Table 3).
Table 3
| Death | Elderly group, cases (%) | Younger group, cases (%) |
|---|---|---|
| Cardiovascular disease | 10 (37.0) | 4 (19.0) |
| Cerebrovascular disease | 4 (14.8) | 4 (19.0) |
| Infection | 3 (11.1) | 6 (28.6) |
| Cachexia | 3 (11.1) | 2 (9.5) |
| Other | 7 (25.9) | 5 (23.8) |
Transferring to HD
A total of 2 (3.3%) elderly PD patients, and 23 (16.3%) younger patients transferred to HD. Peritonitis was the chief reason for both elderly and younger PD patients to transfer to HD (Table 4).
Table 4
| Transfer to HD | Elderly group, cases (%) | Younger group, cases (%) |
|---|---|---|
| Peritonitis | 2 (3.3) | 18 (12.8) |
| Inadequate dialysis | 0 | 2 (1.4) |
| Dialysis failure | 0 | 2 (1.4) |
| Others | 0 | 1 (0.7) |
HD, hemodialysis.
Prognostic outcome factors in elderly PD patients
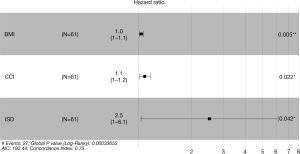
For elderly PD patients, univariate Cox regression analysis indicated that BMI, CCI, previous ISD, peritonitis, and dialysis time were risk factors for long-term survival. BMI, CCI and ISD remained independent significant predictors of long-term survival of elderly PD patients by multivariate Cox regression analysis (Table 5, Figure 3). CCI (r=0.471, P<0.001) and dialysis time (r=0.260, P=0.043) were related to peritonitis and may be confounding factors.
Table 5
| Factor | Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|---|
| P | HR | 95% CI | P | HR | 95% CI | ||
| BMI | 0.016 | 1.139 | 1.025–1.265 | 0.005 | 1.0 | 1.0–1.1 | |
| CCI | 0.018 | 1.073 | 1.012–1.137 | 0.022 | 1.1 | 1.0–1.2 | |
| ISD | 0.011 | 3.084 | 1.301–7.315 | 0.042 | 2.5 | 1.0–6.1 | |
| Peritonitis | 0.042 | 2.305 | 1.031–5.154 | 0.284 | N/A | N/A | |
| Dialysis time | 0.089 | 1.014 | 0.998–1.030 | 0.310 | N/A | N/A | |
BMI, body mass index; CCI, Charlson Comorbidity Index; ISD, ischemic heart disease; HR, hazard ratio; CI, confidence interval; N/A, not available.
Discussion
Both the aging of the population and the outbreak of COVID-19 have led to increased rates of ESRD and the number of elderly patients needing PD (10). In order to improve the prognosis and quality of life in elderly patients with PD, we need to understand the factors influencing their survival and actively prevent and control these risk factors.
In the present study, we analyzed the general condition of elderly CKD patients, the reasons for withdrawal from PD therapy, and the risk factors for survival to provide guidance for improving prognosis and prolonging the survival time of patients with ESRD on PD.
Compared with the younger group, the elderly group of PD patients tended to have hypoalbuminemia and low nPCR, both of which are important indicators of the nutrition of patients (11), and our finding was consistent with the study by Khoshhali et al. (12). Wang et al. also reported that serum albumin remained lower in elderly patients (13). During PD, nutrients are lost in the dialysis solution, and the absorptive capacity of gastrointestinal tract is decreased in elderly patients, leading to malnutrition. Arteriosclerosis and cardiovascular and cerebrovascular events often occur with diabetic nephropathy (14,15), and age is also a risk factor of vascular calcification (16). Because PD does not require vascular access and has less effect on hemodynamics, elderly patients prefer PD. Although it has been reported that elderly PD patients are inclined to develop peritonitis (17), there was no difference in the incidence of peritonitis between the elderly and younger groups in this study, which was consistent with a Canadian study that reported elderly PD patients aged ≥70 years old had no relationship with peritonitis (18), considering they had better family and social support and were treated with advanced antibiotics.
In our study, the mortality rate of younger patients on PD was significantly lower than that of the elderly patients. Age is a risk factor for the survival of PD patients (4,19). The 1-, 2-, 3- and 4-year survival rates of elderly PD patients were 81.97%, 70.49%, 60.66% and 55.74%, respectively. Another study in China found that the 1-, 3-, and 5-year mortality rates of elderly patients with PD were respectively 79%, 56% and 30% (19), which is generally consistent with our results. Cardiovascular disease is the leading cause of death; 53.4% of elderly PD patients had cardiovascular complications in a retrospective study (8). The US Renal Data System data showed that cardiovascular events were the main cause of death in dialysis patients (20), which was related to metabolic abnormalities and the increased incidence of diabetic nephropathy in elderly PD patients.
Our study results provide evidence that high BMI, high CCI and ISD are independent risk factors for death in elderly PD patients. Patients with high BMI have a high risk of dialysis (21), and obesity can increase the incidence of cardiovascular and cerebrovascular events, thus increasing the risk of death (22). However, the relationship between BMI and survival in elderly patients with PD is controversial. Some studies found that obese PD patients lived longer or for the same time as those with lower BMI (23,24), considering that patients with lower BMI will have increased protein consumption and thus inflammation, and high BMI can increase hemodynamic stability and the isolation of fat tissue from toxins (25). Another study found that baseline BMI was not related to the prognosis of PD (26), so more studies are needed to explore the relationship between BMI and death in elderly PD patients. As mentioned, CCI is an important index of complications. Genestier et al. showed that CCI positively correlated with death in elderly patients (27). A retrospective analysis of 292 patients found the 2-year survival rate of elderly patients with CCI score >9 was 38%, and that of patients with CCI <7 reached 69% (28). Elderly PD patients often have ISD, and thus the risk of recurrence of cardiovascular and cerebrovascular events increases (29), so elderly PD patients are at high risk of death.
In this study, peritonitis was main reason for transferring to HD in both elderly and younger patients. Li et al. (30) and Banno et al. (31) also found that the main reason for transferring to HD was peritonitis. The number of elderly patients transferring to HD was less than that of younger patients. Although elderly patients had a higher risk of peritonitis-related and all-cause death. In a recent study from Brazil, the only factor associated with death during peritoneal infection was older age (32), so the elderly patients had no chance to transfer to HD.
This study elucidated the characteristics of elderly PD patients, their prognosis and the prognostic factors for death, which will help nephrologists improve the prognosis of these patients. However, this study had some limitations. First, it was a single-center, relatively small sample study, which cannot represent the situation of all elderly PD patients in China. Therefore, additional multicenter studies are needed in larger populations to confirm the conclusions of our study. In addition, we did not analyze the economic and social status of each patient.
Conclusions
Compared with a younger group, elderly PD patients had poor nutritional status, more complications, a high proportion of diabetic nephropathy and high mortality. High BMI, high CCI and previous ISD were independent risk factors of death of elderly PD patients. Cardiovascular disease was the main cause of death in elderly group. Peritonitis was major reason for PD patients transferring to HD.
Acknowledgments
We would like to thank the nursing staff of the PD unit for inspiration and helpful discussions.
Funding: The study was supported by Key Research and Development Program of Cangzhou City of Hebei Province (No. 204106081) and Research Fund Project of Hebei Provincial Health Commission (No. 20220332).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1008/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-1008/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-1008/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Ethics Committee of the Cangzhou Central Hospital in Cangzhou City, Hebei Province, China [approval number: 2020-257-01(Z)]. Written informed consent was given by each of patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhang L, Wang F, Wang L, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 2012;379:815-22. [Crossref] [PubMed]
- Brown EA, Johansson L. Epidemiology and management of end-stage renal disease in the elderly. Nat Rev Nephrol 2011;7:591-8. [Crossref] [PubMed]
- Dimkovic NB, Prakash S, Roscoe J, et al. Chronic peritoneal dialysis in octogenarians. Nephrol Dial Transplant 2001;16:2034-40. [Crossref] [PubMed]
- Hung CC, Chang CT, Lee CC, et al. Prognostic predictors of technique and patient survival in elderly Southeast Asian patients undergoing continuous ambulatory peritoneal dialysis. Int J Clin Pract 2009;63:254-60. [Crossref] [PubMed]
- Weinhandl ED, Foley RN, Gilbertson DT, et al. Propensity-matched mortality comparison of incident hemodialysis and peritoneal dialysis patients. J Am Soc Nephrol 2010;21:499-506. [Crossref] [PubMed]
- Mizuno M, Ito Y, Tanaka A, et al. Peritonitis is still an important factor for withdrawal from peritoneal dialysis therapy in the Tokai area of Japan. Clin Exp Nephrol 2011;15:727-37. [Crossref] [PubMed]
- Luo Q, Xia X, Lin Z, et al. Very early withdrawal from treatment in patients starting peritoneal dialysis. Ren Fail 2018;40:8-14. [Crossref] [PubMed]
- Iqbal MM, Islam MN, Mansur MA, et al. Outcome of peritoneal dialysis and hemodialysis in elderly patients with diabetes: early experience from Bangladesh. Adv Perit Dial 2005;21:85-9. [PubMed]
- Beddhu S, Zeidel ML, Saul M, et al. The effects of comorbid conditions on the outcomes of patients undergoing peritoneal dialysis. Am J Med 2002;112:696-701. [Crossref] [PubMed]
- Ahmed N, Khderat AH, Sarsour A, et al. The vulnerability of maintenance dialysis patients with COVID-19: mortality and risk factors from a developing country. Ann Med 2022;54:1511-9. [Crossref] [PubMed]
- Grzegorzewska A, Dobrowolska-Zachwieja A. Comparison of indices of kinetic modelling of urea and creatinine as well as evaluation of nutritional status of patients treated with continuous ambulatory peritoneal dialysis. Pol Arch Med Wewn 1994;91:417-26. [PubMed]
- Khoshhali M, Kazemi I, Hosseini SM, et al. Relationship between trajectories of serum albumin levels and technique failure according to diabetic status in peritoneal dialysis patients: A joint modeling approach. Kidney Res Clin Pract 2017;36:182-91. [Crossref] [PubMed]
- Wang X, Han Q, Wang T, et al. Serum albumin changes and mortality risk of peritoneal dialysis patients. Int Urol Nephrol 2020;52:565-71. [Crossref] [PubMed]
- Yao Q, Lindholm B, Heimbürger O. Peritoneal dialysis prescription for diabetic patients. Perit Dial Int 2005;25:S76-9. [Crossref] [PubMed]
- Hadjadj S, Cariou B, Fumeron F, et al. Death, end-stage renal disease and renal function decline in patients with diabetic nephropathy in French cohorts of type 1 and type 2 diabetes. Diabetologia 2016;59:208-16. [Crossref] [PubMed]
- Ma D, Yan H, Yang X, et al. Abdominal aortic calcification score as a predictor of clinical outcome in peritoneal dialysis patients: a prospective cohort study. BMC Nephrol 2020;21:151. [Crossref] [PubMed]
- Wu H, Ye H, Huang R, et al. Incidence and risk factors of peritoneal dialysis-related peritonitis in elderly patients: A retrospective clinical study. Perit Dial Int 2020;40:26-33. [Crossref] [PubMed]
- Nessim SJ, Bargman JM, Austin PC, et al. Impact of age on peritonitis risk in peritoneal dialysis patients: an era effect. Clin J Am Soc Nephrol 2009;4:135-41. [PubMed]
- Joshi U, Guo Q, Yi C, et al. Clinical outcomes in elderly patients on chronic peritoneal dialysis: a retrospective study from a single center in china. Perit Dial Int 2014;34:299-307. [Crossref] [PubMed]
- US Renal Data System 2016 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis 2017;69:A4. [Crossref] [PubMed]
- Kalantar-Zadeh K, Kopple JD. Body mass index and risk for end-stage renal disease. Ann Intern Med 2006;144:701-author reply 701-2. [Crossref] [PubMed]
- Goodkin DA, Mapes DL, Held PJ. The dialysis outcomes and practice patterns study (DOPPS): how can we improve the care of hemodialysis patients? Semin Dial 2001;14:157-9. [Crossref] [PubMed]
- Chung SH, Lindholm B, Lee HB. Influence of initial nutritional status on continuous ambulatory peritoneal dialysis patient survival. Perit Dial Int 2000;20:19-26. [Crossref] [PubMed]
- Quero M, Comas J, Arcos E, et al. Impact of obesity on the evolution of outcomes in peritoneal dialysis patients. Clin Kidney J 2020;14:969-82. [Crossref] [PubMed]
- Park J, Ahmadi SF, Streja E, et al. Obesity paradox in end-stage kidney disease patients. Prog Cardiovasc Dis 2014;56:415-25. [Crossref] [PubMed]
- Badve SV, Paul SK, Klein K, et al. The association between body mass index and mortality in incident dialysis patients. PLoS One 2014;9:e114897. [Crossref] [PubMed]
- Genestier S, Meyer N, Chantrel F, et al. Prognostic survival factors in elderly renal failure patients treated with peritoneal dialysis: a nine-year retrospective study. Perit Dial Int 2010;30:218-26. [Crossref] [PubMed]
- Vrtovsnik F, Porcher R, Michel C, et al. Survival of elderly patients on peritoneal dialysis: retrospective study of 292 patients, from 1982 to 1999. Perit Dial Int 2002;22:73-81. [Crossref] [PubMed]
- Li J, Li Y, Zou Y, et al. Use of the systemic inflammation response index (SIRI) as a novel prognostic marker for patients on peritoneal dialysis. Ren Fail 2022;44:1227-35. [Crossref] [PubMed]
- Li M, Yan J, Zhang H, et al. Analysis of outcome and factors correlated with maintenance peritoneal dialysis. J Int Med Res 2019;47:4683-90. [Crossref] [PubMed]
- Banno T, Shima H, Kawahara K, et al. Risk factors for peritoneal dialysis withdrawal due to peritoneal dialysis-related peritonitis. Nephrol Ther 2021;17:108-13. [Crossref] [PubMed]
- de Moraes TP, Olandoski M, Caramori JC, et al. Novel predictors of peritonitis-related outcomes in the BRAZPD cohort. Perit Dial Int 2014;34:179-87. [Crossref] [PubMed]
(English Language Editor: K. Brown)



