
Risk factors of difficult cases of deliberate postoperative hypotension after endovascular embolization in patients with brain arteriovenous malformation
Introduction
Endovascular embolization is a major treatment option of brain arteriovenous malformations (bAVM), alone or followed by surgical resection (1-3). Post-operative hemorrhage remains a life-threatening complication in patients undergoing surgical treatment due to normal perfusion pressure breakthrough, venous occlusive hyperemia, rupture of small feeding arteries, and rupture of residual AVM nidus (4-7). Uncontrolled post-operative high blood pressure (BP) may induce the above bleeding causes. There’s evidence suggesting a benefit from lowering the BP below normal for patients after AVM surgery (8). Therefore, deliberate employment of post-operative hypotension was widely recommended by neurosurgeons. But the ideal target BP was still under debate (9,10). The systolic blood pressure (SBP) of patients undergoing AVM embolization or microsurgery are routinely kept below normal (100–120 mmHg) (11).
In clinical observation, however, BP control to the aimed target is difficult in some cases and risk factors remain unclear. This study aimed to analyze the potential risk factors of difficult cases of deliberate postoperative hypotension.
Methods
Patients
All patients with bAVM between January 2010 and December 2015 were reviewed for this study. Patients were included into the database if they were confirmed to have a bAVM and underwent endovascular embolization in The First Affiliated Hospital, Sun Yat-sen University. Patient’s medical records, operative reports, radiographic images, and detailed AVM associated database were reviewed. Following factors were recorded: demographic features, clinical presentation, AVM characteristics, peri-operative medication, hemodynamic data, treatment-related information and outcome-related data. For those who underwent more than one treatment procedure, we selected the first one to analyze. Patients with recurrent AVMs, with previous embolization, surgical resection or radiotherapy were excluded.
Management of brain AVM patients
A multi-disciplinary team of cerebrovascular neurosurgeons, interventional neurosurgeons, neurological physicians and anesthesiologists evaluated each brain AVM patient and determined the optimal treatment modality or combination of modalities for the goal of complete AVM obliteration while minimizing risks. Standard endovascular techniques were applied for embolization. Endovascular embolization was performed as an adjunct to microsurgical resection or used alone for complete AVM nidus obliteration.
Commencing with surgery, each patient’s SBP was limited to 100–120 mmHg (10–15 mmHg lower than basic condition). An escalating drug regimen was used to achieve the target BP. The regimen included oral beta-blockers, oral ACEI, intravenous alpha adrenergic agents (Urapidil hydrochloride), intravenous calcium channel blockade (CCB, Nicardipine), nitroglycerin, or sodium nitroprusside.
Intra-operative medication was determined by the current senior anesthesiologists, and extubation was performed in operation room (OR) or intensive care unit (ICU) according to doctors’ decision prior surgery.
Anticonvulsants were commenced after surgery to reduce the potential of seizures as well seizure-related increases in BP.
The detailed post-operative information was recorded on medical records by nurses, including vomiting, headache, hemodynamic information and medication.
Outcome measures
BP of the first 24 hours after operation was recorded. All patients met target BP with or without medication. Difficult cases of deliberate employment for postoperative hypotension was determined as the following situation any time in the first 24 hours after embolization: (I) ineffectiveness of oral hypotensive medication or single bolus of Urapidil (12.5–25 mg), and (II) need of continuous urapidil administration or multiple intravenous hypotensive drugs.
Statistical analysis
Statistical analysis was performed using SPSS (Version 23.0 for windows; SPSS, Inc., Chicago, IL). We analyzed patient age, gender, ruptured at presence, clinical presentation, pre-operative electrocardiogram, history of hypertension, high BP on admission, Glasgow Outcome Score (GOS), AVM location, Sptzler-Martin (S-M) grade, extubation, intra-operative medication, post-operative headache and vomiting, and post-operative analgesics. Univariate tests (chi-square test, or Fisher’s exact test, when appropriate) to describe the risk factors on uncontrolled post-operative BP. When P value smaller than 0.2, data was included in Binary logistic regression to find the independent risk factors. Data were reported as mean ± SD, median (quartile), or frequency (percentage) as appropriate. Statistical significance was indicated at 0.05 level.
Results
Overall results
Four hundred and eighty-five patients with bAVM from January 2010 to December 2015 were evaluated, of which 205 underwent conservative treatment, 78 underwent microsurgical resection merely, 8 were admitted in hospital for other diseases, 12 patients were diagnosed as AVM after surgery. A total of 182 patients were enrolled for analysis. Of the 182 patients, there was a male predominance (n=115, 63.19%), and the mean age at the time of admission was 29.54±12.50 years.
Of the 182 patients, 86 (47.25%) were admitted with ruptured AVM. Headache was the most common presentation (n=86, 47.25%). Thirty-seven (20.33%), 32 (17.58%) and 26 (14.29%) patients presented as neurological deficit, syncope and seizures, respectively.
Ninety-four patients (51.65%) experienced abnormal pre-operative electrocardiograph (ECG). Two patients (1.10%) had a history of hypertension. However, 12 (6.59%) patients were observed high BP on admission (SBP >140 mmHg). The median of Glasgow Coma Score (GCS) was 15 (quartile: 15, 15), and 20 (10.99%) patients were admitted with abnormal consciousness (GCS <15). The American Society of Anesthesiologists (ASA) classification revealed that 143 of the patients meet ASA grade I–II, and only 2 persons (1.10%) had an ASA grade higher than grade III.
AVM and surgical characteristics
Amount of lower grade cAVM (S-M I–II), moderate grade (III) and higher grade (IV–V) was 69 (37.91%), 71 (39.01%) and 42 (23.08%), respectively. The median surgical duration was 65 min (quartile: 50–85 min). Of the 182 patients, 176 (96.70%) patients were extubated in OR, and the median extubation time was 10 min (quartile: 10–15 min). In the 182 patients experienced embolization, the median embolization rate was 60% (quartile: 40–80%).
Dexmedetomidine was administered in 27 patients (14.84%) intra-operatively, and nonsteroidal anti-inflammatory drugs (NSAIDs) were used in 117 patients (64.29%). Besides, in 6 patients (3.30%), pressor agents were medicated intra-operatively to maintain hemodynamics stable.
Recovery outcome
Recovery outcome are shown in Table 1. Patients’ recovery outcomes were recorded when they discharged from the hospital. Of the 182 patients, 170 (93.41%) had good or full recovery (Glasgow outcome score reached 4), and poor outcomes were observed in 12 patients (6.59%), no patient died from embolization. Eighteen (9.89%) patients experienced Moderate to significant neurological deficits after surgery (identified as a modified Rankin score reached 3).
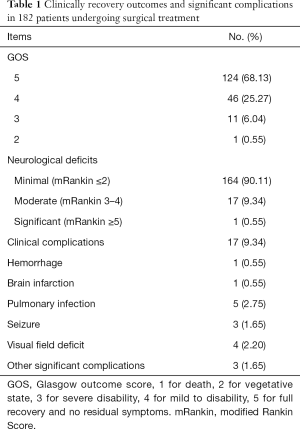
Full table
Surgery related complications were observed in 17 patients (9.34%). Delayed post-operative hemorrhage occurred in 1 (0.55%) patients. One patient suffered from brain infarction because of a dropped arterial thrombus. Seizure episodes were found in 3 patients (1.65%). Besides, pulmonary Infection was seen in 5 patients (2.75%). Furthermore, frequency of visual field deficit and other significant complications were 4 (2.20%) and 3 (1.65%), respectively. No complications resulting in reoperation happened.
Predictors of difficult cases of deliberate postoperative hypotension on the first post-operative day (POD1)
Difficulty in deliberate postoperative hypotension was observed in 75 patients (41.21%) on POD1. The univariate analysis showed that intraoperative dexmedetomidine administration and S-M grade were associated with uncontrolled BP on POD1 (all P<0.05, Table 2).
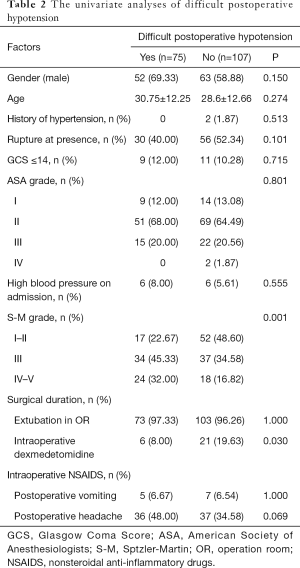
Full table
According to the determined statistic method, we included gender (P=0.150), rupture at presence (P=0.101), intraoperative dexmedetomidine (P=0.030), S-M grade (P=0.001) and headache on POD1 (P=0.069) in the logistic regression.
The logistic regression was performed and indicated that S-M grade was an independent risk factor of difficult cases of deliberate hypotension of POD1 (OR=2.058; 95% CI, 1.364–3.105; P=0.001, Table 3). What’s more, the logistic regression revealed that intraoperative Dexmedetomidine was potential independent protective factor (OR=0.356; 95% CI, 0.133–0.956; P=0.040).
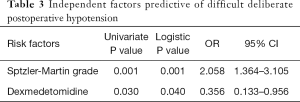
Full table
Discussion
We retrospectively reviewed the data of patients underwent endovascular embolization of bAVMs. We found that S-M grade was an independent risk factor of difficulty in postoperative deliberate hypotension. On the contrary, intra-operative dexmedetomidine administration was protective predictor on POD1.
Deliberate post-operative hypotension was widely used after bAVM treatment. However, ideal hemodynamic boundary is controversial. Introduction of intraoperative and post-operative hypotension for 3 to 5 days were proved effective in case scenario (12). In 2015, kept BP lower than normal for the patient after microsurgical resection and endovascular treatment was recommended by Andre Conger (SBP, 100–120 mmHg), which was the same as our center (11). Spetzler and colleagues, advocated the maintenance of normal BP following AVM resection, regardless of whether embolization was used preoperatively or not (13). However, Morgan strongly recommended that strict BP protocol of a maximum systolic pressure of 110 mmHg for a maximum of 7 days in cases of larger AVMs (larger than 4 cm in diameter) in 1999, in 2003 and 2016, their further studies revealed that deliberate employment of postoperative hypotension (a maximum mean arterial BP ≤70 mmHg, for a minimum of 7 days) was of great importance in patients with moderate to high grade AVMs (S-M grade III to V) (6-9).
In the present study, we kept SBP 10–15 mmHg lower than basic condition during embolization procedure. We observed one case of intra-operative hemorrhage and no patient suffered from delayed hemorrhage. Compared with the reporting data, our center showed a superiority on short-term complication. We declared a further study on long-term outcomes in the future (Table 1).
S-M grading consist of size of AVM nidus, deep vein drainage and eloquent area of brain. High S-M grade was associated with higher risk of bAVM surgery. High S-M grade AVM had larger volume of blood flow. When embolizing these AVMs, more blood flow recontributes to normal brain and cause increased intracranial hypertension, which may result in higher systematic BP. Our study revealed that BP of patients with high-SM-grade AVM was harder to control.
Dexmedetomidine was a highly selective α2-adrenoceptor agonist, and it can provide sedation, analgesia, anti-hypertensive and anxiolytic effects in surgical procedures. In the present study, we revealed that intra-operative Dexmedetomidine administration was potential independent protective factor of uncontrolled BP (P<0.05, OR<1). Moreover, we wandered whether patients benefited from persistent dexmedetomidine following surgery. And further investigation would focus on e long-term outcomes of dexmedetomidine administration in bAVM patients.
We found a trend of association between post-operative headache and difficult deliberate postoperative hypotension (P=0.069). About 50% patients harbored headache when admitted in hospital. Regional hemodynamics change and metabolism of embolism materials also contributed to post-operative pain. In the present study, post-operative headache in patients underwent endovascular embolization had a rate of 40.1% (73 persons in total) on POD1, which was underestimated. We administrated extra analgesics only if patients argued and visual analogue score reached 5. The previous literature also indicated that pain management played important role in better outcome after neurosurgery. We appealed a further study to find the normative post-operative pain management after neurosurgery in the future.
Limitation of this study. We filtrated 182 patients to perform univariate analysis, and we analyzed parameters of P value <0.2 using binary logistic regression. There was risks of omitting potential predictors. Large sample sized research was needed.
Conclusions
We found that higher S-M grade was an independent risk factor of difficult cases of deliberate employment for postoperative hypotension following embolization. Intra-operative Dexmedetomidine administration was potential protective factor. Further studies on adequate post-operative analgesia are of great significance for these selective patients.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional human ethics committee of First Affiliated hospital, Sun Yat-sen University (Guangzhou, China; reference number [2016]206), and it was performed in accordance with institutional ethics committee guidelines.
References
- Blauwblomme T, Bourgeois M, Meyer P, et al. Long-term outcome of 106 consecutive pediatric ruptured brain arteriovenous malformations after combined treatment. Stroke 2014;45:1664-71. [Crossref] [PubMed]
- Andrews BT, Wilson CB. Staged treatment of arteriovenous malformations of the brain. Neurosurgery 1987;21:314-23. [Crossref] [PubMed]
- Hartmann A, Mast H, Mohr JP, et al. Determinants of staged endovascular and surgical treatment outcome of brain arteriovenous malformations. Stroke 2005;36:2431-5. [Crossref] [PubMed]
- Spetzler RF, Wilson CB, Weinstein P, et al. Normal perfusion pressure breakthrough theory. Clin Neurosurg 1978;25:651-72. [Crossref] [PubMed]
- al-Rodhan NR, Sundt TM Jr, Piepgras DG, et al. Occlusive hyperemia: a theory for the hemodynamic complications following resection of intracerebral arteriovenous malformations. J Neurosurg 1993;78:167-75. [Crossref] [PubMed]
- Morgan MK, Johnston IH, Hallinan JM, et al. Complications of surgery for arteriovenous malformations of the brain. J Neurosurg 1993;78:176-82. [Crossref] [PubMed]
- Morgan MK, Winder M, Little NS, et al. Delayed hemorrhage following resection of an arteriovenous malformation in the brain. J Neurosurg 2003;99:967-71. [Crossref] [PubMed]
- Morgan MK, Winder M, Little NS, et al. Delayed hemorrhage following resection of an arteriovenous malformation in the brain. J Neurosurg 2003;99:967-71. [Crossref] [PubMed]
- Morgan MK, Wiedmann MKH, Assaad NNA, et al. Deliberate employment of postoperative hypotension for brain arteriovenous malformation surgery and the incidence of delayed postoperative hemorrhage: a prospective cohort study. J Neurosurg 2017;127:1025-40. [Crossref] [PubMed]
- Fu C, Yu W, Feng Z, et al. Surgical Resection of a Progressive Giant Arteriovenous Malformation After 13-year Follow-Up. Medicine (Baltimore) 2015;94:e1076. [Crossref] [PubMed]
- Conger A, Kulwin C, Lawton MT, et al. Endovascular and microsurgical treatment of cerebral arteriovenous malformations: Current recommendations. Surg Neurol Int 2015;6:39. [Crossref] [PubMed]
- Day AL, Friedman WA, Sypert GW, et al. Successful treatment of the normal perfusion pressure breakthrough syndrome. Neurosurgery 1982;11:625-30. [Crossref] [PubMed]
- Rangel-Castilla L, Spetzler RF, Nakaji P. Normal perfusion pressure breakthrough theory: a reappraisal after 35 years. Neurosurg Rev 2015;38:399-404; discussion 404-5. [Crossref] [PubMed]


