
Traditional Chinese medicine classification of knee osteoarthritis with proteomics analysis
Introduction
Osteoarthritis (OA) is a heterogeneous disease caused by the pathological changes of the synovial joint. About 10–12% of adults suffer from symptomatic OA (1,2). Therefore, it affects many individuals and throws a heavy burden on the medical system. OA is included in the category of “Bone Bi” in traditional Chinese medicine (TCM). The pathogenesis is complicated, the disease evolves rapidly, and multiple pathologies are interchangeable. Due to the inconsistent understanding of Bone Bi syndrome’s pathogenesis, there is a significant difference in the differentiation of syndromes among different medicines. In recent years, scholars have begun to study the essence of “syndrome” from the perspective of genes and proteomics (3). Proteomics theory has gradually been used to diagnose, treat, and research various diseases and syndromes in Chinese medicine (3-8). The substantial material basis research of “syndrome” with proteomics as the starting point has highlighted its advantages in modernizing TCM (9).
Synovial fluid (SF) is the capillary exudate present in the joint chamber. Proteins in SF also comes from surrounding tissues, articular cartilage, synovium, and bone (10). SF directly contacts the affected tissues, cartilage, synovial tissue, and bones, which will become a source of high-quality biomarkers (11). In earlier studies, many substances have been found in synovial fluid, including cytokines, chemokines (12), molecules (13), and proteins (14). SF analysis is a crucial way to understand OA (15). The quantitative proteomics method of isobaric tags for relative and absolute quantitation iTRAQ was initially reported by Ross et al. (16). This method can identify and quantify proteins from many samples simultaneously while retaining the critical posttranslational modification information. This study used iTRAQ technology to compare the protein in the synovial fluid between patients with knee OA and knee traumatic synovitis to obtain the relative and absolute content of histones in different joint synovial fluids, hoping to find the difference of protein expression. We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2117).
Methods
Study population
From January 1, 2011, to January 31, 2013, according to the OA diagnostic criteria established by the American Academy of Rheumatology and the TCM syndrome criteria of Zhonggu Bi in the Chinese Medicine Industry of the People’s Republic of China, “Diagnosis and Curative Effect Standards of TCM Diseases and Syndromes” (94 edition), patients aged 40–65 years old with knee OA stage I–II (according to Kellgren-Lawrence Staging) were enrolled. Knee OA with different TCM Classification of each patient was confirmed by a specialist team (consisting of 2 professors and 2 chief doctors) according to criteria mentioned previously. At the final analysis, 15 patients have enrolled: 5 patients with kidney deficiency, 5 patients with Yang deficiency, 5 patients with blood stasis. Another 5 patients with synovitis were enrolled as the control group. All subjects were excluded from diseases, including severe liver and kidney function, hematopoietic system disorders, hypertension, cardiopulmonary dysfunction, tumors, tuberculosis, infectious diseases, and acute severe injuries. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of The First Affiliated Hospital of Guizhou University of Traditional Chinese Medicine. All subjects were informed and signed an informed consent form before oral treatment with Chinese medicine and joint fluid acquisition.
Classification and medication
Synovial fluid samples were divided into three groups according to the patient diagnosis of TCM: kidney deficiency group, Yang deficiency group, and blood stasis group. Patients of the kidney deficiency group were given the treatment of nourishing yin and nourishing the kidney, and choosing Liuwei Dihuang Decoction (prepared Rehmannia 15 g, dogwood 12 g, yam 12 g, dan bark 10 g, Alisma 10 g, Poria cocos 10 g); patients of Yang deficiency type were given Wenyang therapy to dispel cold and nourish the kidney and replenish Qi (the prescription uses Jinkuishenqi Decoction: 10 g Guizhi, 6 g Aconite, Rehmannia 15 g, Cornus 15 g, Chinese Yam 15 g, Poria 15 g, Dan Bark 10 g, Alisma 10 g); patients of blood stasis type were given blood circulation promotion therapy (the prescription is Taohong Siwu Decoction: Rehmannia root 15 g, angelica 15 g, white peony 10 g, chuanxiong 8 g, peach kernel 9 g, safflower 6 g). The above three prescriptions were administered to patients twice a day for two weeks.
Sample collection and processing
The synovial fluids of different types of OA of kidney deficiency, yang deficiency, and blood stasis before treatment were drawn into the Aa group, Ba group, and Ca group. The synovial fluids were acquired as described before (12). After two weeks of medication, the three joint fluid types were drawn again as the Ab group, Bb group, and Cb group, the untreated control group’s joint fluid, drawn as the D group. The amount of synovial fluid in 35 samples was about 2 to 4 mL. The samples were frozen and stored in a refrigerator at −80 °C. Use iTRAQ analysis to analyze the samples (Shanghai Shanghai Zhongke New Life Biotechnology Co. coordinates iTRAQ analysis, Ltd., China).
Statistical analysis
Using SPSS 20.0 statistical software for statistical processing. Quantitative data were expressed as mean ± standard deviation, and the F test performed a comparison between groups. P<0.05 indicates that the difference is statistically significant.
Results
After 2 weeks of medication, all patients reported no significant suspected side effects. Repeated blood tests revealed no significant liver injury or renal injury.
Quantitative determination results
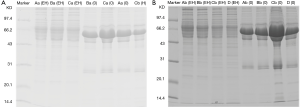
See Table 1 for the quantitative results of protein analyzed by iTRAQ. The comparison showed statistical differences between each group at different time points (P<0.05). The protein electrophoresis has similar results (Figure 1).
Full table
Quantitative comparative analysis
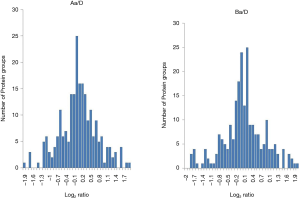
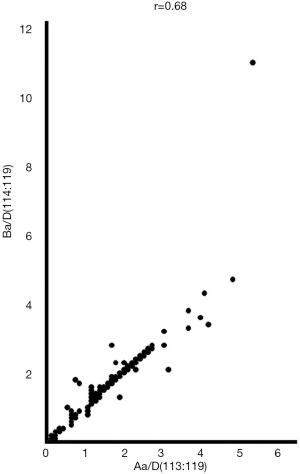
We used a frequency distribution histogram to analyze iTRAQ quantitative data. The ratio of each group of labels to the reference label is Log2 logarithm, the group distance is set to 0.1, and the distribution range is −2.0 to 2.0. Excel draws Figure 2. Figure 2Aa/D and 2Ba/D are typically distributed and similar, and the ratio between the two sets of samples and the reference (2Aa/D and 2Ba/D) is used for Pearson correlation analysis, as shown in the scatter diagram 3. The points in the figure are close to a straight line, suggesting that there is a correlation.
Significantly different proteins
The total number of protein groups identified in the experiment is 251, and all seven channels have quantitative information, and the number of protein groups is 246. The seven samples were analyzed for Aa and D, Ba and D, Ca and D, Aa, and Ab, Ba, and Bb, Ca and Cb, and the significance index (P value) calculated. A total of 32 differential proteins were detected between the treatment group and the control group (P<0.01), as shown in Table S1. Compared with the control group, there were eight significant reductions in the treatment group: histone H4, histone H2A, S100 calcium-binding protein A8, fibrinogen γ, fibrinogen α, cDNA (FLJ92148), C4b binding protein, part of transketolase variants; one significantly increased: basement membrane glycan. Among these differentially expressed proteins, fibrinogen γ and C4b binding protein were still significantly reduced compared with the control group after treatment. Two proteins were significantly reduced in the Aa group than the control group and the Ab group: HIST1H2BC and myeloperoxidase. Compared with the control group and the Bb group, the Ba group also had two significantly reduced proteins: serum amyloid P protein and apolipoprotein C-I variants. Compared with the control group and the Cb group, the Ca group had three proteins significantly reduced: histone H2A, C-reactive protein, and fibrinogen α. Compared with the control group, lactoferrin and prefibrin-1 were significantly decreased in the Aa and Ba groups, and hemoglobin α1 was significantly increased.
Discussion
The iTRAQ technology uses 4 or 8 isotopic labels to label the amino groups of polypeptides specifically and then performs tandem mass spectrometry analysis to compare the relative or absolute content of proteins in 4 or 8 different samples simultaneously. Many scholars have used it to find the differentially expressed proteins of some diseases (17-21). In this experiment, we used iTRAQ technology to investigate OA patients and found 32 proteins with significant differences.
Analysis of the difference between OA and traumatic synovitis proteome
Eight (histone H4, histone H2A, S100 calcium-binding protein A8, fibrinogen γ, fibrinogen α, cDNA (FLJ92148), C4b binding protein, partial transketone) significantly decreased and a significantly increased protein (basement membrane glycan) OA patients compared with patients with traumatic synovitis. Among these proteins, fibrinogen gamma and C4b binding protein were still significantly reduced after treatment, suggesting that OA patients’ systemic symptoms are negatively related to fibrinogen gamma and C4b binding protein in synovial fluid.
Correlation between kidney deficiency and marrow deficiency and yang deficiency and cold coagulation
This study found that lactoferrin and prefibrin-1 were significantly reduced in the Aa and Ba groups compared with the control group hemoglobin α1 was significantly increased. According to Figures 2 and 3, the two groups A and B, have a positive correlation. Both lactoferrin and prefibrin-1 have a specific effect on the structure of bone cells. TCM believes that kidney yin deficiency mainly causes kidney deficiency, while kidney yang deficiency mainly causes yang deficiency, and both are dysfunction of the kidney, and there is a view that yang damages yin and yin damages yang. The two types have common points in symptoms and genes (22). In the treatment of OA, both kidney yin and kidney yang can be cured. Therefore, although both kidney and yang deficiency can find their different proteins, there is a clear correlation between these two types.
Differential proteins of three types of OA in kidney deficiency and marrow deficiency, yang deficiency, and cold coagulation, and blood stasis block
HIST1H2BC and myeloperoxidase were significantly reduced in the Aa group compared with the control group and the Ab group, suggesting that the two are characteristical proteins of kidney deficiency type OA. Serum amyloid P protein and apolipoprotein C-I variants were significantly reduced in the Ba group compared with the control group and the Bb group, suggesting that the two may be the characteristics of the Yang deficiency type OA. At present, many scholars have found the differentially expressed proteins of kidney-yin deficiency and kidney yang deficiency, but there are no reports of differences in HIST1H2BC, myeloperoxidase, serum amyloid P protein, and apolipoprotein CI variants. Histone H2A, C-reactive protein, and fibrinogen α were significantly reduced in the Ca group compared with the control group and the Cb group, suggesting that the three may be characteristically proteins of blood stasis type OA. Studies have shown that fibrinogen is a differential protein of coronary heart disease with blood stasis syndrome (23), and the relationship between histone H2A, C-reactive protein, and blood stasis syndrome has not been studied.
In general, through the analysis of this study, it is concluded that the synovial fluid in OA with kidney deficiency, Yang deficiency n has a significant protein correlation, which further confirms that kidney yang deficiency is related to kidney yin deficiency, which is supportive for further research on the theory of kidney deficiency syndrome. It is also concluded histone H4, histone H2A, S100 calcium-binding protein A8, fibrinogen γ, fibrinogen α, cDNA (FLJ92148), C4b binding protein, and partial transketol and basement membrane glycan may be used as markers to identify OA. HIST1H2BC and myeloperoxidase may be differential proteins that distinguish kidney-deficiency OA from the other two types. Serum amyloid P protein and apolipoprotein CI variants may be differential proteins of yang deficiency. Histone H2A, C-reactive protein, and fibrinogen α may be differential proteins of blood stasis type. The protein differences between the three types of OA syndromes of different TCM types provide a material basis for TCM clinical types and provide theoretical support for the subsequent treatment stage.
However, there are still many limitations to this study. Since some patients have no synovitis changes or, there is very little synovial fluid. It is not easy to get for the test. Secondly, the sample size is small, which decreases the credibility of this study. Future studies should enroll more patients to confirm our findings.
Acknowledgments
Funding: This study was supported by The National Natural Science Fund of China (No.81860855) and the Funding for scientific research on traditional Chinese medicine and Ethnomedicine of Guizhou provincial Administration of traditional Chinese Medicine (No.QZYY2010-19).
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2117
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2117
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2117). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of The First Affiliated Hospital of Guizhou University of Traditional Chinese Medicine. All subjects were informed and signed an informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Centers for Disease Control and Prevention (CDC). Prevalence and impact of chronic joint symptoms--seven states, 1996. MMWR Morb Mortal Wkly Rep 1998;47:345-51. [PubMed]
- Dunlop DD, Manheim LM, Song J, et al. Arthritis prevalence and activity limitations in older adults. Arthritis Rheum 2001;44:212-21. [Crossref] [PubMed]
- Heinegård D, Saxne T. The role of the cartilage matrix in osteoarthritis. Nat Rev Rheumatol 2011;7:50-6. [Crossref] [PubMed]
- Yu ZY, Du J. Proteomics and the qualitative research of traditional Chinese medicine. Chinese Journal of Integrated Traditional Chinese and Western Medicine 2004;24:844-6.
- Liu JR, Fan YG, Wang HB, et al. Bone Proteomic Analysis About Chinese Medicine Action on Rat Glucocorticoid - induced Model of Osteonecrsis. Chinese Journal of Orthopedics and Traumatology 2005;13:4-10.
- Liu WM, Yao NL, Wu ZK, et al. Research on TCM Syndrome and Syndrome Proteomics. Chinese Journal of Traditional Chinese Medicine 2003;31:1.
- Gao Y, Lu QJ, Liu YX, et al. Research on the material basis of Chinese herbal compound prescriptions. Chinese Journal of New Drugs 2000;9:307-8.
- Huang LM, Liang H. Proteomic Considerations and Methods of Different Diseases with Same Syndrome of Kidney-Yang Deficiency. Shanghai Journal of Traditional Chinese Medicine 2005;39:44-8.
- Hu XJ, Cai GX, Liu BY, et al. Application of proteomics in study of syndrome essence in TCM. Chinese Journal of Traditional Chinese Medicine 2008;23:87-91.
- Ruiz-Romero C, Calamia V, Carreira V, et al. Strategies to optimize two-dimensional gel electrophoresis analysis of the human joint proteome. Talanta 2010;80:1552-60. [Crossref] [PubMed]
- Ruiz-Romero C, Blanco FJ. Proteomics role in the search for improved diagnosis, prognosis and treatment of osteoarthritis. Osteoarthritis Cartilage 2010;18:500-9. [Crossref] [PubMed]
- Hampel U, Sesselmann S, Iserovich P, S, et al. Chemokine and cytokine levels in osteoarthritis and rheumatoid arthritis synovial fluid. J Immunol Methods 2013;396:134-9. [Crossref] [PubMed]
- Bertrand J, Cromme C, Umlauf D, et al. Molecular mechanisms of cartilage remodelling in osteoarthritis. Int J Biochem Cell Biol 2010;42:1594-601. [Crossref] [PubMed]
- Mateos J, Lourido L, Fernández-Puente P, et al. Differential protein profiling of synovial fluid from rheumatoid arthritis and osteoarthritis patients using LC-MALDI TOF/TOF. J Proteomics 2012;75:2869-78. [Crossref] [PubMed]
- Bouloux GF. The Use of Synovial Fluid Analysis for Diagnosis of Temporomandibular Joint Disorders. Oral Maxillofac Surg Clin North Am 2018;30:251-6. [Crossref] [PubMed]
- Ross PL, Huang YN, Marchese JN, et al. Multiplexed protein quantitation in Saccharomyces cerevisiae using amine-reactive isobaric tagging reagents. Mol Cell Proteomics 2004;3:1154-69. [Crossref] [PubMed]
- Culnan DM, Cooney RN, Stanley B, et al. Apolipoprotein A-IV, a putative satiety/antiatherogenic factor, rises after gastric bypass. Obesity (Silver Spring) 2009;17:46-52. [Crossref] [PubMed]
- Hardt M, Witkowska HE, Webb S, et al. Assessing the effects of diurnal variation on the composition of human parotid saliva: quantitative analysis of native peptides using iTRAQ reagents. Anal Chem 2005;77:4947-54. [Crossref] [PubMed]
- Ogata Y, Charlesworth MC, Higgins L, et al. Differential protein expression in male and female human lumbar cerebrospinal fluid using iTRAQ reagents after abundant protein depletion. Proteomics 2007;7:3726-34. [Crossref] [PubMed]
- Tewfik MA, Latterich M, DiFalco MR, et al. Proteomics of nasal mucus in chronic rhinosinusitis. Am J Rhinol 2007;21:680-5. [Crossref] [PubMed]
- DeSouza L, Diehl G, Rodrigues MJ, et al. Search for cancer markers from endometrial tissues using differentially labeled tags iTRAQ and cICAT with multidimensional liquid chromatography and tandem mass spectrometry. J Proteome Res 2005;4:377-86. [Crossref] [PubMed]
- Wei M, Zhao XS, Sun XM, et al. Comparative study on gene expression of kidney-Yin deficiency and kidney-Yang deficiency. Journal of Shanxi Medical University 2012;43:652-4.
- Wu HJ, Ma ZC, Gao Y, et al. Study on GAP in Blood - stasis Type of Coronary Heart Disease by Using Proteomic Technique. Journal of Integrated Traditional Chinese and Western Medicine Cardio-Cerebrovascular Disease 2005;3:189-91.
(English Language Editor: J. Chapnick)


