Editor’s note:
“Palliative Radiotherapy Column” features in articles emphasizing the critical role of radiotherapy in palliative care. Chairs to the columns are Dr. Edward L. W. Chow from Odette Cancer Centre, Sunnybrook Health Sciences Centre in Toronto and Dr. Stephen Lutz from Blanchard Valley Regional Cancer Center in Findlay, gathering a group of promising researchers in the field to make it an excellent column. The column includes original research manuscripts and timely review articles and perspectives relating to palliative radiotherapy, and editorials and commentaries on recently published trials and studies as well.
Brain metastases: advances over the decades
Introduction
The burden of brain metastases is significant. Population-based publications estimate the incidence of brain metastases to range from 8.3-14.3 per 100,000 population. The incidence among cancer patients ranges from 8.5-9.6% (1). The most common primary site is lung. Other common primary sources of brain metastases are melanoma, renal, breast, and colorectal cancers (2). Eight-five percent of brain metastases are found in the cerebral hemisphere. A minority, 10-15% are located in the cerebellum and 1-3% are located in the brainstem (3).
Presenting symptoms include symptoms of mass effect such as headaches, nausea, vomiting. Depending on the location of the brain metastases, other symptoms may include focal weakness, confusion, gait ataxia, seizures, speech difficulty, visual disturbance, sensory disturbance and limb ataxia.
The morbidity and mortality associated with brain metastases make this problem a formidable challenge faced by health care professionals and caregivers who look after these patients. A patterns of care study (4) reported on 98 patients with newly diagnosed brain metastases. Median overall survival of these patients after brain radiotherapy was 2.7 months (80 days). Twenty-nine percent of these patients presented to the emergency department or were admitted to the hospital for acute care 2 or more times during the last 6 months of life. Sixty-eight percent of patients were referred to palliative care. The median survival from palliative care referral to death was 27 days. Ultimately, it was concluded that these patients would benefit from palliative care as they have high symptom burden. However, for this cohort of patients, referrals to palliative care were late in the dying process.
Objective
The aim of this review is to summarize management for patients with brain metastases, with a particular focus on symptom management.
Materials and methods
A systematic review of the literature was performed using Medline (1946-April week 4, 2015), PubMed and Cochrane databases (1991-April 30, 2015). Randomized controlled trials with adult (age 18 or over) patients were included and only English language articles were included. Outcomes of interest included survival, brain control (local and whole brain). In particular, symptom control (quality of life, neurological function and neurocognition) were examined.
Results
Steroids vs. steroids and whole brain radiotherapy (WBRT)
Clinical practice guidelines (5) recommend the use of steroids to provide temporary relief of symptoms due to intracerebral edema from brain metastases. The steroid of choice is dexamethasone and the starting dose of 4-8 mg per day was suggested. However, if a patient experiences severe symptoms of increased intracranial pressure, higher doses such as 16 mg per day or more should be considered.
The only contemporary randomized trial that has examined the use of optimal supportive care vs. optimal supportive care and WBRT was the QUARTZ trial (6). An interim analysis (reporting on 151 patients out of a planned 534 patients) indicated no early evidence of detrimental quality of life, overall survival or quality-adjusted life years (QALYs) between the two arms. In this interim analysis, 8% (12/151), 42% (64/151), and 50% (75/151) were classified as Radiation Therapy Oncology Group (RTOG) recursive partitioning analysis (RPA) classes I, II, III respectively.
Overall survival between the two arms was similar 49 days for optimal supportive care and WBRT vs. 51 days for optimal supportive care alone (hazard ratio 1.11, 95% CI: 0.80-1.53). The final trial results have been published in abstract form (7). For the 538 patients recruited, there was no significant difference in overall survival (hazard ratio 1.05, 95% CI: 0.89-1.26). The median survival of optimal supportive care and WBRT vs. optimal supportive care alone was 65 vs. 57 days, respectively. Overall quality of life or steroid use was no different between the two arms.
An older trial (8) randomized patients to prednisone with or without WBRT. The proportion of patients with improved performance status was similar between the two arm and median survival was 10 weeks in the steroid alone arm vs. 14 weeks in the combined arm (P value not stated).
It has been estimated that approximately 28% of patients treated with WBRT are able to taper off steroids completely after WBRT, while another 27% are able to reduce steroids (9). In general, a taper when possible is recommended to avoid the long-term side effects of steroid use. However, a proportion of patients will not be able to taper off steroids completely due to continued symptoms of brain edema, in which case the minimal amount of steroids to alleviate symptoms is recommended (10).
In an editorial by Jones and Simone (11), the fundamental question on the impact of WBRT on quality of life especially in patients with short survival was raised. In these patients, the challenges in defining realistic goals of care and evaluating trade-offs in terms of possible benefits and the shortcomings of medical intervention were brought to the forefront.
Prognostic grading
It is also important to recognize that patients with brain metastases represent a wide spectrum of patients with variable prognosis. Based on the RTOG graded prognostic assessment (GPA), survival may range from short prognoses (e.g., lung cancer from a median overall survival of 4.9 months) to longer prognoses (e.g., breast cancer with a median overall survival of 18.74 months) (12). Although ultimately not curable, patients with longer prognoses likely benefit from optimal supportive care and brain metastases treatment. It would be important to analyze the results from the QUARTZ trial to ascertain whether there may be subgroups of patients with brain metastases who may benefit from radiation treatment. In particular, based on the preliminary publication (6) 50% of the patients in the QUARTZ trial were classified as RTOG class III and 40% were classified as RTOG class II. These represent patients with poor prognoses. A very small minority (8% of patients) were RTOG class I patients. Furthermore, the QUARTZ trial only examined patients treated with WBRT and the larger question of whether good prognoses patients who are eligible for other interventions such as radiosurgery might benefit in terms of survival, quality of life, reduction in steroid use was not addressed.
Seizures
A meta-analysis of six randomized controlled trials including 547 patients with brain tumours (13) reported that those patients with brain tumours who received prophylactic antiepileptic drugs did not significantly lower seizure incidence as compared to the group who did not receive prophylactic antiepileptic drugs. As such, there is evidence to support not using prophylactic anti-seizure medications in patients with a diagnosis of brain metastases but without a history of seizures.
Similarly, a Cochrane meta-analysis (14) found no difference between the use of prophylactic anti-seizure medications vs. no anti-seizure prophylaxis in preventing a first seizure in patients with brain tumours. The risk of adverse side effects was higher in those on prophylactic anti-epileptics than those not on anti-seizure medications (number needed to harm 3; relative risk 6.10, 95% CI: 1.10-34.63, P=0.046).
Anti-seizure medications should however, be given as treatment for brain metastases patients who have a history of seizure. Non-enzyme inducing anti-seizure medications with less drug interactions (such as levetiracetam) are emerging as the preferred category of anti-epileptics (15).
WBRT altered fractionation schemes
Standard WBRT doses include 3,000 cGy in 10 daily fractions and 2,000 cGy in 5 daily fractions. No altered fractionation WBRT scheme was found to be superior to standard fractionation in terms of overall survival, symptom control and neurological function (16).
WBRT radiosensitizers
The addition of radiosensitizers (such as lonidamide, metronidazole, misonidazole, motexafin gadolinium, bromodeoxyuridine and efaproxiral) does not improve overall survival or brain response as compared to WBRT alone. Outside clinical trials, radiosensitizers is not recommended with WBRT (16).
Surgery for single brain metastasis
Randomized trials support the use of surgery to improve survival as compared to WBRT alone in selected patients with controlled systemic disease and a resectable single brain metastasis (17-19). The histologies excluded in the trials on the use of surgery were radiosensitive histologies such as small cell lung cancer, lymphoma, leukemia and germ cell tumors. The use of postoperative WBRT for patients with resected brain metastasis improves overall brain control but does not improve survival (20).
However, the use of WBRT has been shown to negatively affect neurocognition and quality of life (21-24), such that experimental strategies (e.g., surgery for single brain metastasis followed by postoperative cavity radiosurgery or focal postoperative cavity radiation or radiosurgery alone) to avoid WBRT have emerged.
Radiosurgery
Throughout the 1980s to mid-2000, the randomized trials in brain metastases centered on altered WBRT radiation schemes, surgery for single brain metastasis and the use of radiosensitizers added to WBRT. For approximately the last two decades, the trend in radiation brain metastases research has shifted to focused radiation techniques such as radiosurgery and neurocognitive outcomes.
Several trials have reported on the use of radiosurgery alone vs. radiosurgery and WBRT (21,22,25,26). The inclusion criteria for these radiosurgery trials were good performance status patients with 1-4 brain metastases less than 4 cm in size and inactive extracranial disease. These trials are consistent in demonstrating the improved whole brain control with the use of adjuvant WBRT added to radiosurgery. In all but one trial (21), overall survival is not different with the use of radiosurgery and WBRT as compared to radiosurgery alone. Two trials (21,22) reported worsening in neurocognitive function at 3-4 months after adjuvant WBRT as compared to radiosurgery alone.
In 2014, the American Society for Radiation Oncology (ASTRO) released the following Choosing Wisely statement:
“Don’t routinely add adjuvant whole brain radiation therapy to stereotactic radiosurgery for limited brain metastases.
Randomized studies have demonstrated no overall survival benefit from the addition of adjuvant whole brain radiation therapy (WBRT) to stereotactic radiosurgery (SRS) in the management of selected patients with good performance status and brain metastases from solid tumors. The addition of WBRT to SRS is associated with diminished cognitive function and worse patient-reported fatigue and quality of life. These results are consistent with the worsened, self-reported cognitive function and diminished verbal skills observed in randomized studies of prophylactic cranial irradiation for small cell or non-small cell lung cancer. Patients treated with radiosurgery for brain metastases can develop metastases elsewhere in the brain. Careful surveillance and the judicious use of salvage therapy at the time of brain relapse allow appropriate patients to enjoy the highest quality of life without a detriment in overall survival. Patients should discuss these options with their radiation oncologist.”
Neurocognitive protection
In order to spare neurocognitive function with WBRT, a few experimental strategies such as hippocampal radiation sparing (27,28), and the use of medications such as memantine (29) and donepezil (30) have been used.
Cognitive decline in patients with brain metastases is multifactorial. Contributing factors include the brain metastases, medications such as anti-seizure medications, chemotherapy, pain medications and previous brain therapies such as radiation, surgery.
Memory decline with WBRT is thought to arise from depletion of neural stem cells in the sub-granular zone of the hippocampus. These neural stem cells are believed to play a role in replenishing depleted neurons. The hippocampus is rarely the site of brain metastases and as a result efforts to spare the hippocampus and thereby possibly spare memory decline with WBRT were undertaken. In the RTOG-0933 phase II trial, 42 patients were treated with hippocampal sparing WBRT. The authors reported that the use of hippocampal sparing WBRT was associated with preservation of memory and quality of life as compared to historical series of patients (31).
Pharmacologic strategies with the intent to spare cognition have also been studied. A randomized double-blind, placebo-controlled trial reported that memantine was well tolerated and had similar toxicity to placebo in patients treated with WBRT. Overall, patients treated with memantine had better delayed time to cognitive decline and reduced rate of decline in memory, executive function and processing speed as compared to placebo (29).
Another phase III randomized placebo-controlled trial examined the use of donepezil in patients treated with partial or WBRT. While donepezil did not improve overall composite cognitive scores, it did result in some improvement with respect to several cognitive functions, particularly among patients with greater baseline impairments (30).
Molecular agents
Targeted therapies for cancers differ from traditional chemotherapy agents. Chemotherapy affects doubling cells, is cytotoxic in action and tends not to be specific. On the other hand, targeted agents have a mixture of cytostatic and cytotoxic effects and they inhibit specific targets in cells. Over the past decade, targeted agents to treat cancers which commonly metastasize to brain have been developed. The classification of targeted therapies for cancer includes tyrosine kinase inhibitors, monoclonal antibodies and cancer vaccines (32).
Lung cancer
For lung cancer, epidermal growth factor receptor (EGFR) inhibitors such as erlotinib, gefitinib and afatinib are being used in EGFR mutant non-small cell lung cancer (NSCLC). For anaplastic lymphoma kinase (ALK) positive NSCLC, crizotinib is being used for patients who have locally advanced or metastatic disease. With respect to brain metastases in lung cancer, specifically, a randomized phase III trial of WBRT and radiosurgery vs. radiosurgery alone with either temozolomide or erlotinib was reported for 126 out of 381 planned patients (33). This trial closed due to poor accrual. The median survival times were worse for the WBRT and radiosurgery with temozolomide or erlotinib as compared to WBRT and radiosurgery alone (6.3 vs. 6.1 vs. 13.4 months respectively), although the differences did not reach statistical significance likely due to the small numbers. The addition of temozolomide or erlotinib was associated with more frequent grades 3-5 toxicity as compared to WBRT and radiosurgery alone (41% vs. 49% vs. 11%, respectively). Lack of tumour EGFR testing was a major limitation of this trial.
A few small prospective and retrospective series report brain metastases response with the use of EGFR targeted agents alone, without brain radiation (34-36).
Breast cancer
It is estimated that human epidermal growth factor receptor (HER2) overexpression occurs in approximately 20-30% of breast cancers (37). Targeted therapies which act on the HER2 pathway include monoclonal antibodies trastuzumab and tyrosine kinase inhibitors such as pazopanib, lapatinib, neratinib, and afatinib.
The LANDSCAPE prospective multi-institutional phase II trial (38) enrolled 45 HER2 positive breast cancer patients with brain metastases (who did not receive prior WBRT) to lapatinib and capecitabine. Intracranial response (all partial) was seen in 65.9% of patients. However 49% had grade 3 or 4 toxicity. But no grade 5 toxicities were noted.
Other studies have also supported the finding of intracranial response to lapatinib alone (39). In a multicenter phase II trial of lapatinib for salvage of 242 previously treated brain metastases patients with HER2-positive breast cancer, 6% experienced 50% or more volumetric reduction in brain metastases, 21% showed 20% or more volume reduction in brain metastases.
Melanoma
Drugs that treat melanoma driven by BRAF mutations such as dabrafenib and vemurafenib have been developed. In a multi-institutional phase II trial, dabrafenib was associated with 39.3% intracranial response in those patients who had no prior brain therapy and 30.8% brain response in those patients who had progressive metastases after previous brain therapy (40).
A few studies have also examined the use of vemurafenib alone in the treatment of brain metastases from melanoma and intracranial response varies from 37-50% (41,42).
Ipilimumab blocks cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and has been used experimentally either alone and with radiosurgery in a small number of patients with metastatic melanoma to brain (43,44).
In summary, the targeted agents have not been used routinely for the initial management of newly diagnosed brain metastases patients. The targeted therapy studies have focused largely on brain responses. Further research in this modality is needed to ascertain whether there is any survival, quality of life or symptom control benefit with these agents.
Discussion
The mainstay of management for patients with brain metastases presently includes the following (alone or in combination): optimal supportive care including the use of steroids, WBRT, radiosurgery, and surgery. Surgery or radiosurgery improves survival in selected patients with resectable single brain metastasis as compared to WBRT alone. The key to the management of patients with brain metastases is an assessment of patient, tumour and treatment factors. Prognostic scales such as the GPA (45) will help select patients with good prognoses likely to benefit from active brain management. Those with poor prognoses may be best managed with optimal supportive care without brain radiation.
Table 1 summarizes the trends in research for patients with brain metastases over the decades. There continues to be unanswered clinical questions in the area of radiosurgery, postoperative radiation for single brain metastasis, and molecular targeted agents for brain metastases. For example, should there be a limit on the number of brain metastases treated with radiosurgery? Will molecular targeted agents help in terms of survival, brain control and quality of life in the management of brain metastases? Will there be better pharmacologic agents used to improve symptoms in patients with brain metastases, such as drugs which reduce the symptoms of brain edema without the side effects of steroids or drugs which help with neurocognition? It is anticipated that further gains in the management of brain metastases will come in this decade and beyond as several of these questions become addressed in future research trials.
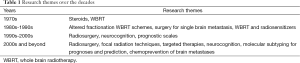
Full table
Acknowledgements
The author thanks Barb Zurowski for her secretarial assistance.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep 2012;14:48-54. [PubMed]
- Barnholtz-Sloan JS, Sloan AE, Davis FG, et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 2004;22:2865-72. [PubMed]
- Arbit E, Wronski M. The treatment of brain metastases. Neurosurg Q 1995;5:1-17. [PubMed]
- Stavas M, Arneson K, Friedman J, et al. From whole brain to hospice: patterns of care in radiation oncology. J Palliat Med 2014;17:662-6. [PubMed]
- Ryken TC, McDermott M, Robinson PD, et al. The role of steroids in the management of brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 2010;96:103-14. [PubMed]
- Langley RE, Stephens RJ, Nankivell M, et al. Interim data from the Medical Research Council QUARTZ Trial: does whole brain radiotherapy affect the survival and quality of life of patients with brain metastases from non-small cell lung cancer? Clin Oncol (R Coll Radiol) 2013;25:e23-30. [PubMed]
- Mulvenna PM, Nankivell MG, Barton R, et al. Whole brain radiotherapy for brain metastases from non-small lung cancer: Quality of life (QoL) and overall survival (OS) results from the UK Medical Research Council QUARTZ randomised clinical trial (ISRCTN 3826061). J Clin Oncol 2015;33:abstr 8005.
- Horton J, Baxter DH, Olson KB. The management of metastases to the brain by irradiation and corticosteroids. Am J Roentgenol Radium Ther Nucl Med 1971;111:334-6. [PubMed]
- Bezjak A, Adam J, Barton R, et al. Symptom response after palliative radiotherapy for patients with brain metastases. Eur J Cancer 2002;38:487-96. [PubMed]
- Sturdza A, Millar BA, Bana N, et al. The use and toxicity of steroids in the management of patients with brain metastases. Support Care Cancer 2008;16:1041-8. [PubMed]
- Jones JA, Simone CB 2nd. Whole brain radiotherapy for patients with poor prognosis: possibilities for the impact of the QUARTZ trial. Ann Palliat Med 2015;4:58-60. [PubMed]
- Sperduto PW, Chao ST, Sneed PK, et al. Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys 2010;77:655-61. [PubMed]
- Kong X, Guan J, Yang Y, et al. A meta-analysis: Do prophylactic antiepileptic drugs in patients with brain tumors decrease the incidence of seizures? Clin Neurol Neurosurg 2015;134:98-103. [PubMed]
- Tremont-Lukats IW, Ratilal BO, Armstrong T, et al. Antiepileptic drugs for preventing seizures in people with brain tumors. Cochrane Database Syst Rev 2008.CD004424. [PubMed]
- Pruitt AA. Medical management of patients with brain tumors. Continuum (Minneap Minn) 2015;21:314-31. [PubMed]
- Tsao MN, Lloyd N, Wong RK, et al. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev 2012;4:CD003869. [PubMed]
- Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 1990;322:494-500. [PubMed]
- Noordijk EM, Vecht CJ, Haaxma-Reiche H, et al. The choice of treatment of single brain metastasis should be based on extracranial tumor activity and age. Int J Radiat Oncol Biol Phys 1994;29:711-7. [PubMed]
- Vecht CJ, Haaxma-Reiche H, Noordijk EM, et al. Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 1993;33:583-90. [PubMed]
- Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: a randomized trial. JAMA 1998;280:1485-9. [PubMed]
- Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 2009;10:1037-44. [PubMed]
- Brown PD, Asher AL, Ballman KV, et al. NCCTG N0574 (Alliance): A phase III randomized trial of whole brain radiation therapy (WBRT) in addition to radiosurgery (SRS) in patients with 1 to 3 brain metastases. J Clin Oncol 2015;3:abstr LBA4.
- Gondi V, Paulus R, Bruner DW, et al. Decline in tested and self-reported cognitive functioning after prophylactic cranial irradiation for lung cancer: pooled secondary analysis of Radiation Therapy Oncology Group randomized trials 0212 and 0214. Int J Radiat Oncol Biol Phys 2013;86:656-64. [PubMed]
- Slotman BJ, Mauer ME, Bottomley A, et al. Prophylactic cranial irradiation in extensive disease small-cell lung cancer: short-term health-related quality of life and patient reported symptoms: results of an international Phase III randomized controlled trial by the EORTC Radiation Oncology and Lung Cancer Groups. J Clin Oncol 2009;27:78-84. [PubMed]
- Aoyama H, Shirato H, Tago M, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 2006;295:2483-91. [PubMed]
- Kocher M, Soffietti R, Abacioglu U, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 2011;29:134-41. [PubMed]
- Gondi V, Tomé WA, Mehta MP. Why avoid the hippocampus? A comprehensive review. Radiother Oncol 2010;97:370-6. [PubMed]
- Kazda T, Jancalek R, Pospisil P, et al. Why and how to spare the hippocampus during brain radiotherapy: the developing role of hippocampal avoidance in cranial radiotherapy. Radiat Oncol 2014;9:139. [PubMed]
- Brown PD, Pugh S, Laack NN, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol 2013;15:1429-37. [PubMed]
- Rapp SR, Case LD, Peiffer A, et al. Donepezil for Irradiated Brain Tumor Survivors: A Phase III Randomized Placebo-Controlled Clinical Trial. J Clin Oncol 2015;33:1653-9. [PubMed]
- Gondi V, Pugh SL, Tome WA, et al. Preservation of memory with conformal avoidance of the hippocampal neural stem-cell compartment during whole-brain radiotherapy for brain metastases (RTOG 0933): a phase II multi-institutional trial. J Clin Oncol 2014;32:3810-6. [PubMed]
- Owonikoko TK, Arbiser J, Zelnak A, et al. Current approaches to the treatment of metastatic brain tumours. Nat Rev Clin Oncol 2014;11:203-22. [PubMed]
- Sperduto PW, Wang M, Robins HI, et al. A phase 3 trial of whole brain radiation therapy and stereotactic radiosurgery alone versus WBRT and SRS with temozolomide or erlotinib for non-small cell lung cancer and 1 to 3 brain metastases: Radiation Therapy Oncology Group 0320. Int J Radiat Oncol Biol Phys 2013;85:1312-8. [PubMed]
- Ceresoli GL, Cappuzzo F, Gregorc V, et al. Gefitinib in patients with brain metastases from non-small-cell lung cancer: a prospective trial. Ann Oncol 2004;15:1042-7. [PubMed]
- Welsh JW, Komaki R, Amini A, et al. Phase II trial of erlotinib plus concurrent whole-brain radiation therapy for patients with brain metastases from non-small-cell lung cancer. J Clin Oncol 2013;31:895-902. [PubMed]
- Wu C, Li YL, Wang ZM, et al. Gefitinib as palliative therapy for lung adenocarcinoma metastatic to the brain. Lung Cancer 2007;57:359-64. [PubMed]
- Mitri Z, Constantine T, O'Regan R. The HER2 Receptor in Breast Cancer: Pathophysiology, Clinical Use, and New Advances in Therapy. Chemother Res Pract 2012;2012:743193.
- Bachelot T, Romieu G, Campone M, et al. Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol 2013;14:64-71. [PubMed]
- Lin NU, Diéras V, Paul D, et al. Multicenter phase II study of lapatinib in patients with brain metastases from HER2-positive breast cancer. Clin Cancer Res 2009;15:1452-9. [PubMed]
- Long GV, Trefzer U, Davies MA, et al. Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): a multicentre, open-label, phase 2 trial. Lancet Oncol 2012;13:1087-95. [PubMed]
- Dummer R, Goldinger SM, Turtschi CP, et al. Vemurafenib in patients with BRAF(V600) mutation-positive melanoma with symptomatic brain metastases: final results of an open-label pilot study. Eur J Cancer 2014;50:611-21. [PubMed]
- Harding JJ, Catalanotti F, Munhoz RR, et al. A Retrospective Evaluation of Vemurafenib as Treatment for BRAF-Mutant Melanoma Brain Metastases. Oncologist 2015;20:789-97. [PubMed]
- Margolin K, Ernstoff MS, Hamid O, et al. Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol 2012;13:459-65. [PubMed]
- Kiess AP, Wolchok JD, Barker CA, et al. Stereotactic radiosurgery for melanoma brain metastases in patients receiving ipilimumab: safety profile and efficacy of combined treatment. Int J Radiat Oncol Biol Phys 2015;92:368-75. [PubMed]
- Sperduto PW, Kased N, Roberge D, et al. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 2012;30:419-25. [PubMed]


