
Impacts of different administration modes of dexmedetomidine with 0.5% ropivacaine on intercostal nerve block
Introduction
The features of an intercostal nerve block are a simple operation, accurate effect, small impact on breathing, and stable hemodynamics. It is one of the commonly used anesthesia methods for lumpectomy (1,2). Dexmedetomidine is a highly selective α2-adrenoreceptor agonist having multifaceted attributes of sedation, anxiolysis, hypnosis, analgesia, and sympatholysis (3). When combined with local anesthetics, it may improve regional block and intrathecal anesthesia (4,5). In our current study, we compared the impacts of different administration modes of dexmedetomidine on the effectiveness of intercostal nerve block and the duration of postoperative analgesia, thus informing the rational use of clinical drugs.
Methods
General data
This study was approved by the Ethics Committee of Wuxi Maternity and Child Health Care Hospital, and all the subjects and their families signed the informed consent forms.
The inclusion criteria included: American Society of Anesthesiologists (ASA) class: I–II; age: 20–45 years; body mass index (BMI): 18.5–23.9 kg/m2; and undergoing elective lumpectomy. The exclusion criteria included: with severe heart, liver, kidney and/or blood system diseases; long-term user of sedative and analgesic drugs; and with a history of allergy to local anesthetics and/or alcoholism before surgery.
The patients were randomly divided into three groups by using a table of random numbers: group D1: perineural administration of dexmedetomidine0.5 µg/kg + intercostal nerve block with 0.5% ropivacaine); group D2: intravenous infusion of dexmedetomidine 0.5 µg/kg + intercostal nerve block with 0.5% ropivacaine; and group R: intercostal nerve block with 0.5% ropivacaine.
Anesthesia methods
All patients fasted before surgery. After the patients entered the operating room, they were checked with an electrocardiogram (ECG) and their heart rate (HR), blood pressure (BP), and blood oxygen saturation (SpO2) were measured. A face mask was applied for oxygen delivery at a rate of 3 L/min. Open venous channels were created to enable the compound sodium lactate infusion at a rate of 10 mL/kg per hour. In group D1, perineural administration of 0.5 µg/kg dexmedetomidine (Hengrui Medicine, Jiangsu Province, China; lot number: 181230BP) + intercostal nerve block with 0.5% ropivacaine (Qilu Pharmaceutical; lot number: 8B132C35) was applied. In group D2, after successful intercostal nerve block with 0.5% ropivacaine, intravenous infusion of 0.5 µg/kg dexmedetomidine was applied till the end of surgery. Group R received the intercostal nerve block with 0.5% ropivacaine only. All patients underwent intercostal nerve block via the anterior axillary approach. The T2 to T6 intercostal space was selected. The needle was inserted perpendicularly at the intersection between the lower edge of the rib and the anterior axillary line. After the lower edge of the rib was reached, the needle was inserted downwards and inwards 3–5 mm. If there was no blood or air return in the syringe, 5 mL of anesthetic solution was injected. Four intercostal nerves were blocked simultaneously according to the location of the mass. If the intercostal nerve block was inadequate, conversion to general anesthesia was needed, and the patients were ruled out from the study. If the intraoperative mean arterial pressure (MAP) decreased and the fluctuation range was greater than 30% of the basal value, intravenous injection of ephedrine 10 mg was needed. If the HR was below 50 bpm, intravenous injection of atropine 0.5 mg was applied. If the SpO2 was <90%, mask-assisted ventilation was given. After the surgery, a single intravenous injection of tramadol 1–2 mg/kg would be applied for rescue analgesia if the patients required.
Main measures
The main measures included: NRS scores (0 representing no pain and 10 representing worst pain) and Ramsay sedation scores (1 point: not quiet, agitated patients; 2 points: quiet and cooperative patients; 3 points: drowsy and obeying directive; 4 points: drowsy and responding to tactile stimulation; 5 points: lethargic and only responding to strong stimulation; 6 points: in deep sleep, no response to calling; a score of 1 means unsatisfactory sedation, 2–4 means satisfactory sedation, and 5–6 means excessive sedation); duration of postoperative analgesia; number of cases requiring rescue analgesia; and adverse reactions such as dizziness, dry mouth, nausea, vomiting, and respiratory depression.
Statistical analysis
Statistical analysis was performed using SPSS 17.0 software. The measurement data were expressed as mean ± standard deviation ( ), and the inter-group comparisons were performed using one-way ANOVA. Comparisons of count data were performed using the chi-square test, with a P value of less than 0.05 being considered statistically significant.
Results
The ASA classification, age, and BMI were matched among these three groups.
The NRS scores in groups D1 and D2 were significantly lower than that in group R 8 hours after the operation (both P<0.05), and the NRS score in group D1 was significantly lower than in group D2 12 hours after operation (P<0.05). The Ramsay scores showed no significant differences among all three groups at all time points after surgery (Table 1).
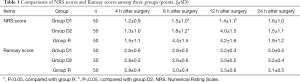
Full table
The duration of postoperative analgesia was significantly longer in groups D1 [(14.2±1.2) h], and D2 [(9.0±0.6) h] in group R [(7.1±0.4) h] (both P<0.05), and group D1 also had significantly longer duration of postoperative analgesia than in group D2 (P<0.05).
No rescue analgesia was needed in all three groups, and no adverse reactions such as dizziness, dry mouth, nausea, vomiting, and respiratory depression were reported.
Discussion
Regional anesthesia has increasingly become popular among surgeons and patients with the development of enhanced recovery after surgery (ERAS) and comfort medicine. An intercostal nerve block is widely used in lumpectomy due to its simplicity and definite analgesic effect. Ropivacaine is a long-acting amide local anesthetic agent. It is thought to provide greater separation of sensory and motor effects, with fewer cardiac toxicities. However, ropivacaine alone has a short duration when used for nerve block and its role in postoperative analgesia is limited; thus, it is not possible for ERAS and comfort medicine to work together.
Dexmedetomidine is a highly selective α2-adrenergic receptor agonist. It is 1,600-fold more selective for α2 receptor than for ɑ1 receptor and has an elimination half-life of 2 to 3 hours (3). Studies have found that the combination of dexmedetomidine and ropivacaine can enhance the effects of peripheral nerve block and prolong the duration of sensory block (6,7). In our current study, intravenous infusion of dexmedetomidine 0.5 µg/kg combined with intercostal nerve block with 0.5% ropivacaine achieved longer postoperative analgesia duration [(9.0±0.6) h], which was significantly longer than that [(7.1±0.4) h] of intercostal nerve block with 0.5% ropivacaine alone, along with the significantly lower NRS score at 8 h after surgery. This may be because dexmedetomidine can act on the α2 receptor in the nucleus ceruleus of the brainstem to exert its sedative-hypnotic and antianxiety effects and relieve the patient’s stress; also, it can act on the α2 receptors on the spinal cord and peripheral nerves to produce analgesic effects and enhance the analgesic effect and duration of local anesthetics (8). Also in our current study, perineural administration of 0.5 µg/kg dexmedetomidine + intercostal nerve block with 0.5% ropivacaine had significantly longer postoperative analgesia duration [(14.2±1.2) h] than intravenous infusion of dexmedetomidine 0.5 µg/kg combined with intercostal nerve block with 0.5% ropivacaine, along with the significantly lower NRS score at 12 h after surgery. The possible reasons may be as follows: (I) at the level of the spinal cord, dexmedetomidine acts on the α2 receptors on both presynaptic and postsynaptic membranes, inhibiting the release of adrenaline; also, it acts on the α2 receptor in the spinal dorsal horn neurons, inhibiting the release of substance P and other pain mediators and thereby inhibiting the transmission of pain signals; (II) at the level of peripheral nerves, dexmedetomidine inhibits the production of action potentials by C and Aδ fibers, enhances the suppression of Na + channels by local anesthetics, and blocks the conduction of excitation; (III) dexmedetomidine acts on the α2 receptors in peripheral vascular smooth muscle cells to constrict the peripheral blood vessels, reduce the absorption of local anesthetics, and prolong the block time (7,9).
The effects of dexmedetomidine on the cardiovascular system are shown as the lowered HR and hypotension, which is related to the dose and infusion speed of dexmedetomidine. Thus, it must be used with caution in patients with severe ventricular dysfunction or severe atrioventricular block (10). Although no patient in our current study experienced severe hypotension or bradycardia, ephedrine and atropine were prepared during the surgery to prevent the occurrence of hypotension and bradycardia.
Conclusions
Both two administration modes of dexmedetomidine with ropivacaine for intercostal nerve block can prolong the duration of analgesia after lumpectomy; however, the duration of analgesia is longer via the perineural route than via the intravenous route.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form and declare: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Ethics Committee of Wuxi Maternity and Child Health Care Hospital (No. 2020-06-0120-01), and all the subjects and their families signed the informed consent forms.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wang WW, Zhou WD, Wang X. The effect of the ultrasound-guided intercostal nerve block in the unilateral lumpectomy. J Clin Anesth 2015;31:763-5.
- Liang XH, Luo XQ. Application of intercostal nerve block in lumpectomy. Jiangxi Medical Journal 2016;51:1111-3.
- Miller. Miller's Anesthesia. Translated by Zeng YM, Deng XM. Beijing: Peking University Medical Press, 2006:359-62.
- Liu L, Qian J, Shen B, et al. Intrathecal dexmedetomidine can decrease the 95% effective dose of bupivacaine in spinal anesthesia for cesarean section: A prospective, double-blinded, randomized study. Medicine (Baltimore) 2019;98:e14666. [Crossref] [PubMed]
- Andersen JH, Jaeger P, Grevstad U, et al. Systemic dexmedetomidine is not as efficient as perineural dexmedetomidine in prolonging an ulnar nerve block. Reg Anesth Pain Med 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Koraki E, Stachtari C, Kapsokalyvas I, Stergiouda Z, Katsanevaki A, Trikoupi A. Dexmedetomidine as an adjuvant to 0.5% ropivacaine in ultrasound-guided axillary brachial plexus block. J Clin Pharm Ther 2018;43:348-52. [Crossref] [PubMed]
- Yu L, Sheng L, Hang DY, et al. Effects of different doses of dexmedetomidine on the effectiveness of intercostal nerve block with ropivacaine. Journal of Clinical Anesthesiology 2016;32:1217-8.
- Nguyen V, Tiemann D, Park E, et al. Alpha-2 Agonists. Anesthesiol Clin 2017;35:233-45. [Crossref] [PubMed]
- Hou YY, Wen QP. Novel approaches of dexmedetomidine using in intravertebral anesthesia. International Journal of Anesthesiology and Resuscitation 2014;35:735-8.
- Wu XM, Xue ZG, Ma H, et al. Expert consensus on the clinical use of dexmedetomidine (2018). Journal of Clinical Anesthesiology 2018;34:820-3.


