
Barriers to inpatient palliative care consultation among patients with newly diagnosed cancer after emergency admission
Introduction
It is not uncommon to diagnose new cancer cases following emergency presentation. In fact, 20–25% of all cancer types in the UK are diagnosed after emergency presentation (1,2). These cases are more likely to have advanced disease status and poor prognosis (3). Previous studies have showed that survival time was significantly shorter after emergency presentation than after any other diagnostic route (1,3,4). Several factors, including access to transportation, lack of a regular primary care provider or a medical home, and personal experience and knowledge were reported as key factors contributing to late diagnosis and delay in seeking medical help (5,6).
It was reported that late presentation of these patients was associated with poor experience and poorly coordinated care (2). Patients with newly diagnosed cancer following emergency presentation often experience delayed referral for oncology and palliative care (PC) services (2). According to a qualitative study, patients diagnosed with cancer following emergency admission (EA) demonstrated a desire to gain knowledge and additional information regarding the respective diagnostic tests and about the type of cancer they had (7). Moreover, this study reported that family/informal caregivers had insufficient information required to facilitate care for patients at home and inadequate care was provided by health and social care services (7). These results can help explain the presence of newly diagnosed cancer patients with unmet PC needs. A randomized clinical trial suggested that early referral for PC consultation from the emergency department (ED) improved quality of life in patients with advanced cancer (8). Patients with newly diagnosed cancer following emergency presentation would benefit from ED-initiated PC consultation.
To the best of our knowledge, few studies have investigated and reported the factors influencing the referral of patients with newly diagnosed cancer following emergency presentation for PC consultation. This study assesses potential patient-related barriers to inpatient PC consultation among patients who were newly diagnosed with cancer after EA and received only supportive care. We present the following article in accordance with the STROBE Reporting Checklist (available at http://dx.doi.org/10.21037/apm-19-504).
Methods
Study design and patients
A single-center, retrospective, observational study was conducted at Tsukuba Medical Center Hospital, Tsukuba, Japan. This hospital is not only an acute care community hospital but also a designated cancer care hospital. The hospital has 453 beds, along with a department of emergency medicine and a PC center with a PC unit (20 beds) and PC team (PCT). The PCT consists of a PC specialist, a PC certified nurse, a pharmacist, and a medical social worker.
This study enrolled patients who were emergently admitted to the hospital between January 2012 and November 2016. First, we analyzed their post-hospitalization discharge summaries and identified patients who were listed as having cancer as the primary disease. Then, we used medical records to identify which of these patients were newly diagnosed with cancer either pathologically or clinically. Patients who were diagnosed with cancer in the past or following discharge from the hospital were excluded. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by ethics board of Tsukuba Medical Center Hospital (No. 2018–009). Because of the retrospective nature of the research, the requirement for informed consent was waived.
Measurements
Medical record information on the patients’ predominant symptoms, primary tumors, metastasis status, anticancer treatments, length of stay, and referral for inpatient PC consultation were collected. Anticancer treatments included radical surgery, palliative surgery, chemotherapy or radiotherapy, transfer to another hospital for anticancer treatment, and supportive care only. Similar to a prior study (7), supportive care was defined as care provided when specific anticancer treatment was either inappropriate or not currently indicated. Among the patients who received only supportive care, this study evaluated their clinical outcomes, survival time after EA, and disclosure of cancer diagnosis. The PCT intervened after patients were referred for inpatient PC consultation by an attending physician.
Statistical analysis
Patients who received only supportive care were separated into two groups based on whether or not they were referred for PC consultation. Quantitative variables were divided into groups for analysis. Differences in categorical variables between the two patient groups were tested using Pearson’s chi-squared test. Patients with missing data were excluded from the analysis. All analyses were conducted using STATA version 14.0 (Stata Corp., College Station, TX, USA).
Results
A total of 11,827 emergency cases were transferred to the hospital during the study duration; of the total, 473 had cancer listed as the primary disease in the post-hospitalization discharge summary. The final study group included 141 patients with newly diagnosed cancer, accounting for 1.2% of all emergency transfer cases.
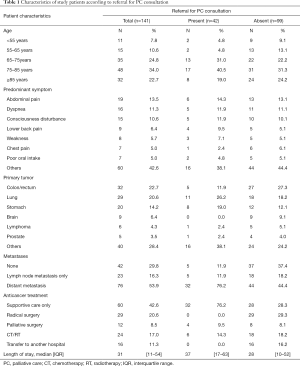
The predominant symptoms of patients in the study were abdominal pain (n=19), dyspnea (n=16), and disturbance of consciousness (n=15), and the locations of the primary lesions were colon or rectum (n=32), lung (n=29), and stomach (n=20) (Table 1). The prevalence of newly diagnosed cancer patients with metastasis was 70.2% (16.3% for lymph node metastasis only and 53.9% for distant metastasis) (Table 1).
Full table
Table 1 shows patient characteristics according to whether patients were referred for inpatient PC consultation. The prevalence of referral for PC consultation was 29.8% for all patients (n=42). More number of patients with distant metastasis were referred for PC consultation than patients without distant metastasis. With respect to anticancer treatment, 20.6% (n=29) of the patients enrolled in the study underwent radical surgery and none of them were referred for PC consultation during their hospital stay. Alternatively, 42.6% (n=60) of the study patients received only supportive care. Fifty-three point three percent of them (n=32) were referred for PC consultation and 23.3% of them (n=14) were discharged alive from the hospital.
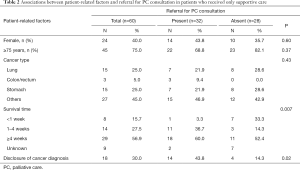
Finally, we investigated the associations between patient-related factors and referral for PC consultation in patients who received only supportive care (Table 2). When comparing patient groups with and without referral for PC consultation, the latter group was significantly more likely to have shorter survival time and less likely to receive disclosure of their cancer diagnosis (P=0.007 and 0.02, respectively). Sex, age, and cancer type were not significantly associated with referral for PC consultation.
Full table
Discussion
To the best of our knowledge, this is the first study to report the present status of referral for inpatient PC consultation among patients with newly diagnosed cancer after EA in Japan. Similar to previous studies, pain was the most common symptom in patients with newly diagnosed cancer after EA (9,10). Furthermore, 42.6% of patients with newly diagnosed cancer after EA received only supportive care. This result is consistent with the findings of previous studies (1,7) and suggests that diagnostic delay is relatively common in patients with newly diagnosed cancer after EA.
In this study, it is extremely important to identify potential barriers that prevent attending physicians from referring their patients for inpatient PC consultation. Our analysis of 60 patients who received only supportive care suggested that short survival time and no disclosure of diagnosis might have interfered with the referral for PC consultation. Previous studies have demonstrated that several factors, other than the aforementioned patient-related factors, reduced the likelihood of referral for PC consultation, such as limited knowledge regarding the role of the PCT (11), inadequate communication that prevented a shared understanding of patients’ needs and goals of care (12), ease of referral (13), lack of 24-hour availability of the PCT (14,15), and cultural differences (16). The present study suggests that facilitating the physicians’ ability to make referrals for PC consultation and improving their knowledge about the role of the PCT might result in successfully meeting the PC needs of patients with poor prognosis or no disclosure of diagnosis.
Moreover, 29.8% of all patients and 53.3% of those who received only supportive care were referred for inpatient PC consultation was a crucial finding. Previous studies have suggested that all patients diagnosed with lung cancer following EA should be routinely offered a specialist PC assessment because of the frequent combination of advanced disease, poor performance status and prognosis, and complex social contexts (6,7). It should be noted that approximately two-thirds of the patients with newly diagnosed cancer after EA and half of the patients who received only supportive care after EA in this study might have received insufficient PC.
Screening for PC consultation may be useful in helping patients and families with unmet PC needs. Screening criteria and tools have been developed for patients with advanced cancer and for those with PC needs in the ED (17). A systematic review of PC screening in the ED identified a variety of screening criteria used to identify ED patients who would benefit from PC resources and referral (17). Standardized screening criteria across varied ED settings may offer benefits to patients with newly diagnosed cancer after EA. Alternatively, it is necessary for the PCT to understand the attitudes and beliefs of the ED provider (18) and to collaborate with the ED providers more effectively to help patients and families with unmet PC needs.
The main limitation of this study is that it was carried out at a single institution. Therefore, our findings may not reflect the general population. Our hospital did not accept emergency patients with hematemesis or melena. This may have also led to an underestimation of the number of patients with gastrointestinal cancer. Furthermore, our hospital could not monitor patients with several types of cancer, including brain tumors and lymphoma, because these patients were transferred to another hospital for consultation with specialists after diagnosis. Moreover, this study recruited patients with newly diagnosed cancer after EA using their post-hospitalization discharge summaries. Hence, this methodology may not have been sufficient to screen these patients because of omission of cancer diagnosis. Finally, this study was limited to patients who were newly diagnosed with cancer during their hospital stay; thus, there might have been cases where patients were diagnosed with cancer at a later visit after discharge from the hospital. Although this study did not aim to clarify the exact number of patients with newly diagnosed cancer after EA, these facts might have slightly affected our results.
In conclusion, this study described short survival time and no disclosure of cancer diagnosis as potential barriers to inpatient PC consultation among patients with newly diagnosed cancer after EA. More effective collaboration with the physicians and the ED providers might be imperative for the PCT to meet the PC needs of the patients and families.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE Reporting Checklist. Available at http://dx.doi.org/10.21037/apm-19-504
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-19-504
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-19-504). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by ethics board of Tsukuba Medical Center Hospital (No. 2018–009). Because of the retrospective nature of the research, the requirement for informed consent was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Elliss-Brookes L, Mcphail S, Ives A, et al. Routes to Diagnosis for Cancer - Determining the Patient Journey Using Multiple Routine Data Sets. Br J Cancer 2012;107:1220-6. [Crossref] [PubMed]
- Young A, Marshall E, Krzyzanowska M, et al. Responding to acute care needs of patients with cancer: recent trends across continents. Oncologist 2016;21:301-7. [Crossref] [PubMed]
- Beckett P, Tata LJ, Hubbard RB. Risk factors and survival outcome for non-elective referral in non-small cell lung cancer patients--analysis based on the National Lung Cancer Audit. Lung Cancer 2014;83:396-400. [Crossref] [PubMed]
- Blackshaw GR, Stephens MR, Lewis WG, et al. Prognostic significance of acute presentation with emergency complications of gastric cancer. Gastric Cancer 2004;7:91-6. [Crossref] [PubMed]
- Ramondetta LM, Meyer LA, Schmeler KM, et al. Avoidable tragedies: Disparities in healthcare access among medically underserved women diagnosed with cervical cancer. Gynecol Oncol 2015;139:500-5. [Crossref] [PubMed]
- Caswell G, Seymour J, Crosby V, et al. Lung cancer diagnosed following an emergency admission: exploring patient and carer perspectives on delay in seeking help. Support Care Cancer 2017;25:2259-66. [Crossref] [PubMed]
- Wilcock A, Crosby V, Hussain A, et al. Lung cancer diagnosed following an emergency admission: Mixed methods study of the management, outcomes and needs and experiences of patients and carers. Respir Med 2016;114:38-45. [Crossref] [PubMed]
- Grudzen CR, Richardson LD, Johnson PN, et al. Emergency department-initiated palliative care in advanced cancer: A randomized clinical trial. JAMA Oncol 2016;2:591-8. [Crossref] [PubMed]
- Swenson KK, Rose MA, Ritz L, et al. Recognition and evaluation of oncology-related symptoms in the emergency department. Ann Emerg Med 1995;26:12-7. [Crossref] [PubMed]
- Brown MW, Bradley JA, Calman KC. Malignant disease in the accident and emergency department. Br J Clin Pract 1983;37:203-8. [PubMed]
- McDarby M, Carpenter BD. Barriers and Facilitators to Effective Inpatient Palliative Care Consultations: A Qualitative Analysis of Interviews With Palliative Care and Nonpalliative Care Providers. Am J Hosp Palliat Care 2019;36:191-9. [Crossref] [PubMed]
- Dudley N, Ritchie CS, Rehm RS, et al. Facilitators and barriers to interdisciplinary communication between providers in primary care and palliative care. J Palliat Med 2019;22:243-9. [Crossref] [PubMed]
- Le BH, Mileshkin L, Doan K, et al. Acceptability of early integration of palliative care in patients with incurable lung cancer. J Palliat Med 2014;17:553-8. [Crossref] [PubMed]
- Weiland TJ, Lane H, Jelinek GA, et al. Managing the advanced cancer patient in the Australian emergency department environment: findings from a national survey of emergency department clinicians. Int J Emerg Med 2015;8:14. [Crossref] [PubMed]
- Lamba S, Nagurka R, Zielinski A, et al. Palliative care provision in the emergency department: barriers reported by emergency physicians. J Palliat Med 2013;16:143-7. [Crossref] [PubMed]
- Enguidanos S, Housen P, Goldstein R, et al. Physician and nurse perceptions of a new inpatient palliative care consultation project: implications for education and training. J Palliat Med 2009;12:1137-42. [Crossref] [PubMed]
- George N, Phillips E, Zaurova M, et al. Palliative care screening and assessment in the emergency department: A systematic review. J Pain Symptom Manage 2016;51:108-19. [Crossref] [PubMed]
- Bruera E. The emergency department point of palliative care access for patients with advanced cancer. JAMA Oncol 2016;2:577-8. [Crossref] [PubMed]


