
Prevalence and contributing factors of osteoporosis in the elderly over 70 years old: an epidemiological study of several community health centers in Shanghai
Introduction
Osteoporosis (OP) is characterized by the decreased bone mass and destruction of the bone microstructure, which may increase the bone fragility and cause the susceptibility to fracture (1). The senile OP generally refers to the primary OP that occurs after the age of 70. The typical clinical manifestations of senile OP are the pain, shortened height, kyphosis, bone fracture and respiratory disorder. Senile OP is the main cause of bone fracture in the elderly. It seriously affects the health status and quality of life of the elderly, even endangers life, and increases the medical burden to society and families.
With the increasing emphasis on the OP in the communities in recent years, most of the elderly in Shanghai have adopted some measures to prevent OP. In the past 10 years, the life expectancy of the elderly in Shanghai increases over year. In the present study, the epidemiological characteristics of OP were investigated in the old people of community health service centers in Shanghai, aiming to understand the current knowledge, prevalence and treatment of OP in Shanghai.
Methods
General information
A total of 565 subjects no younger than 70 years were randomly recruited from four Community Health Centers (Yuyuan Community Health Center in Huangpu District, Laoximen Community Health Center in Huangpu District, Wusong Community Health Center in Baoshan District and Youyi Community Health Center in Boashan District) between Jul 2017 and Dec 2018. The inclusion criteria were as follows: (I) permanent residents of the local community; (II) no younger than 70 years; (III) normal ideation; (IV) cooperation with this study. Exclusion criteria were as follows: (I) severe heart, liver or renal dysfunction; (II) diagnosed with OP secondary to other diseases such as diabetes and hyperparathyroidism; (III) senile dementia or severe mental and neurological disease; (IV) a history of violent or pathological fractures. The project was authorized by the ethical committees of the Chinese Clinical Trial Registry, the number of the approval: ChiECRCT20190088. Informed consent was obtained from all the subjects before taking part. The general characteristics, BMD, history of treatment for OP, awareness rate of OP, prevalence of OP and treatment rate of OP were recorded.
Detection of BMD
Dual energy X-ray BMD detector (Hologc Discovery, USA) was employed to detect the BMD of the proximal femur and lumbar vertebrae at the anterior-posterior position. The BMD and T values were obtained: (I) T ≥−1.0, normal; (II) −2.5< T <−1.0, reduced bone mass; (III) T ≤−2.5, OP.
Assessment of activity of daily living
The activity of daily living (ADL) scale (2) was employed to assess the activity of daily living. The ADLs include daily self-care activities such as eating, dressing, bathing and toileting and mobility activities such as, transferring between the bed and a chair. The difficulty in performing these activities is classified into four grades (0, 5, 10 and 15): (I) >60, normal self-care activity; (II) 41–60, help requirement in the self-care activity; (III) 20–40, greatly depending on help in self-care activity; (IV) <20, functional defects) and the total score was 100.
Nutritional assessment
The mini nutritional assessment short-form (MNA-SF) (3) was used to assess the change in recent diet, the change in body weight within prior 3 months, physical performance, stress and acute disease, neuropsychiatric disease, body mass index (BMI) and calf circumference (CC), and the resultant scores were divided into favorable nutritional status (≥24) and malnutrition (<24).
Detection of BTM
Fasting blood was collected from these subjects into a tube without any anticoagulant. 30 min later, the blood was centrifuged at 3,500 rpm/min for 10 min, and the serum was harvested. The contents of P1NP, β-CTX, N-MID and 25OHD in the serum were detected with an automatic electrochemiluminescence immunoassay analyzer (E601; Roche) and corresponding reagents.
Statistical analysis
Statistical analysis was done with SPSS version 21.0. Quantitative data are expressed as mean ± standard deviation (), and qualitative data as number or percentage. Comparisons between two groups were done with independent sample t test or Chi square test. A value of P<0.05 was considered statistically significant. Multivariable analysis was done with Logistic regression analysis, and Pearson analysis was employed to assess the relationship between BTMs and BMD.
Results
General characteristics
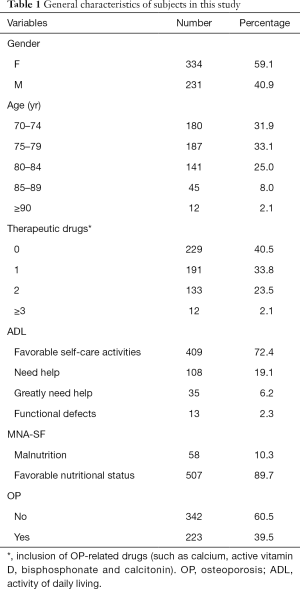
Among these 565 subjects, there were 231 males and 334 females with a mean age of 81.2±6.8 years (range, 70–95 years). The awareness rate was 89.7% (507/565). Based on the BMD, 223 subjects were diagnosed with OP and the prevalence of OP was 39.5%. In addition, 336 subjects received treatment for OP (59.5%). According to the ADL scores, serious functional defects was noted in 13 subjects (2.3%), 35 subjects greatly needed help in the self-care activities (6.2%), 108 subjects needed help in the self-care activities (19.1%) and 409 subjects had favorable self-care activities (72.4%). Favorable nutritional status was noted in 507 subjects and malnutrition was found in 58 subjects (Table 1).
Full table
Correlation between ADL and OP
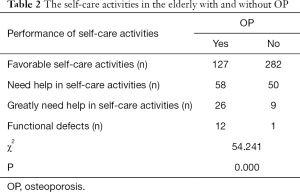
The prevalence of OP was significantly different among the elderly with different self-care activities (χ2=54.241, P=0.000) (Table 2).
Full table
Correlation between MNA-SF and OP
The prevalence of OP was markedly different between the malnutrition people and the people with good nutritional status (Table 3).

Full table
Risk factors of OP
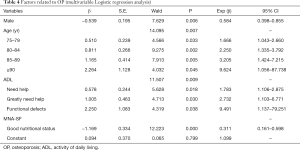
OP was used as a dependent variable, and gender, age, ADL score, and MNA-SF as independent variables for Logistic regression analysis of risk factors of OP with α=0.05. Results showed male gender and good nutritional status were independent protective factors of OP and advancing age and poor self-care activities were independent risk factors of OP (Table 4).
Full table
BTM in the elderly with and without OP
The β-CTX level in OP group was significantly higher than in non-OP group (t=6.81, P<0.05). The levels of P1NP, N-MID and 25OHD in the OP group were significantly lower than in the non-OP group (t=−5.21, −9.64 and −8.90; P<0.05) (Table 5).

Full table
Correlation between BTM and BMD
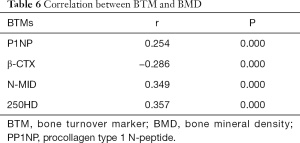
Pearson analysis showed β-CTX level was negatively related to the BMD (r=−0.286, P=0.000) and the levels of P1NP, N-MID and 25OHD were positively related to the BMD (r=0.254, 0.349 and 0.357, P<0.05) (Table 6).
Full table
Discussion
Our results showed the awareness rate of OP was 89.7% in the elderly aged 70 or older, which was significantly higher than previously reported (50.9%) (4); the prevalence of OP was 39.5%, which was similar to previously reported (4). In addition, the treatment rate of OP was 59.5%, which was significantly higher than 20% reported by Bian et al. (5). These may be ascribed to the routine and regular health education in the communities of Shanghai and the increased education level.
Li et al. (6) found the prevalence of OP was comparable between males and females, but Zhang et al. (7) reported that the prevalence of OP in females was higher than in males of the same age group. It is indicated that the controversy about the influence of gender on prevalence of OP. In the present study, multivariate logistic regression analysis showed the prevalence of OP in females increased as compared to males (P=0.006, OR =0.584), suggesting that female gender is an independent risk factor of OP in the elderly. This may be related to the reduction of estrogen after menopause in females. In addition, the risk for OP in the elderly aged 75–79 years (P=0.033, OR =1.666), 80–84 years (P=0.002, OR =2.250), 85–89 years (P=0.005, OR =3.205) and ≥90 years (P=0.045, OR =9.624) increased as compared to the elderly aged 70–74 years, suggesting that the advancing age is also a risk factor of OP, which was consistent with the results of Mathieu et al. (8), who reported that the decreases in sex hormone and bone formation over age were associated with OP (9). At the same time, our study also showed the risk of OP in the elderly who need help, greatly need help or have functional defects, was 1.783, 2.732 and 9.491 times of that in the elderly with favorable self-care activities, which was consistent with the result reported by Chen et al. (10). Studies have shown that the time and intensity of exercise will decrease with the decline of ADL in the elderly, and the appropriate weight-bearing and resistance exercise is beneficial to promote bone formation, reduce bone loss and avoid fragility fractures, and exercise is positively related to BMD (11,12). The BMD reduces with the reductions in the time and intensity of exercise, resulting in OP. The reduction in the ADL may decline the time and intensity of exercise, and therefore reduces the BMD. The elderly with good nutritional status had lower risk of OP than those with malnutrition (P=0.000, OR =0.311), indicating that the better the nutritional status, the less likely the OP is, which is similar to the results reported by Heaney et al. (13). The prevalence of OP in the elderly increases with the decrease in the nutritional status, which may be ascribed to the decreased protein intake, vitamin D reduction and calcium deficiency (14). In the present study, participants were confined to the outpatients in the Community Health Service Centers, and thus there might be bias in the composition of subjects recruited; the intake of protein, vitamin D and calcium was not determined and thus we could not determine the relationship of them with the risk for OP. Further studies are needed to classify the role of different nutrients in the pathogenesis of OP.
The organic components of the bone are mainly composed of type I collagen (about 90%), bone binding protein (about 10%) and other trace proteins (15). After adulthood, the bone growth stops, but cellular activity (bone reconstruction) continues; there are still bone formation and resorption, which remains at a dynamic equilibrium. However, menopause and certain pathological processes may increase the bone resorption, leading to OP. BTMs reflect the functions of osteoblasts and osteoclasts. It has been confirmed that the compromised bone formation is the main cause of OP in the elderly (16). The bone metabolism in the elderly shows low-turnover, the bone formation and resorption are low, and the bone formation is significantly lower than the bone resorption.
At present, the BMD measured by the dual-energy X-ray absorptiometry is recognized by the international academic community as the gold standard for diagnosis of OP (17). However, X-ray bone absorptiometry has some disadvantages, such as radioactivity; the BMD values detected are affected by the instruments used for the measurement; the cost is relatively high; change in BMD is relatively lagging, and increase of bone density will be observed at about 2 years after anti-OP treatment. Clinically, the increase in fracture risk is not always associated with the reduction in BMD, and BTMs have a good correlation with fracture risk (18), which can compensate for the disadvantages of BMD detection. The detection of BTMs has following advantages: the changes in BTMs after anti-absorption therapy can predict the risk for fracture (19); the changes in BTMs precede the change in BMD (20); BTMs can provide information about the therapeutic efficacy at about 3 months after anti-OP treatment (21); the detection is simple, easy, and acceptable.
In the organic components of bone matrix, type I collagen is synthesized by the osteoblasts. The N-terminal and C-terminal extensions of type I collagen are removed by special proteases, forming bone matrix. The N-terminal is P1NP. When the activity of osteoblasts is enhanced, the synthesis of procollagen increases, and the blood concentration of P1NP increases. The blood P1NP concentration may reflect the ability of osteoblasts to synthesize collagen, which is the basis for the assessment of osteoblast activity and bone formation (22,23). Our study showed that P1NP was significantly lower in the OP group than in the non-OP group, suggesting that elderly patients with OP had lower bone formation than the elderly without OP. In addition, BMD was positive related to P1NP, indicating that the reduction of BMD in the elderly is related to the reduction of bone formation.
β-CTX is a degradation product of type I collagen C-terminal peptide and is one of the most valuable markers for the assessment of osteoclast activity and bone resorption (24,25). Increased serum β-CTX indicates the increased bone resorption. Our study showed that β-CTX was elevated significantly in the OP group as compared to non-OP group. It is suggested that the bone resorption in elderly with OP is more evident than in those without OP. Moreover, there’s a negative correlation between BMD and β-CTX, indicating that the decreased BMD in the elderly is related to the increased bone resorption. In the present study, we focused on the increased bone resorption in the OP elderly compared with non-OP elderly, and self-control was employed, which will be improved in our future studies.
Osteocalcin is a non-collagen bone matrix protein secreted by mature osteoblasts, and accounts for 25% of non-collagen components in the bone matrix and 2% of total bone protein. The serum osteocalcin is diverse in the form: about 1/3 is intact osteocalcin (i.e., full-length osteocalcin), 1/3 is N-terminal moderate molecular (N-MID) fragment of osteocalcin and 1/3 is short peptide. Due to the poor stability of the full-length osteocalcin, the temperature and time of storage will affect the experimental results. Therefore, serum N-MID is generally measured in clinical practice. Detection of N-MID is simple and rapid, and N-MID is also a specific biochemical indicator of bone formation. Our study showed N-MID level was significantly lower in the OP group than in the non-OP group, suggesting the elderly with OP have lower bone formation than the non-OP elderly. In addition, BMD is positively related to N-MID, indicating that the reduction of BMD in the elderly is related to the reduction of bone formation.
The blood levels of biochemical indicators reflecting bone formation in our study were lower in the OP group than in the non-OP group, and the biochemical indicators reflecting bone resorption were higher in the OP group than in the non-OP group. In other words, the indicators reflecting bone formation reduced gradually but those reflecting the bone absorption increased gradually with the deterioration of OP, indicating the shift of bone reconstruction balance to a negative equilibrium. With the increase of age, the bone resorption is faster than the bone formation, and the bone reconstruction is in a negative balance, resulting in a gradual decrease in the bone mass and subsequent OP (26). BMD together with biochemical indicators of bone metabolism is better to reflect the bone state, and plays an important role in clinically guiding the targeted anti-OP treatment.
In patients with primary OP, there are dysfunction of vitamin D production and metabolism, resulting in a decrease in the active vitamin D. Although vitamin D does not directly reflect the activity of osteoblasts or osteoclasts, an in vitro study reported that vitamin D was able to promote the differentiation and maturation of precursor cells into osteoblast, induce the synthesis of osteocalcin in the osteoblasts, enhance alkaline phosphatase activity, and promote collagen production and insulin-like growth factors (25). In the present study, the blood 25OHD was significantly reduced in the OP group compared with the non-OP group, and the BMD was positively related to blood 25OHD, indicating that the decreased BMD in the elderly is associated with decreased bone formation.
In summary, female gender, advancing age, malnutrition, and poor self-care activities in daily living are independent risk factors of OP. To strengthen the community health education, increase nutrition intake and improve the self-care activities may be employed to prevent the occurrence of OP. In addition, P1NP, β-CTX, N-MID, 250HD and BMD are related to the BMD, and can reflect the balance between osteoblast function and osteoclast function. BMD together with BMD can be used to comprehensively assess the state of bone health, which is important for early identification of senile OP, guiding the clinical use of anti-OP treatment and monitoring of therapeutic efficacy.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The project was authorized by the ethical committees of the Chinese Clinical Trial Registry, the number of the approval: ChiECRCT20190088. Informed consent was obtained from all the subjects before taking part.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Consensus development conference. diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 1993;94:646-50. [Crossref] [PubMed]
- Ma ZH, Zhang RY, Wan BZ. Application and Practice of PBL in Nursing: Case Analysis. Chinese Nursing Association 1999;34:615.
- Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin Geriatr Med 2002;18:737-57. [Crossref] [PubMed]
- Wang ZF. Investigation on the status and contributing factors of adult chronic diseases in large general hospitals. 2017.
- Bian PD, Shou ZX, Ying QF, et al. Current status of drug treatment of osteoporosis in elderly men. Chinese Journal of Osteoporosis 2016;22:1466-8.
- Li C, Lv WH, Wang TT, et al. The study of prevalence of osteoporosis in 1088 medical workers. Chinese Journal of Osteoporosis 2015:1217-20.
- Zhang W, Wang B, Zhang LL, et al. Correlation between femoral head bone iron content, serum ferritin and bone mineral density of postmenopausal women with femoral neck fragility fracture. Chinese Journal of Orthopaedics 2014;34:39-47.
- Mathieu C, van Etten E, Decallonne B, et al. Vitamin D and 1,25-dihydroxyvitamin D3 as modulators in the immune system. J Steroid Biochem Mol Biol 2004;89-90:449-52. [Crossref] [PubMed]
- Clarke BL, Ebeling PR, Jones JD, et al. Predictors of bone mineral density in aging healthy men varies by skeletal site. Calcif Tissue Int 2002;70:137-45. [Crossref] [PubMed]
- Chen WW, Qian XZ, Chen Y, et al. Research of the risk factors of osteoporosis in more than 60 years old elderly people in Songnan Town, Baoshan District, Shanghai. Chinese Journal of Osteoporosis 2018;24:1493-7.
- Andreoli A, Celi M, Volpe SL, et al. Long-term effect of exercise on bone mineral density and body composition in post-menopausal ex-elite athletes: a retrospective study. Eur J Clin Nutr 2012;66:69-74. [Crossref] [PubMed]
- Zhang H, Zhang G, Peng AJ, et al. Influence of Exercise Therapy Combined with Drug Intervention on the Risk of Falls in the Elderly with Osteoporosis in Aged Care Hospitals. Geriatrics & Health Care 2017;23:392-5.
- Heaney RP. Dairy and bone health. J Am Coll Nutr 2009;28 Suppl 1:82S-90S. [Crossref] [PubMed]
- Zhen D, Liu L, Guan C, et al. High prevalence of vitamin D deficiency among middle-aged and elderly individuals in northwestern China: its relationship to osteoporosis and lifestyle factors. Bone 2015;71:1-6. [Crossref] [PubMed]
- Tan ZL, Ren HL, Bai RX, et al. Osteoporosis and biochemical indicators of bone metabolism. Chinese journal of Osteoporosis 2006;12:89-93.
- Halvarsson A, Franzen E, Stahle A. Assessing the relative and absolute reliability of the Falls Efficacy Scale-International questionnaire in elderly individuals with increased fall risk and the questionnaire's convergent validity in elderly women with osteoporosis. Osteoporos Int 2013;24:1853-8. [Crossref] [PubMed]
- Osteoporosis and Bone Mineral Disease Branch of Chinese Medical Association. Diagnosis and treatment of primary Osteoporosis (2011). Beijing: People’s Health Publishing House, 2011;3.
- Cummings SR, Karpf DB, Harris F, et al. Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med 2002;112:281-9. [Crossref] [PubMed]
- Wu XY, Wu XP, Liao EY. Bone turnover markers and bone mineral density monitoring therapy osteoporosis and their relationship with fracture. Chinese Journal of Osteoporosis 2007;13:797-802.
- Garnero P, Sornay-Rendu E, Duboeuf F, et al. Markers of bone turnover predict postmenopausal forearm bone loss over 4 years: the OFELY study. J Bone Miner Res 1999;14:1614-21. [Crossref] [PubMed]
- Guo HF. Correlation between bone metabolism markers and senile osteoporosis. Chinese Journal of Medical Guide 2011;13:1710-2.
- Xie QP, Ye DX, Wen HK, et al. Relationship between the changes of biochemical markes of bone turnover and osteoporosis in male patients with type 2 diabetes. Chinese Journal of Clinical Laboratory Management (Electronic Edition) 2014:51-4.
- Koivula MK, Risteli L, Risteli J. Measurement of aminoterminal propeptide of type I procollagen (PINP) in serum. Clin Biochem 2012;45:920-7. [Crossref] [PubMed]
- Srivastava AK, MacFarlane G, Srivastava VP, et al. A new monoclonal antibody ELISA for detection and characterization of C-telopeptide fragments of type I collagen in urine. Calcif Tissue Int 2001;69:327-36. [Crossref] [PubMed]
- Filip RS, Zagórski J. Age- and BMD-related differences in biochemical markers of bone metabolism in rural and urban women from Lublin Region, Poland. Ann Agric Environ Med 2004;11:255-9. [PubMed]
- Sosa M, Lainez P, Arbelo A, et al. The effect of 25-dihydroxyvitamin D on the bone mineral metabolism of elderly women with hip fracture. Rheumatology (Oxford) 2000;39:1263-8. [Crossref] [PubMed]


