
Plasma cell leukemia characterized by EDTA-dependent plasma cell agglutination: a case report
Introduction
Primary plasma cell leukemia (PPCL) is one of the most challenging diseases for hematologists. PPCL is an uncommon form of plasma cell dyscrasia, and the most aggressive form of monoclonal gammopathies in humans (1,2). PPCL is characterized by the presence of >20% circulating plasma cells in the peripheral blood (1). Peripheral blood flow cytometry is an important tool to identify the presence of plasma cells and to exclude other lymphoproliferative disorders (2). EDTA-K2 induced white blood cells agglutination is a rare phenomenon in vitro. It is the first case reporting EDTA-dependent plasma cells agglutination in China. Herein, we reported a case of PPCL which was characterized by the EDTA-dependent plasma cell aggregation. We present the following case in accordance with the CARE Reporting Checklist.
Case presentation
A 65-year-old Chinese male with a history of chronic kidney disease was admitted to the Department of Nephrology due to the complaint of vomiting and nausea for two months. He lived alone and could perform daily activities independently with a good performance status. On admission, the vital signs were normal. Physical examination was unremarkable except for anemic appearance.
Laboratory examinations showed the hemoglobin (Hb) was 77.00 g/L, hematocrit was 22.2%, red blood cell (RBC) count was 2.38×1012/L, white blood cell (WBC) count was 12.3×109/L and platelet count was 158×109/L; the proportions of lymphocytes, monocytes and neutrophils were 40.9%, 21.2% and 37.14%, respectively; the serum creatinine was 787 µmol/L, cystatin C was 2.90 mg/L, total serum protein was 63.52 g/L, urea nitrogen was 30.8 mmol/L, uric acid was 815 µmol/L, total cholesterol was 7.70 mmol/L, triglyceride was 3.70 mmol/L, activated partial thromboplastin time was 41.90 s, thrombin time was >120 s, fibrinogen was 10.0 µg/mL and D-dimer was 2.6 µg/mL; homocysteine was 33.57 µmol/L. His serum bilirubin and liver enzymes were within normal ranges. Urine examination showed urine protein was 2+, the serological tests for human immunodeficiency virus, hepatitis B and C viruses, and human herpes viruses 6 and 8 showed negative. Immunophenotypic analysis of peripheral blood revealed the cluster of CD38+ cells, which was considered as the source of plasma cells. After admission, gastrointestinal bleeding and coagulant function was abnormal, appeared hemorrhagic shock, hemorrhagic shock threaten life, stomach, endoscopic check had no obvious bleeder, the patient was administered with repeated infusion of fresh plasma and suspended red blood cells due to the aggravating anemia and blood coagulation disorder. The patient received treatment for hemostasis, protecting gastric, inhibit gastric acid and transfusion. Hemodialysis was also recommended. In spite of systemic treatment, the patient died on January 10, 2018. According to the above findings, he was diagnosed with PPCL. The case report was approved by the Ethics Committee of the Second People’s Hospital of QuJing City in YunNan and written informed consent was obtained from the patient.
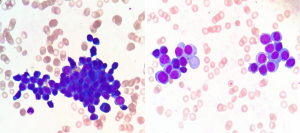
The peripheral blood smearing showed cloud-like piles of plasma cells (Figure 1).
Discussion
According to the recommendations of the International Council for Standardization in Hematology (ICSH), EDTA is widely used as an anticoagulant for routine hematologic testing in the laboratory medicine. The ethylenediaminetetraacetic acid dependent PTCP (EDTA-PTCP) is the most frequent cause of Pseudothrombocytopenia (3), which is usually caused by EDTA-dependent antiplatelet antibodies that can recognize the cytoadhesive receptors gp IIb-IIIa (4). The calcium-chelating effect of EDTA results in aggregation of platelets in vitro and EDTA may cause the dissociation of Ca2+-dependent gp IIb-IIIa heterodimer (5). This interaction stimulates the expression of activated antigens, and triggers the activation of tyrosine kinases which finally leads to a spurious reduction in the platelet count measured by an automated hematology analyzer (6). In our report, this was a rare case that EDTA-K2 the induced the aggregation of peripheral blood plasma cells, which has never been reported.
As for the limitation of this study, due to the rapid progress of this case, the patient died without further examination of the bone marrow.
The exact mechanisms of EDTA-dependent peripheral blood plasma cell agglutination are not clear. This phenomenon may be related to the elevated production of abnormal proteins in some diseases, such as malignant tumors, infections, liver diseases and auto-immune diseases. We hope this report may provide experimental evidence on the early clinical diagnosis of PTCP.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-19-424). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chng WJ, Dispenzieri A, Chim CS, et al. IMWG consensus on risk stratification in multiple myeloma. Leukemia 2014;28:269-77. [Crossref] [PubMed]
- Jelinek T, Kryukov F, Rihova L, et al. Plasma cell leukemia: from biology to treatment. Eur J Haematol 2015;95:16-26. [Crossref] [PubMed]
- Salignac S, Latger-Cannard V, Schlegel N, et al. Platelet counting. Methods Mol Biol 2013;992:193-205. [Crossref] [PubMed]
- Casonato A, Bertomoro A, Pontara E, et al. EDTA dependent pseudothrombocytopenia caused by antibodies against the cytoadhesive receptor of platelet gpIIB-IIIA. J Clin Pathol 1994;47:625-30. [Crossref] [PubMed]
- Chae H, Kim M, Lim J, et al. Novel method to dissociate platelet clumps in EDTA-dependent pseudothrombocytopenia based on the pathophysiological mechanism. Clin Chem Lab Med 2012;50:1387-91. [Crossref] [PubMed]
- Lippi G, Plebani M. EDTA-dependent pseudothrombocytopenia: further insights and recommendations for prevention of a clinically threatening artifact. Clin Chem Lab Med 2012;50:1281-5. [Crossref] [PubMed]


