
Investigation of retro-orbicularis oculi fat and associated orbital septum connective tissues in upper eyelid surgery
Introduction
The aim of Asian blepharoplasty, besides creating an eyelid crease, should be to improve the eyelid’s efficiency in opening and crease formation (1). Repositioning the preseptal tissues may help to accomplish this, and any tissue impediment that works against crease formation should also be reduced. The preaponeurotic anterior space can be remodeled to improve tissue interaction and LPS (levator palpebrae superioris) retraction. Care should be taken to avoid adding impedance or load to the biodynamics of the eyelids (2-6).
Surgical techniques include suture ligation (non-incision) and external incision. Some surgeons have advocated removing some preaponeurotic fat as part of the blepharoplasty procedure. However, a relatively new concept of the importance of the preaponeurotic glide zone has been described by Chen (1). It is believed that the preaponeurotic space with its free fat layer acts as a glide zone that allows the posterior layer of the levator and muller’s muscle to contract smoothly upwards against the anterior layer of the skin and orbicularis, with little resistance. This facilitates the formation of the lid-fold with the crease and prevents the development of a sunken supratarsal sulcus with loss of the fullness and a stiff looking upper lid (3-5).
The removal of excess preaponeurotic volume including retro-orbicularis oculi fat (ROOF) and orbital septum fat (OSF), especially the removal of OSF (post-orbital septum volume), has long been the focus of the continuous developments in double eyelid surgery (7). However, the removal of ROOF (pre-orbital septum volume) has received little attention. The relationship between the orbital septum and its adjacent structures is complex, especially that with the ROOF (8). As part of the preaponeurotic volume, ROOF is considered to be a continuation of the brow fat pad. ROOF is prominent in East Asian people and shows great variation between individuals (9). However, based on surgical observational and cadaver dissection studies, we hypothesized that ROOF and the orbital septum are closely connected and have an important positional relationship, which may shed light on resistance to LPS. This study aimed to assess the position relationship between ROOf and orbital septum position in detail, as well as the effect of this relationship on LPS and the results of surgical remodeling of position relationship in order to inform the selection of appropriate methods to improve the eyelid’s efficiency in opening and crease formation in upper eyelid surgery.
High-resolution P45 sectional plasticization techniques have steadily improved and can be used to obtain valuable data on the normal anatomy of the eyelid. Recently, P45 plastination has become a powerful tool in scientific imaging in many areas of medicine (10,11). In this study, p45 sections of periorbital cadaver specimens were prepared, and images of the upper eyelid were analyzed.
We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1822).
Methods
Anatomic evaluation
Nineteen cadaver heads were subjected to anatomic evaluation, performed by the Department of Anatomy in the College of Basic Medical Sciences at Dalian Medical University, and the Center of Plastic and Aesthetic Surgery at the First Affiliated Hospital of Dalian Medical University. The cadaver heads were subjected to P45 sheet plastination, which is a technique for preserving tissue slices that retains the advantages of P35 and P40 technology, including being non-toxic and durable (12). Furthermore, this technique can simplify the manufacturing flow, reduce operation costs, and maintain specimens in their original state (13). We divided the tissue samples into five 6-mm-thick sagittal layers, from the medial canthus outward to the lateral canthus region (Figure 1). The layers were as follows: the medial canthus, the medial crest, the midpoint of the pupil, the lateral crest, the lateral canthus.

Patients
The Institutional Review Board of the Center of Plastic and Aesthetic Surgery at the First Affiliated Hospital of Dalian Medical University approved this study, which was performed according to the principles of the Declaration of Helsinki (as revised in 2013). Each patient gave informed consent.
Between January 2019 and December 2019, a grading system for the upper mean reflex distance was established by three plastic surgeons independent of this study. The extent of eye opening in all enrolled patients was graded preoperatively using the system and regraded after surgery. All patients had consistent grades for the upper eyelid on both sides and were followed up for at least 6 months. Patients meeting any of the following criteria were excluded: (I) cutis laxa; (II) a history of cosmetic surgery, such as periorbital injections or filling; (III) a history of periorbital trauma; (IV) a local skin infection and/or inflammation; (V) incomplete data or insufficient follow-up.
Surgical procedure
The procedure was performed on most patients under local anesthesia with 10 mg of diazepam (Valium) and 1,000 mg of acetaminophen (Tylenol), orally administered 30–45 minutes before the start of the procedure. Local injections of 0.75–1.0 cc of 2% xylocaine (with 1:100,000 dilution of epinephrine) were administered into each upper eyelid via the suborbicularis plane, using a 32-gauge ½-inch needle. The surgical technique used was described previously in “Trapezoidal debulking of eyelid tissues: application in Asian blepharoplasty” (14). Intraoperative observations included the presence or absence of ROOF, partial resection, or reposition. ROOF was removed to improve the restriction of the LPS and the position of the SRJ. In all cases, the wound was closed through skin-aponeurosis-skin. On the first day post surgery, the patients were advised to have bed rest, and cold compresses were applied locally. Topical antibiotic ointment was applied to the upper eyelids twice a day for 1 week. All sutures were removed after 1 week.
Satisfaction questionnaire
Each patient completed an anonymous questionnaire comprising the following two statements: (I) The extent of eye opening has been increased; and (II) the appearance of my upper eyelid has been improved. The patients were asked to respond to each statement using one of the following options: strongly disagree, disagree, neither agree nor disagree, agree, or strongly agree.
Results
Roof
The ROOF was divided into three portions. The upper, middle, and lower portions corresponded to the preorbital, preseptal orbital, and pretarsal portions, respectively. The midsection of the specimen had three groups of fasciae in the ROOF. The fasciae distributed over the upper, middle, and lower portions were referred to as the upper, middle, and lower fibers, respectively (Figure 2).
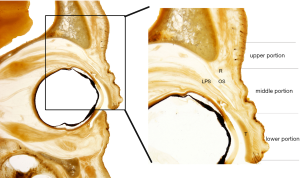
Upper portion
In the upper portion of the ROOF, the soft tissue space was small and the adipose tissue had more fibers than that in other portions. The fibers near the orbital septum and orbital bone increased and became denser and more distinct, running together with the fasciae on the muscle surfaces. Near the orbital bone, dense fibers increased in number and were wrapped around the blood vessels, due to the vascular crossing. Near the orbital margin where the orbital septum region begins, denser and clearer fibers were observed. The fibrous septum formed an interconnected reticular compartment. Some fibers ran on the surface of the orbicularis oculi. Irregular dense fibers were observed near the surface of the orbicularis oculi in the sagittal direction (Figure 2).
Middle portion
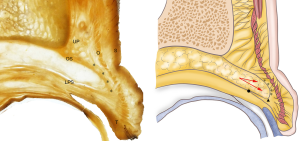
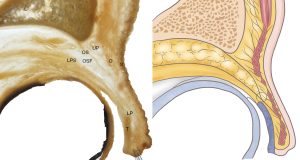
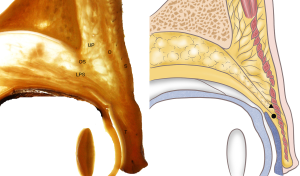
In the middle portion, the soft tissue space was very large. There were fewer fibers in the center of the middle portion, and the orbital septum was thick and clear. The adipose tissue had a linear shape and was larger than that in the other portions of the ROOF. In the inferior part of the portion, the SRJ was found to connect with the SAJ in three locations:
- In 63.2% of specimens, the SRJ was lower than the SAJ. These specimens were most influenced by herniation of the orbital fat. The orbital septum made a U-turn toward the tarsus, giving the ROOF an S shape. In type I specimens, the ROOF portion was pressed forward, and its thickness was reduced by the orbital septum (Figure 3).
- In 28.9% of specimens, the SRJ and the SAJ were in the same horizontal position. The orbital septum, including the orbital fat, consisted of several thin membranes instead of a single, thick membrane. The superior margin of the orbital septum was located close to the upper fibers. The septum itself was stretched forward and down toward the middle portion of the orbicularis oculi muscle, while the inferior margin was touching the aponeurosis of the upper eyelid and the lower part of the ROOF (Figure 4).
- In 2.9% of specimens, the SRJ was higher than the SAJ. The ROOF space was especially small. The fibers close to the orbicularis oculi muscle were still very dense and ran with the fasciae on the muscle surface, but the interspace was reduced. In these specimens, the lowest point of the orbital septum was inserted in front of the aponeurosis of the levator eyelid, into the orbicularis oculi muscle (Figure 5).
Lower portion
In three specimens, the ROOF space before the tarsus was small, and the structure could not be observed. In other specimens, the ROOF was extended after stretching to the middle portion, and the fibers between the muscle and orbital septum were sparse. There were clearly fewer fibers in the ROOF and the fat tissue than in the other portions. The muscle in the lower portion of the orbicularis oculi had an elliptical shape. A small amount of fibrous connective tissue originating from the orbicularis oculi muscle fascia and aponeurosis of the levator eyelid was present but extremely loose. Both the SAJ and the SRJ were higher than the superior tarsal margin (Figure 2).
Postoperative grading of the extent of eye opening showed that all 57 cases were of grade 1 or 2. Of the 34 cases categorized as grade 2 preoperatively, 30 (88.2%) improved to grade 1 after surgery. Although the grades of the remaining 4 (11.8%) cases showed no improvement, the upper eyelids of these patients appeared rejuvenated. Of the 15 cases preoperatively categorized as grade 3, 9 (60.0%) and 6 (40.0%) improved to grade 1 and grade 2, respectively. Of the 8 cases preoperatively categorized as grade 4, 2 (25.0%) and 6 (75.0%) improved to grade 1 and grade 2, respectively.
The second statement had a higher agreement rate than the first statement. None of the subjects strongly disagreed with either statement.
Patient 1
A 28-year-old woman underwent SRJ lifting. A significant improvement was seen in the patient’s grade for the upper mean reflex distance, which rose from grade 2 to grade 1. The differences in the patient’s complexion were caused by seasonal factors (Figure 6).

Patient 2
A 25-year-old woman with a sunken upper eyelid underwent SRJ lifting. The patient’s grade for the upper mean reflex distance significantly improved, from grade 3 to grade 1 (Figure 7).

Patient 3
A 35-year-old man with ptosis underwent SRJ lifting and additional levator aponeurosis migration. The patient’s grade for the upper mean reflex distance significantly improved, from grade 4 to grade 2 (Figure 8).

Discussion
ROOF was first described three decades ago after careful observation during upper eyelid surgery. However, this description was based on intraoperative findings, and the limited operative field prevented the anatomy of the ROOF from being fully explored (15). The relationships between the ROOF layer and other important structures in the periorbital region, including lateral orbital thickening, deep temporal fascia, and the zygomatio-temporal nerve, have only recently been elucidated (16).
In individuals with Asian ethnicity, ROOF participates in the formation of the upper eyelid. ROOF tissue that is too thick or too thin may result in an aged appearance. Therefore, to achieve a youthful appearance in the upper eyelid, the appropriate volume of ROOF is needed (17). The operative details of upper eyelid surgery are guided by this volume-related theory. At the same time, another important principle of upper eyelid surgery is to raise the position of the SAJ and reduce the load in front of the aponeurosis (18). However, the ROOF is located in the compartment adjacent to the orbital septum. As a fibrous fat pad, ROOF has yet to be the focus of analysis, and the specific relationship between the SRJ and the SAJ still needs to be researched.
In our study, the adipose structure of ROOF was not found to be wrapped; the space included ROOF and a large amount of connective tissue, so the author generally chose not to refer to it as a fat pad. ROOF fibers were observed to extend from the supra-orbital arch to the tarsal space but did not extend deep into the orbicularis. In their functional study of ROOF, Wang et al. (19) described ROOF and SOOF (suborbicularis oculi fat) as being continuous and concluded that ROOF was the basis of cases of excessively thick and sunken upper eyelids. Some of the fibers we observed were distributed across different regions; these fibers, which were mainly concentrated in the upper portion, adjacent to the orbital septum and the orbital margin, play a suspension and fixation role in the morphology of orbital septum function. Some studies on lower eyelid aging have shown convex fat of the lower eyelid caused by aging to compress the middle area of the orbital septum, SOOF, and orbicularis oculi muscle, and become medial (20). The orbital septum and ROOF could be considered as extremely weak membranes for sustaining pressure from orbital fat caused by aging-induced changes (21); this view considers the anterior projection of orbital septum fat as a motivating factor of orbital septum and ROOF weakening. However, considering the influence of gravity and the differences in ROOF in Asian individuals, we believe that ROOF and orbital fat exert mutual forces, which are not affected by aging. In other words, ROOF contains a larger number of fibers and has a blocking effect, which can effectively maintain the orbital septum and the separation function of the orbital septum.
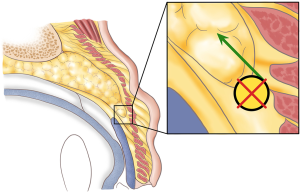
Although, according to the volume reduction theory, the anterior aponeurosis was believed to strengthen the levator palpebrae muscle, it actually exacerbated the problem. Specifically, the decrease in the volume of ROOF would reduce the tractive tension between the orbital septum and orbital septum fat, and accentuate forward bulging of the orbital septum fat (Figure 3). Our results further elucidate the function of ROOF and confirm the findings of our previous research (11). This article may be the first to report the morphological classification of ROOF.
The positional relationship between the SAJ and the SRJ
The junction between the orbital septum and the fascia levator was first reported as the SAJ by Dr. W (22). The position of the SAJ is generally believed to be higher in Caucasians than in Asians. Most scholars believe that the SAJ is always above the tarsal plate to the septoaponeurosis junction (TJD) through gross anatomy and histological observations (23). Interestingly, Huang found through histological measurement that part of the SAJ is below the TJD (18). In our study, the SAJ was above the TJD in all patients. In double eyelid surgery in Asians, fixing the position of the levator aponeurosis and reducing the fat volume in the anterior of the levator aponeurosis are considered as the baseline means for improving the functional efficiency and appearance of the upper eyelid (24). In particular, proper removal of orbital septum fat, ROOF, and orbicularis oculi muscle can effectively reduce the volume in the anterior of the levator aponeurosis, thus improving the retraction force of the levator muscle. However, in our study, the structure of the anterior tissue of the levator aponeurosis was found to be complex, especially the positional relationship between the orbital septum and ROOF. In 63.2% of specimens, the SRJ was lower than the SAJ, which also limited the effective retraction of the levator muscle. Unlike volume load, this SRJ position loads pressure on the levator muscle. From a mechanistic perspective, resistance to the retraction force of the levator muscle is disassembled in two directions: vertical upward and horizontal backward. The ROOF was in the direction of vertical resistance. If the position of the SRJ is too low or even lower than that of the SAJ, the resistance of the vertical force will increase, requiring more retraction force (Figure 9). Thus, the pressure load theory based on ROOF distribution is proposed for the first time. As ROOF is not wrapped, there are many fibers, which results in a closer connection with the orbital septum. In 2.9% of specimens in our study, all areas of the ROOF were filled with dense fibrous septum, while in other specimens, fibrous septum was mainly concentrated in the upper portion of the ROOF, while the lower ROOF fibers appeared to participate in filling the space of levator fibers in the anterior of the tarsus; this finding has not been reported in previous studies. To date, the role of ROOF in upper eyelid surgery has been underestimated.
Although lifting the SRJ was effective in this study, its outcomes differed somewhat between patients with different grades of upper eyelid opening. Additional aponeurosis migration was observed in grade 4 cases, while grade 3 and grade 4 cases had more ROOF removed, and the position of the SRJ and SAJ was improved by surgery. Thus, patients with grade 3 and 4 showed higher rates of improvement, both in extent of eye opening and in the appearance of the upper eyelid. Because patients with grade 2 do not have large amounts of soft tissue, tissue removal should be minimized. Patients with grade 2 showed higher rates of clear improvement. Self-assessments by grade 2 patients also revealed a low rate of disagreement with the statement “The appearance of my upper eyelid has been improved.”
Achieving the desired result in upper Asian blepharoplasty requires a thorough understanding of the unique anatomic features of the Asian upper eyelid that prevent the formation of an upper eyelid crease—namely, preaponeurotic fat and ROOF that extend inferiorly into the area overlying the superior tarsal border, which prevents interdigitations of the levator aponeurosis to the skin. Debulking of this prominent tissue in the pretarsal and lower preseptal plane (SRJ) allows for the creation of a more natural and efficiency crease.
The aim of this research was to examine ROOF. It is worth noting that the vessels and their branches also run inside ROOF, so some of the fibers we observed could belong to those structures. However, in regard to the development of upper eyelid operation, ROOF fibers and the location of the SRJ could affect the intraoperative treatment. We hope these results will serve as a foundation for hypotheses about the formation and appearance of double eyelids.
Conclusions
ROOF is a structural fat that exists in the upper eyelids of Asian adults. The function of ROOF may have been underestimated as an anatomical factor in double eyelid surgery. The position relationship between the SRJ and SAJ has a certain guiding role in the operation of double eyelid surgery. Lifting the SRJ can effectually improve the extent of eye opening and reduce resistance to LPS. Eyelid surgery should involve the careful evaluation of ROOF and the SRJ to properly guide the operation and to ensure a rejuvenated appearance of the upper eyelid is successfully achieved.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1822
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1822
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1822). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Institutional Review Board of the Center of Plastic and Aesthetic Surgery at the First Affiliated Hospital of Dalian Medical University approved this study, which was performed according to the principles of the Declaration of Helsinki (as revised in 2013). Each patient gave informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen WP. Literature on double eyelid surgeries: appendix 1,2,3. In: Asian Blepharoplasty and the Eyelid Crease. 3rd ed. Edinburgh/ New York: Elsevier; 2016:345-65.
- Fernandez LR. Double eyelid operation in the oriental in Hawaii. Plast Reconstr Surg Transplant Bull 1960;25:257-64. [Crossref] [PubMed]
- Boo-Chai K. Peroperative bleeding in the pre-tarsal (postaponeurotic) space in oriental blepharoplasty. Br J Plast Surg 2001;54:370. [Crossref] [PubMed]
- Mutou Y, Mutou H. Intradermal double eyelid operation and its follow-up results. Br J Plast Surg 1972;25:285-91. [Crossref] [PubMed]
- Chen WPD. Aesthetic eyelid surgery in Asians: an east-west view. Hong Kong J Ophthalmol 2000;3:27.
- Homma K, Mutou Y, Mutou H, et al. Intradermal stitch for orientals: does it disappear? Aesthetic Plast Surg 2000;24:289. [Crossref] [PubMed]
- Seiff SR, Seiff BD. Anatomy of the Asian eyelid. Facial Plast Surg Clin North Am 2007;15:309-v. [Crossref] [PubMed]
- Meyer DR, Linberg JV, Wobig JL, et al. Anatomy of the orbital septum and associated eyelid connective tissues. Ophthal Plast Reconstr Surg 1991;7:104-13. [Crossref] [PubMed]
- Liu D, Hsu WM. Oriental eyelids. Anatomic difference and surgical consideration. Ophthalmic Plast Reconstr Surg 1986;2:59-64. [Crossref] [PubMed]
- Gao J. Liu, S Yu, H Sui. A new polyester technique for sheet plastination. Brain Structure and Function. J Intl Soc Plastination 2006;21:7-10.
- Chun P, Yu S, Qin H, et al. The Use of P45 Plastination Technique to Study the Distribution of Preseptal and Preaponeurotic Fat Tissues in Asian Eyelids. Cell Biochem Biophys 2015;73:313-21. [Crossref] [PubMed]
- Zhang JH, Tang W, Zhang ZX, et al. Connection of the Posterior Occipital Muscle and Dura Mater of the Siamese Crocodile. Anat Rec (Hoboken) 2016;299:1402-8. [Crossref] [PubMed]
- Zhang JF, Du ML, Sui HJ, et al. Investigation of the ischioanal fossa: Application to abscess spread. Clin Anat 2017;30:1029-33. [Crossref] [PubMed]
- Chen WPD. Techniques, Principles and Benchmarks in Asian Blepharoplasty. Plast Reconstr Surg Glob Open 2019;7:e2271. [Crossref] [PubMed]
- May JW Jr, Fearon J, Zingarelli P. Retro-orbicularis oculus fat (ROOF) resection in aesthetic blepharoplasty: a 6-year study in 63 patients. Plast Reconstr Surg 1990;86:682-9. [Crossref] [PubMed]
- Singh DP, Forte AJ, Apostolides JG, et al. The sentinel fat pads: the relationship of the ROOF and SOOF to the temporal nerve in facial rejuvenation. Aesthet Surg J 2011;31:11-20. [Crossref] [PubMed]
- Tower J, Seifert K, Paskhover B. Longitudinal Analysis of Superficial Midfacial Fat Volumes Over a 10-Year Period. Aesthetic Plast Surg 2018;42:995-1001. [Crossref] [PubMed]
- Hwang K, Yoo SK, Kim DJ. Location of the Septoaponeurosis Junction Relative to the Tarsal Plate in Upper Eyelids. J Craniofac Surg 2018;29:1051-3. [Crossref] [PubMed]
- Wang X, Wang H. Anatomical Study and Clinical Observation of Retro-orbicularis Oculi Fat (ROOF). Aesthetic Plast Surg 2020;44:89-92. [Crossref] [PubMed]
- Iwanami M, Tsurukiri K. Histological comparison between young and aged specimens of the Oriental lower eyelid using sagittal serial sections. Plast Reconstr Surg 2007;119:2061-71. [Crossref] [PubMed]
- Lim WK, Rajendran K, Choo CT. Microscopic anatomy of the lower eyelid in asians. Ophthalmic Plast Reconstr Surg 2004;20:207-11. [Crossref] [PubMed]
- Kim HS, Hwang K, Kim CK, et al. Double-eyelid surgery using septoaponeurosis junctional thickening results in dynamic fold in asians. Plast Reconstr Surg Glob Open 2013;1:1-9. [Crossref] [PubMed]
- Kakizaki H, Leibovitch I, Selva D, et al. Orbital septum attachment on the levator aponeurosis in Asians: in vivo and cadaver study. Ophthalmology 2009;116:2031-5. [Crossref] [PubMed]
- Chen WPD. Aesthetic eyelid surgery in Asians: an east-west view. Hong Kong J Ophthalmol 2000;3:27.


