The effect of hemodialysis on serum magnesium concentration in hemodialysis patients
Introduction
Magnesium ions are the main intracellular cations after potassium (1), and the fourth most abundant group of ions in the body (1). Magnesium plays a central part in the maintenance of normal neuroendocrine function, muscle contraction, and cell signal transmission (1). Magnesium balance in the body is regulated by dietary intake of magnesium, intestinal magnesium absorption, the filtration of magnesium by glomeruli, renal magnesium reabsorption, and the utilization and release of magnesium ions from bone (1-3). When the rate of glomerular filtration decreases, the reduction in magnesium excretion may bring about hypermagnesemia (1,3). Dialysis can remove excessive magnesium (3,4).
Both hypomagnesemia and hypermagnesemia can cause functional disorders to develop. Arrhythmia, neuropsychiatric disorders, and respiratory depression can all result from serious magnesium disorders (1,3). Kanbay et al. suggested in their study that magnesium in patients with chronic kidney disease is related to insulin resistance, vascular endothelial dysfunction, and systemic inflammation (5). Nevertheless, in clinical practice, magnesium has received a relatively low amount of attention compared with other electrolytes.
Serum magnesium concentration was reported to be related to the prognosis of hemodialysis patients in 2014 (6). A U-shaped curve relationship between serum magnesium concentration and mortality in hemodialysis patients was described (6). In recent years, the concentration of magnesium in hemodialysis patients has drawn an increasing level of attention (3,4,6-10). However, previous studies have been inconsistent in their findings, with a large range reported in the magnesium concentrations of dialysis patients in various studies (3,4,6-10). The effect of magnesium on prognosis is still uncertain. Magnesium may be an influencing factor in prognosis or just a bystander (11). Although some Chinese studies have been carried out on magnesium metabolism in peritoneal dialysis and hemodialysis patients, these studies are still limited (12,13). The metabolic balance of magnesium in normal people depends on food intake, fecal and urine excretion (1-3). Different from normal people, it is really necessary to consider the clearance of magnesium ion by dialysis (4). Dialysis may be an important factor for magnesium regulation in dialysis patients. However, studies on both hemodialysis and peritoneal dialysis and magnesium metabolism are very limited (8,9,12,13). In previous studies, the effect of dialysis on the concentration of magnesium ion has not been investigated (3,5-8,10-12). In a prospective observational cohort study, the effect of routine hemodialysis treatment on post-dialysis plasma magnesium concentrations in chronic hemodialysis patients was investigated (4). However, the sample size of the previous study was small. Only 34 patients were included in the study (4). To our knowledge, no studies to date have investigated the effect of hemodialysis on magnesium concentration in a Chinese population. Bearing the possible relationship between serum magnesium concentration and mortality in dialysis patients in mind, such a study is called for. The current single-center, retrospective study set out to investigate the serum magnesium concentrations in hemodialysis patients and examine the factors related to the serum magnesium concentration, as well as to explore the effect of hemodialysis with conventional hemodialysis solution (magnesium ion concentration 0.5 mmol/L) on blood magnesium concentration. It is hoped that this study will improve our understanding of the influence of conventional hemodialysis solution on magnesium concentration in hemodialysis patients. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-992).
Methods
Patient selection
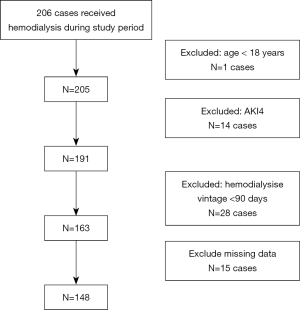
All patients who received hemodialysis treatment in our hospital between Nov 1, 2017, and Oct 31, 2018, were screened for the current study. The inclusion criteria were as follows: 1. uremic patients who had received hemodialysis treatment for a period of more than 90 days; and 2. pre-dialysis and post-dialysis total serum magnesium concentrations were tested at least once during the study period. The exclusion criteria were as follows: (I) aged <18 years old; (II) acute renal injury; (III) received hemodialysis therapy for a period of less than 90 days; (IV) without total serum magnesium concentration data.
The study was approved by the ethics committee of Tangdu Hospital (No. TDLL-201812-27). Informed consent was waived by the ethics committee, in consider of the study’s retrospective nature.
Databases and variables
Outpatient and inpatient data and variables were collected from the Electronic Medical Information System and information system at the hemodialysis center at our hospital. The dialyzers used in our hospital were Baxter gambro AK96 (membrane surface area 1.4 m2, membrane material polyamide). The dialysate was supplied via a central dialysis concentrate supply system. The magnesium ion concentration in the dialysate was 0.5 mmol/L. During hemodialysis treatment, the blood flow ranged between 200–280 mL/min, and the dialysate flow was 500 mL/min.
Patient information including demographic data, primary diseases, dialysis vintage, vascular access, hemodialysis treatment frequency, comorbidity, self-medication history, and prescription was collected. Laboratory variables included hemoglobin, total platelet count, white blood cell count, alanine aminotransferase (ALT), plasma albumin, alkaline phosphatase (ALP), intact parathyroid hormone (iPTH), blood total cholesterol, triglyceride, C-reactive protein (CRP), blood urea, serum creatinine (Scr), uric acid (UA), and electrolytes (total serum magnesium, total calcium, sodium, potassium, chloride, phosphorus, and carbon dioxide binding rate). During the study period, some patients may receive multiple magnesium ion tests. We only selected the values of magnesium concentrations before and after dialysis at the same hemodialysis therapy. In cases where the post-dialysis magnesium concentrations of a patient had been evaluated multiple times, the first test was used.
Previous studies have shown that some drugs can cause magnesium metabolic disorders. These drugs included proton pump inhibitors, diuretics, laxative, calmodulin inhibitors (CNI) cisplatin and anti-epidermal growth factor receptor (EGFR) agents (14-18). In the current study, patients with a history of using the above drugs up to two weeks before the laboratory tests were included.
Sample collection and assay method
Before hemodialysis treatment, samples were collected by nurses from the arteriovenous fistula or peripheral vein. If vascular access was gained with a hemodialysis catheter, the blood samples were obtained from the peripheral vein. After hemodialysis treatment, samples were collected from the peripheral vein. The samples were sent to the hospital laboratory within 30 minutes. The samples were dealt with within 2 h and centrifuged at 3,500 rpm for 5 minutes. Electrolytes (including total serum magnesium) were measured by toluidine blue method [BECKMAN AU5800, America, Reagent (original reagent)], and serum creatinine level was measured by autoanalyzer (BECKMAN AU5800, America).
Definition
Based on the manufacturer’s instructions, the normal total magnesium reference range was from 0.77 to 1.03 mmol/L. In the current study, hypomagnesemia was defined as total serum magnesium of <0.77 mmol/L. If the total magnesium in plasma was >1.03 mmol/L, hypermagnesemia was diagnosed. Hypoalbuminemia was defined as a plasma albumin level of <35 g/L.
Statistical analysis
The continuous variables were presented by mean ± standard deviation or median and quartile. Statistically significant difference was represented by P value <0.05. The differences between variables pre- and post-dialysis were compared by paired t-test.
The relationships between variables and total serum magnesium were examined with linear regression models. Model-1 was unadjusted, while model-2 was adjusted for age, gender, dialysis vintage, diabetes (19), dialysis treatment frequency per week, and vascular access. On the basis of model-2, model-3 was further adjusted for pre-dialysis serum phosphorus, pre-dialysis blood urea, pre-dialysis plasma albumin, pre-dialysis triglyceride, iPTH, and ALP (6). For the continuous variables with non-normal distribution, the logarithm transformation was carried out before the regression models were established.
Results
Between Nov 1, 2017, and Oct 31, 2018, 186 patients received hemodialysis treatment in our hospital. The current study included 148 patients of these patients. Patients <18 years old, patients with acute kidney injury or dialysis vintage <90 days, and patients without blood magnesium data were excluded (Figure 1). In the study period, 18 patients received multiple tests of the post-dialysis magnesium concentrations. Only the first test results were used in the current study.
Characteristics of patients (Table 1)
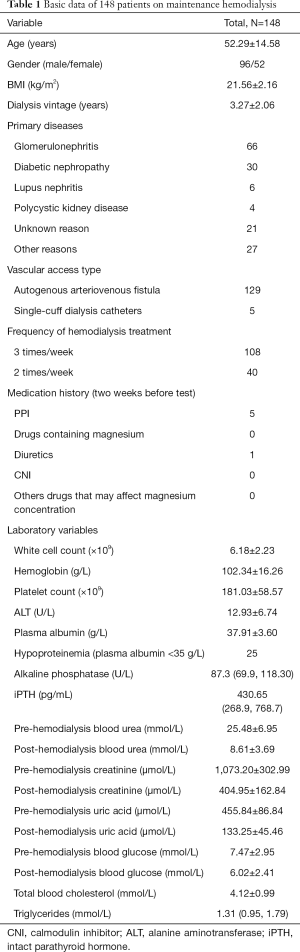
Full table
Of the 148 included patients, 96 (64.86%) were male and 52 (35.14%) were female. The patients ranged in age from 22–84 years old, with an average age of 52 years old. Glomerulonephritis (66 cases) was the most common etiology of end-stage renal disease (ESRD). Diabetic nephropathy was also a major cause of ESRD within the cohort (30 cases in total). Other causes included, for instance, lupus nephritis and polycystic kidney disease. In 129 patients, the vascular access in hemodialysis was via autogenous arteriovenous fistula. One hundred and eight patients received hemodialysis treatment 3 times a week, while the other 40 patients received hemodialysis twice a week. In the two weeks prior to undergoing serum magnesium examination, five patients had taken PPI and one patient had taken furosemide. None of the other patients had taken any medications that may have affected the serum magnesium concentration.
The effect of hemodialysis on serum magnesium concentration
Levels of electrolytes before and after dialysis in 148 patients on maintenance hemodialysis were presented in Table 2. The mean pre-hemodialysis serum magnesium concentration was 1.11±0.14 mmol/L. Two patients had hypomagnesemia, 109 patients had hypermagnesemia, and the prevalence of hypermagnesemia was 73.65%. Among the five patients who were taking PPI, the pre-dialysis serum magnesium concentration ranged from 0.93 to 1.16 mmol/L.
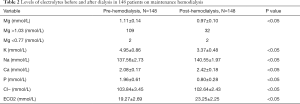
Full table
After dialysis treatment, the serum magnesium concentration was 0.97±0.10 mmol/L. The average serum magnesium concentration had decreased by an average of 0.14 mmol/l, which was significantly lower (P<0.001). Serum magnesium concentration was decreased in 135 patients. A minority of patients (13 cases) had lower serum magnesium concentration after dialysis treatment, while 32 patients had elevated serum magnesium concentration (>1.03 mmol/L) after dialysis treatment. In the two patients with hypomagnesemia before hemodialysis, the concentrations of blood magnesium after dialysis were increased (from 0.66 to 0.70 mmol/L, from 0.73 to 0.75). Post-dialysis serum magnesium concentration was highly correlated with pre-dialysis serum magnesium (coef. 0.88, P<0.001). The difference between the magnesium concentration before and after dialysis was also highly correlated with pre-dialysis magnesium concentration (coef. 0.89, P<0.001). The levels of electrolytes before and after hemodialysis are shown in Table 2.
Relationship of variables with serum blood magnesium concentration in hemodialysis patients
In the unadjusted linear regression model, age, hemoglobin, platelet count, pre-dialysis potassium, pre-dialysis total plasma calcium, pre-dialysis phosphorus, pre-dialysis serum creatinine, pre-dialysis blood urea, pre-dialysis plasma albumin, iPTH level, and total cholesterol were found to be significantly related to pre-dialysis serum magnesium concentration (P<0.05). However, only total platelet count, pre-dialysis serum phosphorus, pre-dialysis serum creatinine, serum plasma albumin, and total cholesterol were significantly related to the concentration of pre-hemodialysis serum magnesium (P<0.05) (Table 3).
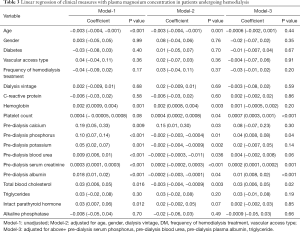
Full table
Discussion
We conducted a single-center, retrospective study to investigate the effect of hemodialysis on serum magnesium concentration. Up to now, studies on effect of hemodialysis on serum magnesium concentration are very limited. The results showed that the average pre-dialysis concentration of total serum magnesium was 1.11±0.14 mmol/L. While only two patients had hypomagnesemia, the prevalence of hypermagnesemia was 73.65%. Linear regression analysis showed total platelet count, pre-dialysis serum phosphorus, serum creatinine, plasma albumin, total cholesterol to be significantly related to serum magnesium concentration. The above findings suggested that a relationship may exist between serum magnesium concentration and dietary and nutritional status. Comparing the differences in pre-dialysis and post-dialysis magnesium concentration, it was indicated that conventional hemodialysate (dialysate magnesium ion concentration 0.5 mmol/L) can remove blood magnesium ions. The average decrease in serum magnesium concentration after dialysis treatment was 0.14 mmol/L.
In healthy individuals, the magnesium is regulated through glomerular filtration and renal tubular reabsorption in the kidneys (1,2). Renal failure can affect the metabolism of magnesium ion. As renal failure develops, it can cause magnesium metabolism disorders (1-3). In recent years, more attention has been paid to the magnesium metabolism of hemodialysis patients (6-10,12,20). Several studies have reported that serum magnesium concentration is related to mortality and CV events in hemodialysis and peritoneal dialysis patients (6-9,12,20). Cunningham et al. summarized the studies of the serum magnesium concentration on dialysis patients before 2012 and found that the mean value of serum magnesium concentration in patients who underwent hemodialysis or peritoneal dialysis was 0.78–1.40 and 0.55–1.27 mmol/L, retrospectively (3). However, the studies summarized by Cunningham et al. (3) were based on small samples. Furthermore, only 47 of the patients in Cunningham’s summary received treatment with dialysate containing 0.5 mmol/L magnesium ion, with an average serum magnesium concentration of 1.01 mmol/L, whereas the concentration of magnesium ion in dialysate is 0–0.75 mmol/L (3). Since 2014, epidemiological investigations, including large-sample studies in Japan and the United States (6,7), have reported the blood magnesium concentration in hemodialysis patients. In the Japanese study, the average blood magnesium concentration of 142,555 hemodialysis patients was 1.09 mmol/L (6). In the U.S. investigation, 21,534 patients with maintenance hemodialysis had an average blood magnesium concentration of 0.92±0.16 mmol/L (7). In the study based on a Chinese population, Wu et al. reported the serum magnesium concentration of 169 patients with maintenance hemodialysis and the average pre-dialysis serum magnesium concentration was 1.00±0.18 mmol/L (8). In another study, the mean serum magnesium concentration of 115 Chinese patients who received peritoneal dialysis was 0.95 mmol/L (9).
Compared with previous studies (8,9), the hemodialysis patients in the current study had a slightly higher concentration of serum magnesium, with an average value of 1.12 mmol/L. We also reported a higher prevalence of hypermagnesemia. The potential causes are as follows: the average age of the patients in our cohort was 50 years, which is younger than that of the patients in the previous studies. The analysis of unadjusted linear regression model revealed age to be significantly related to serum magnesium concentration. Previous studies (21), like the current study, have suggested that the blood magnesium concentration is related to patients’ nutritional status. Younger patients may have better dietary intake and nutritional status, so serum blood magnesium concentration is therefore slightly higher. Some drugs may induce a decrease in serum magnesium concentration (14-18). Previous studies have reported that a higher rate of PPI use may be related to the lower magnesium concentration in hemodialysis patients (4,22). In the current study, in the two weeks prior to the test, only five patients took PPI. Avoiding long-term PPI use may reduce the prevalence of hypomagnesemia in hemodialysis patients. In this study, 40 patients received hemodialysis twice a week. In the current study, we observed that the serum magnesium concentration decreased after hemodialysis. In these patients, relatively high blood magnesium concentration could possibly be attributed to the reduction in dialysis clearance of magnesium ions. The linear regression model did not indicate that dialysis frequency was related to blood magnesium concentration. However, in the current study, the blood magnesium concentration of the patients who received dialysis twice a week was higher than that of the patients who were dialyzed three times a week
Previous studies have suggested that pre-dialysis magnesium concentration is related to the outcomes of dialysis patients (6,7,12,20,23). The aforementioned large-scale Japanese study suggested a U-shaped association between magnesium concentration and mortality in hemodialysis patients (6). However, the large-scale American study showed that the mortality of dialysis patients increased when serum magnesium concentration was low, and a U-shaped curve was not present (7). The above studies support the idea that hemodialysis patients may need a slightly higher level of blood magnesium concentration than healthy individuals. However, not all studies have supported the correlation between magnesium concentration and mortality. Other studies have suggested that the association between magnesium concentration and mortality is dependent on the level of plasma albumin (24,25). It may be suggested that hypomagnesemia is only one of the signs of malnutrition, rather than a cause of increased mortality. The results of the current study showed that hemoglobin, platelet count, potassium level before dialysis, blood phosphorus, serum creatinine, urea, plasma albumin, and total cholesterol were significantly related to the serum magnesium concentration. These results suggest that blood magnesium concentration is related to dietary intake and nutritional status, and it is therefore possible that a relatively low serum magnesium concentration acts only as a bystander.
Serum calcium level, calcitriol, and FGF-23 play an important role in the regulation of PTH synthesis and secretion (26). The calcium-sensing receptor of the parathyroid gland is regulated by the level of plasma calcium ions (26), and it can also be affected by magnesium ions. Although the specific mechanism of magnesium ion-regulated PTH secretion has not been completely eliminated, it may inhibit PTH regardless of hypermagnesemia or severe hypomagnesemia (27,28). Previous studies on the relationship between the level of serum magnesium and PTH in dialysis patients produced inconsistent results. Although several studies have shown that low magnesium in hemodialysis patients is associated with increased PTH, other studies do not support this result (3). In this study, no correlation was identified between magnesium concentration and PTH. At present, there is a lack of well-designed research to clarify the relationship between magnesium ions and PTH (3).
In hemodialysis treatment, magnesium ions, as small molecules, can be easily removed by diffusion and convection through the dialysis membrane (1,3,4). Total magnesium in plasma includes magnesium ion, protein-bound magnesium, and other complexes (1,3,4). The movement of magnesium ions on both sides of the dialysis membrane is affected by the ratio of magnesium ions to total magnesium in the plasma, the concentration gradient of magnesium ions in dialysate and blood, and dialysis ultrafiltration (3,4). In addition, the Gibbs-Donnan effect caused by negatively charged proteins in plasma cannot be ignored (3). In studies in which 0–0.25 mmol/L magnesium ion concentration was used, the plasma magnesium concentration of patients decreased significantly (29-31). At present, dialysate with 0.5 mmol/L magnesium ion concentration is widely used in hemodialysis. Leenders et al. (4) used dialysate with 0.5 mmol/L magnesium ion concentration to measure the blood magnesium of 34 hemodialysis patients before and after hemodialysis. The results showed that the average decrease of serum magnesium concentration after hemodialysis was 0.1 mmol/L. The results of this study also indicated that the plasma magnesium concentration decreased by an average of 0.14mmol/L after the treatment with 0.5 mmol/L dialysate. In Leenders et al.’s study, the mean blood magnesium concentration of the 34 patients was relatively low (0.88 mmol/L). Among the 34 patients, 25 patients took PPI orally, 18 patients took diuretics, and 1 patient took CNIs (4). The above drugs may be one of the reasons for the relatively low blood magnesium concentration in this group. The statistical analysis of this previous study showed that gender, age, plasma albumin, hemoglobin, plasma bicarbonate concentration, body weight, vascular access type, blood flow, and hemodialysis filtration were not significantly related to the blood magnesium of dialysis patients before and after dialysis, and only ultrafiltration volume was related to the blood magnesium level after dialysis (4). Compared with the study of Leenders et al., our study holds the advantage of having a relatively large sample size, having analyzed data from 148 hemodialysis patients. However, Leenders’ study involved repeated observation and compared blood magnesium concentration pre- and post-dialysis.
This study has some limitations that must be addressed. First, the study’s single-center, retrospective nature made bias inevitable. Second, the study could not include all confounding factors, such as diet, residual renal function, and ultrafiltration, for example. Third, we only measured the total plasma magnesium concentration, and did not measure the magnesium ion concentration. During dialysis, only magnesium ions can be diffused. Although there is a significant relationship between the concentration of magnesium ions in hemodialysis patients and plasma magnesium, a patient’s magnesium ion concentration changes over time (32,33). The detection of magnesium ion concentration is able to reflect the low magnesium or hypermagnesemia that can not be reflected by measuring blood total magnesium concentration alone (32,33). It is therefore better to determine the total magnesium and magnesium ion concentration in plasma. Finally, we have to admit that we cannot include all potential factors in the current study.
Conclusions
The results of this study show that most hemodialysis patients have mild hypermagnesemia when they are treated with 0.5 mmol/L magnesium ion conventional dialysate. A patient’s blood magnesium concentration is related to their nutritional status. In most cases, after hemodialysis, some magnesium ions can be removed from the body, resulting in a decrease in blood magnesium concentration.
Acknowledgments
Funding: This work was supported by grant from the Scientific Nurturing Program Of Beijing Municipal Hospital (PX2018070).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-992
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-992
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-992). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the ethics committee of Tangdu Hospital (No. TDLL-201812-27). Informed consent was waived by the ethics committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jahnen-Dechent W, Ketteler M. Magnesium basics. Clin Kidney J 2012;5:i3-14. [Crossref] [PubMed]
- Liu M, Yang H, Mao Y. Magnesium and liver disease. Ann Transl Med 2019;7:578. [Crossref] [PubMed]
- Cunningham J, Rodriguez M, Messa P. Magnesium in chronic kidney disease Stages 3 and 4 and in dialysis patients. Clin Kidney J 2012;5:i39-51. [Crossref] [PubMed]
- Leenders NHJ, Ittersum FJV, Hoekstra T, et al. Routine hemodialysis induces a decline in plasma magnesium concentration in most patients: a prospective observational cohort study. Sci Rep 2018;8:10256. [Crossref] [PubMed]
- Kanbay M, Yilmaz MI, Apetrii M, et al. Relationship between serum magnesium levels and cardiovascular events in chronic kidney disease patients. Am J Nephrol 2012;36:228-37. [Crossref] [PubMed]
- Sakaguchi Y, Fujii N, Shoji T, et al. Hypomagnesemia is a significant predictor of cardiovascular and non-cardiovascular mortality in patients undergoing hemodialysis. Kidney Int 2014;85:174-81. [Crossref] [PubMed]
- Lacson E, Wang W, Ma L, et al. Serum Magnesium and Mortality in Hemodialysis Patients in the United States: A Cohort Study. Am J Kidney Dis 2015;66:1056-66. [Crossref] [PubMed]
- Wu L, Cai K, Luo Q, et al. Baseline Serum Magnesium Level and Its Variability in Maintenance Hemodialysis Patients: Associations with Mortality. Kidney Blood Press Res 2019;44:222-32. [Crossref] [PubMed]
- Li G, Zhang L, Ren H, et al. Clearance of Magnesium in Peritoneal Dialysis Patients: A Single-Center Study. Blood Purif 2019;47:1-7. [Crossref] [PubMed]
- Shimohata H, Yamashita M, Ohgi K, et al. The relationship between serum magnesium levels and mortality in non-diabetic hemodialysis patients: A 10-year follow-up study. Hemodial Int 2019;23:369-74. [PubMed]
- Courivaud C, Davenport A. Magnesium and the risk of all-cause and cardiac mortality in hemodialysis patients: agent provocateur or innocent bystander? Kidney International 2014;85:17-20. [Crossref] [PubMed]
- Yu L, Li H, Wang SX. Serum Magnesium and Mortality in Maintenance Hemodialysis Patients. Blood Purif 2017;43:31-6. [Crossref] [PubMed]
- Ye H, Cao P, Zhang X, et al. Serum Magnesium Abnormality and Influencing Factors of Serum Magnesium Level in Peritoneal Dialysis Patients: A Single-Center Study in Northern China. Br J Nutr 2018;120:415-23. [Crossref] [PubMed]
- Shah GM, Kirschenbaum MA. Renal magnesium wasting associated with therapeutic agents. Miner Electrolyte Metab 1991;17:58-64. [PubMed]
- Lajer H, Daugaard G. Cisplatin and hypomagnesemia. Cancer Treat Rev 1999;25:47-58. [Crossref] [PubMed]
- Nijenhuis T, Hoenderop JG, Bindels RJ. Downregulation of Ca(2+) and Mg(2+) transport proteins in the kidney explains tacrolimus (FK506)-induced hypercalciuria and hypomagnesemia. J Am Soc Nephrol 2004;15:549-57. [Crossref] [PubMed]
- Costa A, Tejpar S, Prenen H, et al. Hypomagnesaemia and targeted anti-epidermal growth factor receptor (EGFR) agents. Target Oncol 2011;6:227-33. [Crossref] [PubMed]
- Fatuzzo P, Portale G, Scollo V, et al. Proton pump inhibitors and symptomatic hypomagnesemic hypoparathyroidism. J Nephrol 2018;30:297-301. [PubMed]
- Chen W, Fitzpatrick J, Monroy-Trujillo JM, et al. Diabetes Mellitus Modifies the Associations of Serum Magnesium Concentration With Arterial Calcification and Stiffness in Incident Hemodialysis Patients. Kidney Int Rep 2019;4:806-13. [Crossref] [PubMed]
- Yang X. Serum Magnesium Levels and Hospitalization and Mortality in Incident Peritoneal Dialysis Patients: A Cohort Study. Am J Kidney Dis 2016;68:619-27. [Crossref] [PubMed]
- Joffres MR, Reed DM, Yano K. Relationship of magnesium intake and other dietary factors to blood pressure. The Honolulu Heart Study. Am J Clin Nutr 1987;45:469-75. [Crossref] [PubMed]
- Alhosaini M, Walter JS, Singh S, et al. Hypomagnesemia in Hemodialysis Patients: Role of Proton Pump Inhibitors. Am J Nephrol 2014;39:204-9. [Crossref] [PubMed]
- Ferrè S, Li X, Adams-Huet B, et al. Association of serum magnesium with all-cause mortality in patients with and without chronic kidney disease in the Dallas Heart Study. Nephrol Dial Transplant 2018;33:1389-96. [Crossref] [PubMed]
- Mizuiri S, Nishizawa Y, Yamashita K, et al. Hypomagnesemia is not an independent risk factor for mortality in Japanese maintenance hemodialysis patients. Int Urol Nephrol 2019;51:1043-52. [Crossref] [PubMed]
- Tamura T, Unagami K, Okazaki M, et al. Serum Magnesium Levels and Mortality in Japanese Maintenance Hemodialysis Patients. Blood Purif 2019;47:88-94. [Crossref] [PubMed]
- Kumar R, Thompson JR. The regulation of parathyroid hormone secretion and synthesis. J Am Soc Nephrol 2011;22:216-24. [Crossref] [PubMed]
- Massry SG, Coburn JW, Kleeman CR. Evidence for suppression of parathyroid gland activity by hypermagnesemia. J Clin Invest 1970;49:1619-29. [Crossref] [PubMed]
- Ferment O, Garnier PE, Touitou Y. Comparison of the feedback effect of magnesium and calcium on parathyroid hormone secretion in man. J Endocrinol 1987;113:117-22. [Crossref] [PubMed]
- Gonella M, Buzzigoli G, Bencivelli W, et al. The determination of whole blood magnesium concentration in uremics on chronic dialysis. Nephron 1981;28:88-9. [Crossref] [PubMed]
- Nilsson P, Johansson SG, Danielson BG. Magnesium studies in hemodialysis patients before and after treatment with low dialysate magnesium. Nephron 1984;37:25-9. [Crossref] [PubMed]
- Kelber J, Slatopolsky E, Delmez JA. Acute effects of different concentrations of dialysate magnesium during high-efficiency dialysis. Am J Kidney Dis 1994;24:453-60. [Crossref] [PubMed]
- Saha H, Harmoinen A, Pietila K, et al. Measurement of serum ionized versus total levels of magnesium and calcium in hemodialysis patients. Clin Nephrol 1996;46:326-31. [PubMed]
- Del Giorno R, Riva H, Donato G. Ionized and total serum magnesium in hemodialysis: predictors and variability. A longitudinal cross-sectional study. Clin Exp Nephrol 2018;22:620-8. [Crossref] [PubMed]