
Differences between conventional wound closure and a closed suction irrigation method for the prevention of surgical site infection—a comparative study
Introduction
Wound infections are the most common healthcare-associated infections in surgical patients and cause postoperative morbidity (1,2). Therefore, prevention of wound infection is of paramount importance.
Conventionally, the abdominal wound was sutured sequentially after irrigated with normal saline. Herein we proposed a new strategy of wound closure called the closed suction irrigation method. It has previously been reported that closed suction irrigation is also used in the treatment of postoperative spinal infection (3), but the drainage tube operation is different from that for abdominal wounds in this study.Herein, the drainage tube is run through the whole incision, with the middle segment in the tissue and both ends in vitro, which is not easy to block. By eliminating any exudates and irritants collected in the wound, the method focuses on applying saline irrigation combined with sub-atmospheric pressure in the subcutaneous layer. Furthermore, our present method promotes wound healing by gradually obliterating the dead space, which could expedite angiogenesis, decrease the rate of wound infection, and diminish tissue edema.
In this retrospective study, we compared the closed suction irrigation method with conventional primary wound closure on the incidence of postoperative wound infections.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2154).
Methods
Our present retrospective study examined how open abdominal wounds influence the rate of wound infections. All enrolled patients were registered in our hospital from January 2009 to July 2019 and referred by tertiary hospitals. Patients who were treated by the closed suction irrigation method were classified into the study group. Patients treated by the conventional primary wound closure method were classified into the control group. All patients received equal systemic antibiotic treatment to fight against anaerobes and aerobes during the entire period of the operation. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of First People’s Hospital of Foshan and individual consent for this retrospective analysis was waived.
Conventional method (control group)
The wound was irrigated with one liter of normal saline, and the skin and fascia sutured separately by general surgeons.
Closed suction irrigation method (study group)
One liter of typical saline was used to irrigate the wound. The skin and the fascia were carefully sutured independently. A Fr 12–16 sized tube with 5 mm side ports at 1–2 cm apart was implanted into the subcutaneous cavity. Two separate tab injuries were made near the main wound (Figure 1). Typical saline was applied to irrigate the injury’s subcutaneous cavity through the two-ended tubes at a speed of 50 microdrops per minute. With one end of the tube interfaced, the other end was connected to an adjustable vacuum pump with a container to collect the irrigant and the wound exudate. A constant negative suction force of 100–150 mmHg was applied. The skin dressings were changed when necessary. After three days, saline irrigation was halted, and the tube was removed.
Statistical analysis
All data were collected and analyzed. Continuous variables were presented as mean ± median (range) or mean ± standard deviation (SD) and compared using the Mann-Whitney U test. Categorical variables were compared using the χ2 test or the Fisher exact test. Results were considered statistically significant when the P value was below 0.05.
Results
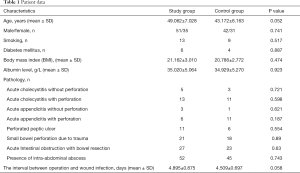
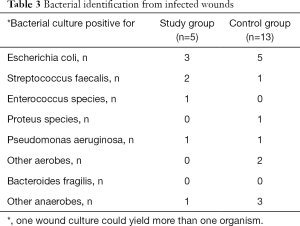
There were 86 and 73 patients enrolled in the study group and the control group in our present study, respectively. The patients’ characteristics are presented in Table 1. The total length of hospital stay and time is taken for the wound to heal completely was shorter in the study group compared to the control group (Table 2, 8.046±2.110 vs. 8.983±2.887 days and 8.092±3.258 vs. 10.328±6.074 days, respectively). Wound infection, which was defined by the type of the discharge from positively cultured wounds, was also significantly lower in the study group compared to the control group (Table 2). The time interval between the operation and detection of infection was 4.895±0.875 days for the study group and 4.509±0.697 days for the control group (Table 2, P=0.058). In case of redness, swelling, pain or purulent secretions, microbiological testing was performed. Bacteria were cultured from the infected wounds at the diagnosis time to identify the different bacterial infections types and are shown in Table 3. There was no abdominal wound dehiscence in either group of patients. After a median follow-up time of 2.5 months (range of 2–3 months), no incisional hernia or re-infection was detected. no sepsis occurred in any of the cases.
Full table

Full table
Full table
Discussion
Vacuum-assisted closure (VAC) is an advanced and widely used technique for managing difficult acute and chronic wounds. VAC is also well known as sealed surface wound suction (SSS), sub-atmospheric pressure (SAP), vacuum sealing technique (VST), topical negative pressure (TNP), and more (4). A VAC system involves placing a foam dressing directly onto the wound, which is then covered by a film that seals the wound and dressing. Drainage tubes under the dressing are connected to a pump to apply sub-atmospheric pressure to the wound. Although some scientific data regarding the rate of wound healing has been reported in open medical literature databases, there is a relatively limited number of randomized controlled trials to validate these current findings (5-8). Cohort studies have demonstrated that VAC decreased the infection rate for high-risk wounds compared to primary closure of wounds (9,10). Our closed suction irrigation system is an alteration of the VAC method and was used to reduce postoperative wound infection rates in high-risk patients. Unlike the VAC method, there was no requirement for a unique foam dressing. The viability of this closed suction irrigation technique in diminishing injury diseases has not been previously tested.
Postoperative wound infection rates are dependent on various patient and surgical factors. One crucial factor is the contamination of the wounds by high concentrations of microorganisms (11,12). Furthermore, restricted delicate tissue edema packs the vascular and lymphatic frameworks inside the injury. It has been suggested that the shut attractions water system technique reduces bacterial counts, removes any excessive fluid collecting in wounds, restores normal vascular and lymphatic flow, as well as mechanically triggers angiogenesis, neovascularization, and immunomodulation, consequently expediting recovery from injury.
From our studies, the closed suction irrigation strategy is a promising method to decrease wound disease. Currently in our hospital, besides abdominal wounds, it is also used for surgery on limbs and chest wall. It can shorten hospitalization and improve recovery time. Further investigations and randomized controlled trials are essential to characterize the closed suction irrigation technique’s efficacy at decreasing postoperative injury disease. In addition, whether it is possible to further reduce the infection rate of incisions by changing the flushing fluid of closed suction irrigation, such as adding aeriodine and other liquid flushing, remains to be further studied.
Acknowledgments
Funding: The study was supported by Science and Technology Project of Guangdong Province (2014A020209003), and sponsored by Shanghai Tongshu Biotechnology Co., Ltd.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2154
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2154
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2154). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of First People’s Hospital of Foshan and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bratzler DW, Hunt DR. The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 2006;43:322-30. [Crossref] [PubMed]
- Broex EC, van Asselt AD, Bruggeman CA, et al. Surgical site infections: how high are the costs?. J Hosp Infect 2009;72:193-201. [Crossref] [PubMed]
- Rohmiller MT, Akbarnia BA, Raiszadeh K, et al. Closed suction irrigation for the treatment of postoperative wound infections following posterior spinal fusion and instrumentation. Spine (Phila Pa 1976) 2010;35:642-6. [Crossref] [PubMed]
- Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg 2005;29:219-26. [Crossref] [PubMed]
- Mouës CM, Vos MC, van den Bemd GJ, et al. Bacterial load in relation to vacuum-assisted closure wound therapy: a prospective randomized trial. Wound Repair Regen 2004;12:11-7. [Crossref] [PubMed]
- Braakenburg A, Obdeijn MC, Feitz R, et al. The clinical efficacy and cost effectiveness of the vacuum-assisted closure technique in the management of acute and chronic wounds: a randomized controlled trial. Plast Reconstr Surg 2006;118:390-7; discussion 398-400. [Crossref] [PubMed]
- Plikaitis CM, Molnar JA. Subatmospheric pressure wound therapy and the vacuum-assisted closure device: basic science and current clinical successes. Expert Rev Med Devices 2006;3:175-84. [Crossref] [PubMed]
- Vuerstaek JD, Vainas T, Wuite J, et al. State-of-the-art treatment of chronic leg ulcers: A randomized controlled trial comparing vacuum-assisted closure (V.A.C.) with modern wound dressings. J Vasc Surg 2006;44:1029-37; discussion 1038. [Crossref] [PubMed]
- Machen S. Management of traumatic war wounds using vacuum-assisted closure dressings in an austere environment. US Army Med Dep J 2007.17-23. [PubMed]
- Leininger BE, Rasmussen TE, Smith DL, et al. Experience with wound VAC and delayed primary closure of contaminated soft tissue injuries in Iraq. J Trauma 2006;61:1207-11. [Crossref] [PubMed]
- Nikfarjam M, Kimchi ET, Gusani NJ, et al. Reduction of surgical site infections by use of pulsatile lavage irrigation after prolonged intra-abdominal surgical procedures. Am J Surg 2009;198:381-6. [Crossref] [PubMed]
- Granick MS, Tenenhaus M, Knox KR, et al. Comparison of wound irrigation and tangential hydrodissection in bacterial clearance of contaminated wounds: results of a randomized, controlled clinical study. Ostomy Wound Manage 2007;53:64-6, 68-70, 72. [PubMed]
(English Language Editors: J. Teoh and J. Chapnick)



