Illness understanding in patients with advanced lung cancer: curse or blessing?
Introduction
Lung Cancer is the most common cause of cancer death in Europe with around 354,000 deaths in 2012 (20% of the total) (1,2). Its diagnosis in advanced stage is the most obvious cause of this poor prognosis. Patients with advanced lung cancer have a median survival of 10 months (3). In view of the fact that there is no cure possible, treatment is primarily based on maintaining the quality of life (QoL). According to the World Health Organization (WHO) this means a treatment which improves the QoL of patients and their relatives, who deal with a life threatening disease, by preventing and relieving the suffering by means of early detection, careful judgment and treatment of pain and other problems of physical, psychosocial and spiritual kind (4). Informing the patient and his/her family of the consequences and prognosis of their disease is an important part of the treatment and needs to be undertaken by the treating oncologist. In daily practice, most patients start with palliative chemotherapy (and, if needed, palliative radiotherapy) to improve survival while maintaining their QoL by improving symptom control (5). The other aspects of palliative care are often addressed in a later phase of the disease history (6). Can a patient be informed of his prognosis from the diagnosis onwards without detrimental effect on QoL? The purpose of this current review is to provide an answer on this relevant question.
The consequences of a primarily physically-oriented treatment
When a physician brings bad news and tells the patient that he/she has an incurable disease, this part of the consultation is often quickly followed by the discussion of the treatment plan, where the main discussion is about side-effects of chemo- and/or radiotherapy. Physicians and patients are focused on the ‘treatment calendar’ and therefore primarily on the physical aspect of lung cancer. They don’t address the factual goal of the treatment, which is palliation in view of a better QoL. There also seems to be a non-verbal message: all these efforts and costs cannot be ‘useless’, and the patient makes a mind switch where he believes that the treatment will cure him/her (7).
Although the patient should be aware of the palliative goal of the treatment, recent research has shown that most patients assume that they are still receiving a curative treatment (8-10). It hence seems that many patients and their family have no insight about the palliative setting of their disease. In 68% of the cases, the patient’s family only realizes that the disease is incurable, when this has explicitly been said by the physician (11). The same authors also report that this issue is only discussed rather late in the disease history: in 24% of the cases even less than a month prior to the patient’s death. This implies that these conversations are often held by a physician, other than the treating physician, during an acute hospital admission when the patient is already in the final stage of his disease evolution (12). Pardon et al. have shown that more than half of the patients with metastasized lung cancer were not involved in a conversation about life end, despite the fact that most patients indicated that they wanted to be involved (13). Starting with palliative care at an early stage of the disease makes this possible. This is called early palliative care (EPC) in which the treating physician plays a role in communicating about the goal of the therapy.
What is the content of EPC?
EPC includes better symptom control, strengthening coping mechanisms, improving illness understanding, making the patient aware of the prognosis and involving the family (14). This results in a more holistic approach towards the patient in comparison with the standard oncologic outpatient contact.
EPC and advanced lung cancer
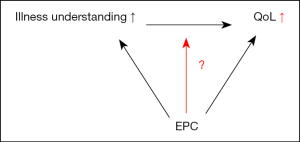
Temel et al. (15) performed a randomized controlled trial in patients with advanced lung cancer, whereby the effect of EPC, starting within 8 weeks after diagnosis in combination with the standard oncological treatment was compared to standard oncological treatment only. They showed that the intervention group experienced a better QoL and state of mind, better illness understanding and a longer survival, with less aggressive treatment at the end of life (Figure 1). This study and two other randomized studies (16,17) are considered ‘landmark studies’ for the implementation of EPC in the day-to-day care since they all showed better QoL in the EPC group (18). Is this effect on QoL primarily caused by better symptom control? Is this the effect of more attention for the other domains by more social, psychological and spiritual support? Or is it influenced by early communication on the palliative setting, with consequently a better illness understanding and less aggressive therapy? Until now, the answers are unclear and need further investigation.

In practice, EPC has not been applied yet (6). Most likely, this has to do with operational reasons such as lack of time and insufficient resources to work out such a care pathway. Furthermore, there are hospitals without palliative units but with a palliative team having limited resources.
Understanding the disease
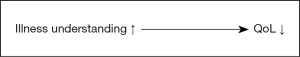
Patients with better understanding of their disease choose more often for symptom control and less for an aggressive treatment at the end of life (19). Until now, limited research has been done with regard to illness understanding in patients with lung cancer. Two recent studies have shown that in patients with either gastro-intestinal or hematological malignancies, who did not receive EPC, a better disease insight was correlated with a reduced QoL and more distress (10,20). Another study concludes that patients with advanced lung cancer, who show a certain degree of denial, have a better QoL (21,22). These data suggest that disease insight implies reduced QoL (Figure 2).
Influence of illness understanding on QoL in patients with advanced lung cancer
Informing the patient and his/her family of the consequences and prognosis of their disease is an important part of EPC and needs to be undertaken by the treating oncologist. The available evidence suggests a possible negative interaction between illness understanding and QoL (Figure 1). On the other hand, there is a positive interaction between EPC and Illness Understanding and between EPC and QoL (Figure 2). Figure 3 amalgamates these two previous figures and suggests that EPC has a protective effect on the relation between illness understanding and QoL. This is a relevant question for a physician. Can a patient be informed of his prognosis from the diagnosis onwards without detrimental effect on QoL? It seems that this is only possible if the necessary preconditions, namely EPC with holistic support of the patient and his/her family, are met.
Conclusions
Illness Understanding by the treating oncologist is an important part in the treatment of patients with advanced lung cancer. Based on the limited available literature about illness understanding, it seems that an EPC program is necessary when breaking bad news, in order to maintain or improve QoL in patients. Illness Understanding seems to be a curse but can become a blessing when EPC is offered. Whether the relation between illness understanding and QoL is different in patients with or without EPC is matter of further research.
Acknowledgements
A Coene for linguistic support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013;49:1374-403. [Crossref] [PubMed]
- Pilkington G, Boland A, Brown T, et al. A systematic review of the clinical effectiveness of first-line chemotherapy for adult patients with locally advanced or metastatic non-small cell lung cancer. Thorax 2015;70:359-67. [Crossref] [PubMed]
- Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 2011;61:212-36. [Crossref] [PubMed]
- World Health Organization. WHO Definition of Palliative Care. Available online: http://www.who.int/cancer/palliative/definition/en/, accessed 18 Novembre 2015.
- Chemotherapy in non-small cell lung cancer: a meta-analysis using updated data on individual patients from 52 randomised clinical trials. Non-small Cell Lung Cancer Collaborative Group. BMJ 1995;311:899-909. [Crossref] [PubMed]
- Charalambous H, Pallis A, Hasan B, et al. Attitudes and referral patterns of lung cancer specialists in Europe to Specialized Palliative Care (SPC) and the practice of Early Palliative Care (EPC). BMC Palliat Care 2014;13:59. [Crossref] [PubMed]
- The AM, Hak T, Koëter G, et al. Collusion in doctor-patient communication about imminent death: an ethnographic study. BMJ 2000;321:1376-81. [Crossref] [PubMed]
- Weeks JC, Catalano PJ, Cronin A, et al. Patients' expectations about effects of chemotherapy for advanced cancer. N Engl J Med 2012;367:1616-25. [Crossref] [PubMed]
- Chen AB, Cronin A, Weeks JC, et al. Expectations about the effectiveness of radiation therapy among patients with incurable lung cancer. J Clin Oncol 2013;31:2730-5. [Crossref] [PubMed]
- El-Jawahri A, Traeger L, Park ER, et al. Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer 2014;120:278-85. [Crossref] [PubMed]
- Cherlin E, Fried T, Prigerson HG, et al. Communication between physicians and family caregivers about care at the end of life: when do discussions occur and what is said? J Palliat Med 2005;8:1176-85. [Crossref] [PubMed]
- Mack JW, Cronin A, Taback N, et al. End-of-life care discussions among patients with advanced cancer: a cohort study. Ann Intern Med 2012;156:204-10. [Crossref] [PubMed]
- Pardon K, Deschepper R, Vander Stichele R, et al. Preferred and actual involvement of advanced lung cancer patients and their families in end-of-life decision making: a multicenter study in 13 hospitals in Flanders, Belgium. J Pain Symptom Manage 2012;43:515-26. [Crossref] [PubMed]
- Bauman JR, Temel JS. The integration of early palliative care with oncology care: the time has come for a new tradition. J Natl Compr Canc Netw 2014;12:1763-71; quiz 1771.
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009;302:741-9. [Crossref] [PubMed]
- Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 2014;383:1721-30. [Crossref] [PubMed]
- Yoong J, Park ER, Greer JA, et al. Early palliative care in advanced lung cancer: a qualitative study. JAMA Intern Med 2013;173:283-90. [Crossref] [PubMed]
- Mack JW, Weeks JC, Wright AA, et al. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 2010;28:1203-8. [Crossref] [PubMed]
- El-Jawahri A, Traeger L, Kuzmuk K, et al. Prognostic understanding, quality of life and mood in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 2015;50:1119-24. [Crossref] [PubMed]
- Vos MS, Putter H, van Houwelingen HC, et al. Denial in lung cancer patients: a longitudinal study. Psychooncology 2008;17:1163-71. [Crossref] [PubMed]
- Vos MS, Putter H, van Houwelingen HC, et al. Denial and social and emotional outcomes in lung cancer patients: the protective effect of denial. Lung Cancer 2011;72:119-24. [Crossref] [PubMed]


