Editor’s note:
“Palliative Radiotherapy Column” features articles emphasizing the critical role of radiotherapy in palliative care. Chairs to the columns are Dr. Edward L.W. Chow from Odette Cancer Centre, Sunnybrook Health Sciences Centre in Toronto and Dr. Stephen Lutz from Blanchard Valley Regional Cancer Center in Findlay, gathering a group of promising researchers in the field to make it an excellent column. The column includes original research manuscripts and timely review articles and perspectives relating to palliative radiotherapy, editorials and commentaries on recently published trials and studies.
Re-irradiation for painful bone metastases: evidence-based approach
Introduction
Bone pain secondary to bone metastases is the most common cancer-related pain syndrome requiring treatment (1). With bone metastases occurring in 50% of advanced cancer patients (2,3), the management of bone pain is an important consideration for health care professionals involved in the care of such patients. Radiotherapy (RT) is widely considered to be an effective way to palliate pain arising from bone metastases, and its efficacy has been established through a number of randomized controlled trials (4). With the advent of increasingly effective systemic treatment and better supportive care, the prognosis of patients with bone metastases has improved (5). As such, a growing number of bone metastases patients outlive the duration of benefits from their initial treatment of RT (5). Moreover, a number of patients fail to initially respond to RT (5). Given these facts, re-irradiation (re-RT) may be required in at least three scenarios (5):
- No pain relief after first-time radiation;
- Partial response to first time radiation and those in whom a better response is desired;
- Pain relapse after either partial or complete response to the first time radiation.
While there is limited evidence that initial non-responders would respond to re-RT (6), re-RT has been shown to be an effective treatment, especially in patients with responses to initial RT (7,8). Most notably, in a systematic review and meta-analysis analyzing 527 evaluable patients from seven studies, Huisman et al. found pain response after re-RT in 58% of patients (6). In addition, in another systemic review to determine the efficacy of re-RT in patients with bone metastases published in 2014, Wong et al. found complete, partial and overall response rates to be 20%, 50% and 68%, respectively (1).
Despite the acknowledgement of re-RT as an effective treatment for specific patients, until recently, evidence on the optimal dose fractionation schedules for painful bone metastases has been lacking (9). Given new evidence-based findings, the purpose of the current review is to provide an update on the new findings in the area of re-RT and to outline the optimal re-RT dose fractionation in the treatment of painful bone metastases.
Background on re-RT
The lowest optimal single fraction RT dose in the treatment of painful bone metastases was first determined by Jeremic et al. in a randomized controlled trial of 4, 6, and 8 Gy single fraction treatments published in 1998 (10). The Jeremic et al. study confirmed 8 Gy to be the lowest optimal single fraction RT. While both 6 and 8 Gy treatments were found to be superior to the 4 Gy single fraction treatment in terms of both complete and overall response rates, many patients were retreated during the study (8). Jeremic et al. noted that since the 4 Gy treatment produced overall response rates of 45-60%, the 4 Gy treatment could thus be advantageous in cases where re-treatments are sought or where large fields are treated (10).
In 1999, Jeremic et al. published a follow-up study investigating the effectiveness of a 4 Gy treatment for re-treatment of bone metastases following single-fraction RT with either 4, 6, or 8 Gy doses (8). The study found that 74% of patients responded and, of the 26 initial non-responders, 12 (46%) responded. In addition, patients with previous complete response were more likely to achieve complete response than patients with previous partial response (P=0.042). The authors concluded that a 4 Gy single fraction RT treatment was effective for re-treatment after a single fraction RT (8).
Jeremic et al. published an additional study in 2002, investigating the efficacy of a second 4 Gy single fraction RT treatment for patients with painful bone metastasis who had previously received single fraction RT twice already (4, 6, or 8 Gy plus 4 Gy) (11). The study found overall response rate to be 80%, with no difference between previous responders and non-responders with respect to complete or partial response (11). The authors thus concluded that a third single fraction RT of 4 Gy was effective and not toxic in the treatment of painful bone metastasis (11).
While the efficacy of re-treatment was established, the optimal schedule of repeat RT was not established until recently. This review thus serves as un-update for the literature given the emergence of recent evidence-based findings.
Single versus multiple fractions of repeat radiation for painful bone metastases
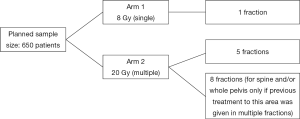
The first randomized controlled trial to assess the appropriate schedule of repeat RT to palliate pain from bone metastases was published in 2014 (9). This non-inferiority trial was conceived, undertaken, and analyzed by the National Cancer Institute of Canada Clinical Trials Group (NCIC CTG) Symptom Control (SC20) and accrued 850 patients from 92 centers in nine countries worldwide. Between January 2004, and May 2012, 850 patients were randomly assigned to receive 8 Gy in a single fraction or 20 Gy in multiple fractions (Figure 1). Karnofsky Performance Status (KPS) was required to be greater or equal to 50 and the interval between the last fraction of initial radiation and the date of randomization had to be at least 4 weeks. Patients with clinical or radiological evidence of spinal cord compression, pathological fracture, or impending fracture for surgical fixation were excluded. Other exclusion criteria included prior palliative surgery, systemic RT (Sr-89), or half-body irradiation (HBI) within 30 days. The primary endpoint of the study was overall pain response at 2 months, with overall response being defined as the sum of complete and partial responses to treatment. Secondary endpoints included freedom from pain progression, reduction in functional interference of daily activities, incidence of acute radiation-related side effects as assessed by an acute toxicity questionnaire 7 and 14 days after the start of treatment, incidence of in-field pathological fractures and spinal cord compression, and patient-reported quality of life (QoL) as assessed by the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTC QLQ-C30).
The authors found that 250 (48%) of all patients who received their assigned treatment had reduced pain at the site of repeat radiation or reduced need for opioid analgesia. In addition, 68% of 466 patients with available data had improved QoL pain scores, with no significant difference between the two arms at baseline or follow-up. In the intention-to-treat population, 28% of 425 patients allocated to 8 Gy treatment had an overall response while 32% of 425 patients allocated to 20 Gy treatment had an overall response to treatment (P=0.21; response difference of 4%). As the upper limit of the 95% confidence interval (CI), 9.2, was less than the pre-specified non-inferiority margin of 10%, the authors concluded that treatment with 8 Gy given in a single fraction is non-inferior to treatment with 20 Gy in multiple fractions. In the per-protocol population, 45% of 258 patients and 51% of 263 patients had an overall pain response to treatment (P=0.17; response difference 6%). However, since the upper limit of the 95% CI, 13.2, was greater than the pre-specified non-inferiority margin of 10%, per-protocol analysis did not show 8 Gy in a single fraction to be non-inferior.
Furthermore, lack of appetite (56% of assessable patients receiving 8 Gy and 66% of assessable patients receiving 20 Gy) and diarrhea (23% of assessable patients receiving 8 Gy and 31% of assessable patients receiving 20 Gy) were the most frequently reported acute-radiation related toxicities at 14 days. More patients from the multiple fraction arm experienced various acute adverse effects on both days 7 and 14, however, pain progression was similar between the two groups. In addition, 7% of 425 patients in the 8 Gy group and 5% of 425 patients in the 20 Gy group had pathological fracture, while 2% in the 8 Gy group and <1% in the 20 Gy group had spinal cord or cauda equina compression.
Given these findings, the authors concluded that repeat radiation does seem to be beneficial for patients with symptomatic bone metastases. Moreover, a single treatment with 8 Gy is non-inferior to treatment with 20 Gy in multiple fractions as in the intention-to-treat analysis. However, because the per-protocol analysis did not show 8 Gy treatment to be non-inferior, the authors acknowledged that a small proportion of patients may benefit from more protracted fractionation, although such patients might experience greater acute toxicity and inconvenience under this treatment.
Impact of re-RT of painful bone metastases on QoL and function
In addition to establishing the non-inferiority of a single 8 Gy for radiation retreatment, analysis of the SC20 database allowed for investigation into further characteristics of re-RT. In particular, while the NCIC CTG SC20 trial showed that 45% of those receiving a single 8 Gy and 51% receiving 20 Gy had an overall response to repeat RT (9), patients that require repeat radiation often have more extensive disease burden (1). Thus, to determine whether re-RT has the potential to improve bone metastases patients’ QoL and function, a secondary analysis of the SC20 database was performed (12).
This study utilized the SC20 database to evaluate whether response, as determined by the International Consensus Endpoint (ICE) and the brief pain inventory pain score (BPI-PS), is associated with improved QoL as assessed by the EORTC QLQ-C30 and functional interference scale of the brief pain inventory (BPI-FI). Of the 850 patients from the original database, 528 patients were evaluable for response using the ICE and 605 using the BPI-PS. Two-hundred and fifty-three patients experienced a response with the ICE, while 275 did not. The authors found that responding patients had superior scores on all items of the BPI-FI as well as improved QoL, as determined by the EORTC QLQ-C30 scales. Likewise, similar results were obtained using the BPI-PS. Given such findings, the authors concluded that patients responding to re-RT experience superior QoL scores as well as less functional interference. As such, patients should be offered re-RT to both reduce pain severity and improve QoL and pain interference (12).
Effect of re-RT for painful bone metastases on urinary markers of osteoclast activity
While the NCIC CTG SC20 study has confirmed the benefit of repeat radiation therapy and has observed this benefit in patients who both did and did not respond to initial treatment (9), there does exist a small group of patients who seem to be non-responsive to any amount of palliative RT (13). A supplementary study to the UK Bone Pain RT Trial (14) concluded that RT-mediated inhibition of bone resorption caused by osteoclastic activity might predict responses to RT. As the examination of urinary markers would aid to confirm this possibility, a further companion study to the NCIC CTG SC20 was done to investigate this issue (13). The investigators correlated urinary markers of osteoclast activity with response to re-RT, survival, and skeletal related events (13). Specifically, the study correlated the urinary markers of bone turnover [pyridinoline (PYD), deoxypyridinoline (DPD), N-telopeptide (NTX), Alpha and Beta cross-laps of C-telopeptide (CTX)] before and 1 month after re-RT with response to re-RT, to initial and re-RT, and then to either or none. Patients were then categorized as frequent responders (response to both initial and re-RT), eventual responders (response to re-RT only), eventual non-responders (response to initial radiation only), and absolute non-responders (no response to both). The authors found significant differences for PYD and DPD between responders and non-responders at baseline. Moreover, urinary markers were noticeably higher at both baseline and follow-up and there was a statistically significant difference for DPD at baseline (13).
The findings of this study suggest a biological relationship between bone markers and response to re-RT. The authors noted that given the fact that absolute non-responders have elevated urinary markers of bone turnover, it may be beneficial to reduce or normalize levels of bone markers in these patients before palliative RT with bone modifying agents. They further recommended that more research be done to determine whether such biomarkers can be developed in order to provide patients and radiation oncologists with more prognostic information with which to make treatment decisions (13).
Further confirmation of the comparable efficacy of a single fraction initial treatment and re-treatment: pooled overall response rates
Further support for a single fraction of radiation at both initial treatment and retreatment was published in April of 2014. Bedard et al. noted that while results from the NCIC CTG SC20 study provided overall response rates of initial treatment and retreatment alone, pooled overall response rates in patients treated with both initial and retreatment radiation are unknown. As such, the objective of their study focused on determining the overall response rates in patients undergoing initial and re-RT and comparing them between the different fractionation regimens (15). To determine the pooled response rates for first and second-time radiation, statistics from a systematic review of palliative RT trials for bone metastases (4) and from the NCIC CTG SC20 trial (9) were collected from the intent-to-treat and evaluable patient populations. The authors found that 71-73% of patients in the intent-to-treat calculation had an overall response to RT while 85-87% of patients in the evaluable population did so. Furthermore, the overall response rates were almost identical between single and multiple fraction treatment groups. As such, the authors recommended that patients with painful uncomplicated bone metastases be treated with a single fraction of 8 Gy for both initial treatment and retreatment, echoing the findings of the systematic review of initial radiation studies (4) and the NCIC CTG SC20 trial (9).
Conclusions
The current review sought to update the literature on findings in the area of re-RT. In particular, with the recent publication of the NCIC CTG SC20 trial, evidence now exists that treatment with 8 Gy in a single fraction for re-RT seems to be non-inferior and less toxic than 20 Gy in multiple fractions. In addition, patients responding to re-RT have been found to experience superior QoL and complain of less functional interference from pain; as such, patients with bone metastases should be offered re-treatment to reduce pain severity and improve QoL. Further support for the use of single fraction radiation at both initial treatment and retreatment has also been published. Despite such findings, some specific patients will never respond to initial radiation or re-RT. New findings have found significant differences in bone markers between responders and non-responders, thus opening the possibility for further research into the use of such biomarkers for predicting prognosis and for the guidance of consequent treatment decisions.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wong E, Hoskin P, Bedard G, et al. Re-irradiation for painful bone metastases - a systematic review. Radiother Oncol 2014;110:61-70. [PubMed]
- Uppelschoten JM, Wanders SL, de Jong JM. Single-dose radiotherapy (6 Gy): palliation in painful bone metastases. Radiother Oncol 1995;36:198-202. [PubMed]
- Mercadante S. Malignant bone pain: pathophysiology and treatment. Pain 1997;69:1-18. [PubMed]
- Chow E, Zeng L, Salvo N, et al. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 2012;24:112-24. [PubMed]
- Chow E, Hoskin PJ, Wu J, et al. A phase III international randomised trial comparing single with multiple fractions for re-irradiation of painful bone metastases: National Cancer Institute of Canada Clinical Trials Group (NCIC CTG) SC 20. Clin Oncol (R Coll Radiol) 2006;18:125-8. [PubMed]
- Huisman M, van den Bosch MA, Wijlemans JW, et al. Effectiveness of reirradiation for painful bone metastases: a systematic review and meta-analysis. Int J Radiat Oncol Biol Phys 2012;84:8-14. [PubMed]
- Mithal NP, Needham PR, Hoskin PJ. Retreatment with radiotherapy for painful bone metastases. Int J Radiat Oncol Biol Phys 1994;29:1011-4. [PubMed]
- Jeremic B, Shibamoto Y, Igrutinovic I. Single 4 Gy re-irradiation for painful bone metastasis following single fraction radiotherapy. Radiother Oncol 1999;52:123-7. [PubMed]
- Chow E, van der Linden YM, Roos D, et al. Single versus multiple fractions of repeat radiation for painful bone metastases: a randomised, controlled, non-inferiority trial. Lancet Oncol 2014;15:164-71. [PubMed]
- Jeremic B, Shibamoto Y, Acimovic L, et al. A randomized trial of three single-dose radiation therapy regimens in the treatment of metastatic bone pain. Int J Radiat Oncol Biol Phys 1998;42:161-7. [PubMed]
- Jeremic B, Shibamoto Y, Igrutinovic I. Second single 4 Gy reirradiation for painful bone metastasis. J Pain Symptom Manage 2002;23:26-30. [PubMed]
- Chow E, Meyer RM, Chen BE, et al. Impact of reirradiation of painful osseous metastases on quality of life and function: a secondary analysis of the NCIC CTG SC.20 randomized trial. J Clin Oncol 2014;32:3867-73. [PubMed]
- Chow E, DeAngelis C, Chen BE, et al. Effect of re-irradiation for painful bone metastases on urinary markers of osteoclast activity (NCIC CTG SC.20U). Radiother Oncol 2015;115:141-8. [PubMed]
- Hoskin PJ, Stratford MR, Folkes LK, et al. Effect of local radiotherapy for bone pain on urinary markers of osteoclast activity. Lancet 2000;355:1428-9. [PubMed]
- Bedard G, Hoskin P, Chow E. Overall response rates to radiation therapy for patients with painful uncomplicated bone metastases undergoing initial treatment and retreatment. Radiother Oncol 2014;112:125-7. [PubMed]


