Gastrolithiasis with incomplete intestinal obstruction in the perioperative period of percutaneous transluminal coronary intervention: one case report
Introduction
Gastroliths refer to some kind of food or foreign body that can neither pass through the pylorus in time nor be digested, it stays in the stomach and gathers into a mass, or coagulates into a solid mass with gastric mucosa (1). Due to the different compositions of gastrolith, they can be mainly divided into the following categories: plant gastrolith, hair gastrolith, drug gastrolith, lactic acid gastrolith, etc., and plant gastrolith is the most common (2). The usual symptoms include abdominal discomfort after meal, fullness, dull pain, which can be accompanied by nausea, vomiting and halitosis, sometimes a gastrolith with large volume can cause heavy pressure in upper abdomen. The common complications include pyloric obstruction, gastric mucosal erosion, ulcer or bleeding, hypoxemia in a few people, gastric perforation happens occasionally, and acute intestinal obstruction may happen when gastrolith enters the small intestine (1).
The symptoms of gastrolith are similar to those of acute gastritis, so gastrolith is easy to be ignored, but its complications are serious. Therefore, early diagnosis and intervention are very important to avoid complications caused by gastrolith (3). This paper shows the entire process of a patient with a big gastrolith accompanied with incomplete intestinal obstruction just after PCI, and recovered after endoscopic removal with no adverse events while DAPT was given. It may provide some help for the diagnosis and treatment of gastrolithiasis.
We present the following article in accordance with the CARE reporting checklist.
Case report
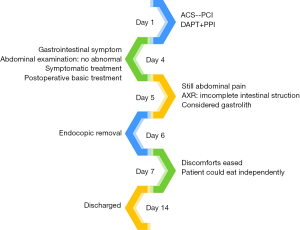
A 62-year-old female patient was referred to hospital with intermittently chest fillness and breathlessness for 3 years and aggravating for 3 days. As the timeline of this case in Figure 1 shows that during hospitalization, her angina pectoris recurred and the electrocardiogram (ECG) showed dynamic changes. Combined with her previous coronary angiography results, we considered it as an acute coronary syndrome, then a stent was inserted into her LAD by coronary angiography. Her angina pectoris was significantly relieved after the operation, and routine antiplatelet and rabeprazole sodium enteric-coated tablets (proton pump inhibitor, PPI) were given to her to prevent postoperative complications.
But on the 3rd day after the operation, the patient suffered from continuously abdominal distention, nausea and non-ejective vomiting once, and there was no obvious inducement for them. There was a large amount of undigested food in her vomit, and no obvious brown like substance was found.
After vomiting, abdominal pain occurred frequently. Besides, she had only defecated once until given glycerol enema to assist on the 4th day. She had no history of gastrointestinal diseases. Color Doppler of the upper abdomen showed many gastric contents in her stomach and Color Doppler of the superior mesenteric artery (SMA) showed that the blood of the SMA was circulating. No obvious abnormality was found on the abdominal X-ray (AXR) and upper abdomen CT. Based on the above examination results, the patient was given enema, gastrointestinal decompression, fasting for solids and liquids, fluid infusion, and continued to be given postoperative basic treatment.
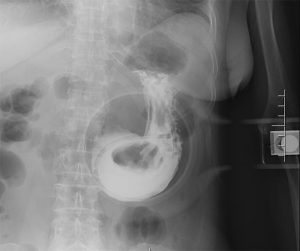
After treatment, her abdominal distension was slightly relieved on the 5th day, but the abdominal pain still remained. Nausea and vomiting occurred once more. The vomit was stomach contents, including a black hard substance whose size was like jujuba. Reexamination result of the AXR showed incomplete intestinal obstruction. According to the physical examinations, her body temperature, heart rate and blood pressure were all normal, and she was conscious all the time and cooperated with the examinations. Her abdomen was palpated flat and soft, without obvious tenderness and rebound pain, nor masses, the shifting dullness was negative and bowel sounds were normal. Upper gastrointestinal angiography revealed a 5.2 cm oval filling defect in her stomach, as shown in Figure 2, which could move in different positions and compressions, so gastrolithiasis was considered more likely. In addition, the duodenum was unblocked. It could be traced back to one month before admission that the patient had eaten a lot of hawthorn and crabs, and one week before admission, the patient had intermittent epigastric fullness and anepithymia.
After endoscopic removal on the 6th day, the patient’s discomforts were released mostly, and she could eat on her own. The patient got better and was discharged one week later. Through following-up, the patient is very careful of diet and her digestive system symptoms seldom appear so far.
Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Discussion
First, according to the analysis of the causes of the formation, gastrolith in China are mainly related to the food such as persimmon, jujube, hawthorn, etc., which contain a lot of tannic acid and pectin (4). These substances can combine with protein to form water-insoluble tannic acid protein and deposite in the stomach. The content of tannic acid in unripe and astringent fruit or peel is higher, and gastric bezoars are easy to occur after eating these foods (5). If the above foods are eaten together with high protein food such as fish, shrimp and crab, the risk of forming gastrolith will increase (6). In this case, the patient had a history of eating a lot of hawthorn and crabs, which was an important cause of her gastrolith. And she had a long-term regular oral administration of aspirin enteric-coated tablets, enalapril maleate tablets, atorvastatin calcium tablets before admission, these drugs have been reported for gastrointestinal adverse reaction, so it may be another risk factor for her gastrolith. Besides, although the use of PPI could reduce the risk of UGIB, the risk of gastrolithiasis progression may increase.
Second, gastrolith is easy to be missed diagnosis. The patient was admitted to the hospital mainly because of chest tightness and suffocation. After PCI, the main symptoms were relieved obviously, while the abdominal symptoms continued. ECG had been reexamined many times without any obvious change, the correlation between her abdominal symptoms and postoperative complications could be excluded. Therefore, we considered that it was mainly the digestive system problem, but patients with long-term use of aspirin may have chronic gastric injury, so acute gastritis was an interference factor in the initial diagnosis of gastrolithiasis. According to the patient’s symptoms and the results of physical examinations, imageological examinations and laboratory examinations, we can basically exclude acute inflammation of abdominal viscera (such as acute cholecystitis and acute pancreatitis), biliary colic, biliary ascariasis and SMA embolism. The patient had abdominal pain, nausea and vomiting, abdominal distension, and stool obstruction at the same time, and the AXR showed incomplete intestinal obstruction, which may easily mislead the diagnosis as acute intestinal obstruction. However, the physical examinations showed that the patient didn’t have acute abdominal diseases and surgical indications, which was the key to the differential diagnosis. Gastric retention and incomplete intestinal obstruction are the key point to determine the direction of the next examination, and the upper gastrointestinal radiography can be used as the basis of clinic diagnosis. Combined with the patient's diet history, it is more likely to be diagnosed as plant gastrolith. The incidence of gastrointestinal calculi is less than 1%, rare in clinic, which can be distributed in the whole digestive system, especially in the stomach (7). The diagnosis of gastrolith mainly depends on endoscopy, ultrasound and CT. AXR can show opaque gastrolith shadow, and the positive rate of diagnosis of non-metallic stomach foreign body is low. Upper gastrointestinal radiography is the first step in the diagnosis of gastrolith. Upper gastrointestinal endoscopy is the gold standard for diagnosis, and it is also suitable for treatment (3).
Third, currently available treatment options for plant gastrolith include the dissolution gastrolith of by Coca-Cola, removal by endoscopic devices, laparotomy, and laparoscopic surgery. Coca-Cola has poor effect on large and hard gastroliths. Surgical removal is inevitable for cases presenting with ileus or patients with refractory bezoars (8-10). Gastroscopy is not only an important diagnostic method for gastrolithiasis, but also a major therapeutic method. This patient had a large gastrolith, no obvious intestinal obstruction and gastric retention, so the better choice was to use the gastroscope lithotripsy. The patient was in the perioperative period of PCI, and DAPT was indispensable. UGIB is one of its adverse reactions, and also one of the complications of gastroscopy. Besides, some cases of UGIB after gastroscopy while taking aspirin have been reported. So there was a certain degree of risk in the treatment. In this case, the patient was cooperated and agreed with all of the treatment, and improved obviously after the removal operation, and there were no adverse events.
Thus, there were two notable points in the case. Firstly, it is difficult to speculate how long the gastrolith had been in the patient’s body. We suspect that the stress response caused by abdominal discomfort caused by gastrolithiasis was one of the inducing factors of ACS after admission. Secondly, gastroscopy after coronary stents inserted may cause high risk of UGIB according to the guideline (11), but UGIB didn’t appear in this case, so gastroscopy may be safe in the perioperative period of PCI while taking DAPT and PPI with no history of UGIB.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-467). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Association CM. Clinical Guidelines for Diagosis and Treatment of Digestive System Diseases. Beijing: People’s Health Publishing House; 2004.
- Ladas SD, Kamberoglou D, Karamanolis G, et al. Systematic review: Coca-Cola can effectively dissolve gastric phytobezoars as a first-line treatment. Aliment Pharmacol Ther 2013;37:169-73. [Crossref] [PubMed]
- Khan S, Jiang K, Zhu L-p, et al. Upper Gastrointestinal Manifestation of Bezoars and the Etiological Factors: A Literature Review. Gastroenterol Res Pract 2019;2019:5698532. [Crossref] [PubMed]
- Guan L, Liu T. Risk factors of gastric calculi and progress in the treatment of integrated traditional Chinese and Western Medicine. New Medicine 2019;50:400-3.
- Jin S, Xu Y. Types and diagnosis and treatment of gastrolith. Chinese Journal of clinicians (Electronic Edition) 2012;6:153-5.
- Liu Y, Li M, Jin L, et al. Upper Gastrointestinal Obstruction Caused by Gastrolithiasis After Laparoscopic Roux-en-Y Gastric Bypass: a Case Report. Obes Surg 2019;29:1937-8. [Crossref] [PubMed]
- Park SE, Ahn JY, Jung HY, et al. Clinical outcomes associated with treatment modalities for gastrointestinal bezoars. Gut Liver 2014;8:400-7. [Crossref] [PubMed]
- Lee BJ, Park JJ, Chun HJ, et al. How good is cola for dissolution of gastric phytobezoars? World J Gastroenterol 2009;15:2265-9. [Crossref] [PubMed]
- Sharma D, Srivastava M, Babu R, et al. Laparoscopic treatment of gastric bezoar. JSLS 2010;14:263-7. [Crossref] [PubMed]
- Zhang RL, Yang ZL, Fan BG. Huge gastric disopyrobezoar: a case report and review of literatures. World J Gastroenterol 2008;14:152-4. [Crossref] [PubMed]
- Veitch AM, Vanbiervliet G, Gershlick AH, et al. Endoscopy in patients on antiplatelet or anticoagulant therapy, including direct oral anticoagulants: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guidelines. Endoscopy 2016;48:385-402. [Crossref] [PubMed]