
Patient-doctor concordance of perceived mental health service needs in Chinese hospitalized patients: a cross-sectional study
Introduction
The prevalence of emotional disorders is high among people who seek help from general medical services. In most international studies, the prevalence of depression and anxiety ranges from 3.6% to 13.1% (1-3). Co-morbid emotional problems such as depression and anxiety are associated with a decreased quality of life, impaired self-management behaviors, and a diminished perception of disease control in medical patients (4).
Unfortunately, most of the patients with emotional problems are not properly treated. For example, an investigation of the Epidemiology of Mental Disorders (ESEMeD) of 21,400 adults from six European countries indicated that the lifetime prevalence of major depression was 13.4%, but only 4.6% of the depressive patients accepted antidepressants treatment (5).
In our opinion, there are two reasons why detection and treatment rates for emotional problems are so low: the medical staff and the patients themselves. When paying attention to the doctors’ role in detecting a mental disorder and providing treatment for patients with clinically significant depression, studies found that only half of the patients with clinically significant depression were recognized by their physicians in charge (6,7). Additionally, the physicians’ assessment of the needs of their patients regarding mental health services is not always correct (8). In 2009, Mitchell et al. reviewed 41 studies about the recognition of depression with a total of 50,371 patients and found that the correct recognition rate was 47.3% and out of these, only 33.6% were recorded in patient files. In addition, within the complete group of all the patients diagnosed with depression, the misdiagnosis rate was nearly 20% (9).
Doctors play an important role in identifying and preventing mental distress by providing adequate information and basic emotional support to patients. However, only the minority of patients with mental problems receive timely and proper treatment even when they are correctly recognized. Hansen et al. found that about 50% of internal medical inpatients with a co-morbid psychiatric disease were correctly evaluated by medical doctors and nurses, and that only about 20% of them obtained mental health treatment (10).
Pasacreta and Massie reported that, even in the patients who perceived their symptoms as requiring a psychiatric consultation, only 13% actually received psychiatric help (11). Maguire et al. found that only 15% to 50% of patients with cancer requiring a psychiatric intervention actually obtained mental health services such as supportive consultations (12,13). In 2009, data from a large scale epidemiology survey in China led by Phillips et al. suggested that among individuals with a diagnosable mental illness, only 5% had ever seen a mental health professional (14).
The other important reason why inpatients do not receive mental health care may be the absence of perceived needs for psychological care by the patients themselves. Patient expectations of their need for psychological care have been extensively studied. Seekles reported that, in 762 primary care patients who had been diagnosed with depression or/and anxiety disorders, only 55.3% believed that they needed mental health care (15). Prins reported that 87.1% of the 622 primary care patients with a current (within the past 6 months) diagnosis of depression and/or anxiety disorder expressed their need for any type of psychological services, such as practical support, skill training, consultation/psychotherapy (16). In 2001, Wisely asked burn-injured patients what additional help they wanted. Patients were given a list of options, including support groups, individual mental treatment or consultation, written information, and other desired options. One or more options could be selected. Of these patients, 38.6% reported that they would like to have received some written information about the emotional difficulties which could be expected after a burn injury. A further 36.4% felt that they would benefit from individual psychological interventions (17). Hodgkinson et al. (18) found a high percentage (86%) of reported unmet needs in breast cancer survivors and a significantly higher percentage in those patients with high levels of anxiety or depression. Given the widespread range and high proportion of patients who have unmet needs, it is important and necessary to pay more attention to this problem and solve it.
Moreover, we believe that a high concordance in the assessment of psychological needs rated by patients and medical staff is another important precondition for an adequate treatment of patients with depression or anxiety. However, it has been shown that doctor and patient attitudes relating to mental health services are not always consistent (19,20). Richards et al. reported that 37% and 12% of patients with psoriasis were identified as probable clinical cases for anxiety disorder and depression respectively. Dermatologists identified only 39% of the patients with significant psychological difficulties during the consultation. The level of concordance between patients’ ratings and dermatologists’ ratings regarding the presence of anxiety or depression was low (kappa values of 0.24 and 0.26 respectively) (21).
The concordance between patients and doctors on perceived needs for mental health services has not been broadly studied before. Therefore, our study aimed to assess the concordance of perceived psychological needs between patients and doctors in China and to identify the social demographic factors of both patients and doctors that may influence the concordance. Here, we also summarize and recommend some methods for medical staff to ensure that patients receive appropriate treatment for their mental problems.
Methods
Research design and sampling
This cross-sectional survey was approved by the Ethics Committee of West China Hospital of Sichuan University and was conducted from October to November, 2013. Participants in this study were inpatients recruited from 10 voluntary departments (Oncology, Internal Cardiology, Respiratory Medicine, Rehabilitation, Geriatrics and Gerontology, General Practice, Pain Management, Rheumatology, Hepatic Surgery, and Thyroid and Breast Surgery) of West China Hospital, a major tertiary general hospital in Chengdu, China. All hospitalized patients of the listed departments were selected as potential participants. The following inclusion criteria were applied: (I) all inpatients from the selected departments with (II) junior middle school education and above who (III) had been given informed consent to participate in the study. Patients who met all these criteria were included in our research. The exclusion criteria were as follows: (I) patients who were discharged from the hospital on the day of the survey; and (II) patients who were unable to finish the self-report questionnaire on their own due to a serious physical condition or very poor mental health status.
Instruments and measures
Demographic questionnaire
We designed and gave participants a demographic questionnaire of demographic information including patients’ gender, marital status, ethnic origin, smoking status, alcohol drinking habits, educational background, and annual household income. In addition, we asked doctors for their gender, years of working experience, and educational background.
Patient Health Questionnaire-9 (PHQ-9)
PHQ-9 is a 9-item questionnaire focusing on depression. The PHQ-9 total score ranges from 0 to 27 and a score ≥10 was used as the cutoff point for clinically significant depression in the present study (22). The PHQ-9 is a reliable and valid scale used to evaluate depressive symptoms both in the general population and in clinical samples (23). Previous studies have shown that the PHQ-9 has good reliability and validity to screen depression in Chinese outpatients in general hospitals (24). In addition, a cutoff value of 10 has been shown to be optimal (24).
Generalized Anxiety Disorder 7-item scale (GAD-7)
The GAD-7 was used to evaluate symptoms of anxiety, which has been shown to have a satisfying sensitivity and specificity as a screening instrument for panic, social anxiety, post-traumatic stress disorder, and generalized anxiety disorder (25). GAD-7 scores range from 0 to 21, and a score ≥10 also represents clinically significant anxiety in the present study (26). The Chinese GAD-7 with the cutoff value of 10 has been validated in general medical outpatients to detect GAD (27).
Investigation of patients’ mental health service needs
Patients were asked to answer one query: “Do you think that you require any professional mental health services? Yes/No” This way of investigating patients’ mental health service needs is simple and time-saving and was therefore used to minimize the false-negative responses and the non-response rate.
Doctors’ evaluation of patients’ mental health service needs
All doctors in this survey were in charge of the individual patients and knew the patient's condition well. In most cases, one doctor was in charge of 3 to 4 patients. The question “Do you think that the patient requires any mental health services?” with a dichotomous answering format of “yes” or “no” was given to the doctors.
Interviewing and data collection
The investigation panel was composed of 22 nurses from the 10 departments listed above. Due to the familiarity and good relations between the nurses and the patients, the false-negative responses and the non-response rates were thought to be minimized. The investigation panel participated in a 2-day training program focusing on the questionnaires and practicing conducting the interviews. Before the study began, a pilot investigation was carried out in the departments of Thyroid and Breast Surgery, Oncology, and Pain Management. The pilot research showed that the questionnaire was feasible and understandable to the hospitalized patients. The response rate was high in the pilot study. In the final sample, all the questionnaires were completed by the included patients themselves and their responsible doctors under the supervision of the nurses. These nurses explained the research questions and the proper use of the questionnaire. Informed consent was obtained at the beginning of every interview. After the patient had completed the questionnaire, the interviewer checked the questionnaires for completeness to minimize the number of missing items.
Ethical
Written informed consent was obtained from all participants before every interview. The study was approved by the Ethics Committee of West China Hospital of Sichuan University.
Data analysis
Descriptive statistics were used to describe the sociodemographic variables of the sample. Chi-square tests were used to analyze the differences in the mental health needs between the patients with significant emotional problems and the patients without significant emotional problems. The concordance rate between the patients’ needs and doctors’ evaluation was measured using kappa statistics. A logistic regression was conducted to find the potential influencing factors of the concordance rate. SPSS 19.0 was used for data analysis and the statistical significance was set at P<0.05 based on two-tailed tests.
Results
Participants
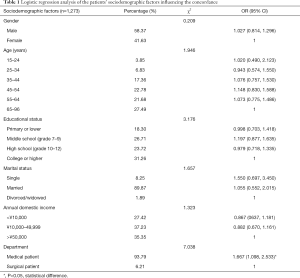
From the 1,662 hospitalized patients which could be approached at the 10 departments that day, 151 patients were excluded based on the exclusion criteria. Among the included 1,511 hospitalized patients, 149 patients refused to participate in the study with “lack of time” and “not interested” as the most common reasons; 89 participants were excluded because their doctors did not respond. The overall response rate was 84.25% and the final sample consisted of 1,273 participants. The sociodemographic characteristics of the study group are reported in Table 1. The mean (SD) age was 53.1±16.3 years; 58.37% of the sample were men (n=743).
Full table
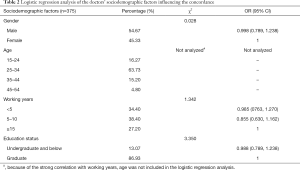
In this study, 375 doctors were included. The mean (SD) age was 31.85±6.78 years (Table 2).
Full table
The patients’ mental health service needs evaluated by patients and their doctors
We divided the patients into two groups: those with scores from the PHQ-9 or GAD-7 above or equal to 10 were placed in the significant depression or anxiety group, while those with scores from the PHQ-9 and GAD-7 below 10 were placed in the without significant depression or anxiety group.
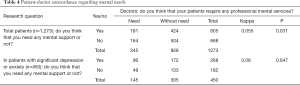
In total, 605 of the 1,273 (47.53%) patients believed that they needed mental health help: the proportion of patients who actually reported having significant depression or anxiety according to PHQ-9 and GAD-7 was 59.56% (268 out of 450) and 40.95% (337 out 823), respectively (Table 3).

Full table
According to the results from the doctors, only 345 out of the 1,273 (27.10%) patients were in need of mental health services: the rate in patients with or without significant depression or anxiety scores was 32.22% (145 out of 450) and 24.30% (200 out of 823), respectively (Table 3).
The doctors’ recognized present mental distress in 60.33% (768 out of 1,273) of the cases (Table 3).
The patient-doctor concordance on the perceived mental needs of patients
Kappa statistics were used to analyze the patient-doctor concordance rate on perceived psychological needs of patients. The analysis result showed that the concordance rate between patients and doctors regarding mental needs can be considered as low in either the total patients (kappa =0.055) or the patients who had significant emotional problems according to PHQ-9 and GAD-7 (kappa =0.080) (Table 4).
Full table
Logistic regression analysis
To determine the predictors of patient-doctor concordance on mental needs, we included the years of working experience, gender, and education status of doctors, and the gender, age, educational status, marital status, annual domestic income, and wards of patients in a logistic regression analysis. We defined successful recognition as 1 (including patients with or without obvious emotional problems) versus a misrecognition as 0. The wards of patients was related to the consistent recognition rate (OR =1.667) (Tables 1 and 2).
Discussion
The ability to recognize emotional problems is believed to be one of the most important influencing factors for the proper treatment of patients with depression or anxiety. Unfortunately, patients’ and doctors’ ability to recognize distress is poor.
In this study, only 59.56% of patients with significant depression or anxiety indicated their need for psychological help. The result was similar to the results of a study from Seekles [2012] who found that just over half of patients had needs for mental health services (55.3%) (15). Prins et al. conducted a systematic review including 71 studies and found that only 49% to 84% of the patients with depression or anxiety perceived the need for treatment (28).
It is noteworthy that even in patients without significant depression or anxiety scores, 40.95% of them expressed their needs for mental health services, although the rate was markedly lower than that of the patients with actual significant depression or anxiety scores.
Moreover, more than 40% of patients with significant emotional problems thought that they did not need mental health services. There are several reasons why patients might not express their needs for mental health services. For example, patients may experience stigma when showing help-seeking behavior (29). This phenomenon may be especially common in China because some Chinese people believe that suffering from a mental disease is a taboo topic which is accompanied by guilt and shame.
In addition, personality traits were also reported as one influencing factor of the perceived needs for care. Patients with higher levels of neuroticism or higher levels of openness for new experiences are more likely to perceive that consultation is needed (15).
Seeking help for mood and/or anxiety disorders is also related to patient’s coping styles. An investigation on the role of personality traits in the strategies for coping with depressed mood indicated that people with a high score on neuroticism used more coping strategies (including seeking professional help) (30).
A systematic review (28) of the health beliefs and perceived needs of anxiety and depression patients demonstrated that younger age, being female, the presence of an affective disorder, and the comorbidity of anxiety and depressive disorders are positively associated with perceiving needs for the treatment of anxiety and depressive disorders. In addition, being divorced or widowed, having insurance coverage and having a positive attitude towards mental health care were also found to be associated with perceived needs for professional help. The youngest and oldest age groups, along with underage group patients, seemed to have the lower perceived needs for care.
We investigated the doctors’ ability to identify inpatients’ needs for mental health services. The doctors’ sensitivity in evaluating the psychological needs of patients with significant depression or anxiety was relatively low (32.22%). Similar results have been widely reported. Mitchell et al. reviewed 41 studies regarding the recognition of depression and found that the correct recognition rate of depression was 47.3% and that the misdiagnosis rate was nearly 20% in primary care physicians (9).
The doctors’ evaluation of patients’ emotional problems is important for subsequent treatment and is closely related to symptomatic improvement (31). Therefore, it is very important to explore the influencing factors on the recognition rate. After reviewing the literature, we identified some possible reasons why patients’ emotional needs are frequently overlooked by doctors. Medical staff have a noticeable tendency of underestimating the level of depressive symptoms in patients. Chew-Graham et al. found that primary care physicians stated that they were reluctant to diagnose depression in patients as they felt that the depressive symptoms were a normal reaction to environmental stressors and physical illness (32).
Discussion of the patients’ emotional problems requires time, good communication skills and sufficient knowledge about emotional problems in patients. Most of the doctors did not have the skills or expertise to deal with these problems (33).
Moreover, medical staff may refer patients for psychiatric evaluation only when the problems become acute. McDonald et al. reported that when patients had obvious symptoms, such as crying and a depressed mood, the detection of psychological needs by staff was higher (34).
The concordance between doctors’ and patients’ perception of psychological needs was low (kappa =0.055). The concordance between patients and doctors on perceived needs for psychological services has not been broadly studied before. Therefore, it is difficult to compare our results with previous research. Richards conducted a study on patients with psoriasis and found that the level of concordance between patients’ and dermatologists’ rating for the presence of anxiety or depression was also low (kappa values of 0.24 and 0.26) (21).
Logistic regression was used to find potential influencing factors of the concordance rate. However, only the wards in which the patients were treated at the time of the investigation could be identified as a reason for the discordance and this result might be not persuasive because of the low ratio (6.21%) of surgical patients. In the next study, the ward of the patient should be reasonably included and the number of surgical patients might be increased.
Possible reasons for the low concordance between the doctors’ and the patients’ perceptions are discussed below.
- Patients’ denial behavior. Patients’ denial behavior will influence whether or not patients are referred to receive mental support and hamper the identification of emotional problems by doctors.
- Time restrictions: Chinese hospitals are characterized by high out-patient turnover and heavy workloads which may hinder the identification of severe distress or patients who are poorly supported.
- Physicians’ interviewing techniques are characterized by directive and closed questions, premature advice, and the avoidance of mental issues. Such techniques could be the reason for doctors’ poor recognition of patient distress. It has been reported that doctors tended to avoid asking their patients about their feelings and the way they coped with illness because they were afraid of provoking strong emotional reactions in their patients (35).
- Communicational barriers between physicians of middle-class origin and lower-class patients have been found in several studies investigating information provision to patient (36).
We have to acknowledge some methodological shortcomings of this study. Firstly, we assessed patients’ subjective needs for mental health service with only one question and this might not be accurate enough. The assessment of mental health service needs lacks a third-party gold standard. Both patients and doctors have biased perceptions, and need an objective standard as a reference. Secondly, the sampling of this research only selected participants from one hospital for convenience, which may not reliably represent a sample of Chinese hospital staff or inpatients. Thirdly, including too many doctors in this study might have been problematic, and some of the doctors who were not concerned with patients’ mental health did not respond. In addition, many other factors, like ethnicity, which could influence the concordance, were not included in this study.
Conclusions
In this paper, we explored the concordance between Chinese patients’ perception of their own mental needs and the corresponding evaluation by doctors in charge of these inpatients. This concordance is believed to be an important factor to guarantee timely and adequate treatment. However, the concordance in this study was very low (kappa =0.055), even in patients with depression and anxiety, which is a severe problem on inpatients’ mental health. Therefore, in the future, we hope to shed some light on this topic by studying potential effective strategies to prompt this process, such as the raising of doctors’ awareness, the use of screening-instruments, and the training of health professionals.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of West China Hospital of Sichuan University (No. 2016269). The participants including patients and doctors gave their written consents to publish this study.
References
- Bener A, Al-Kazaz M, Ftouni D, et al. Diagnostic overlap of depressive, anxiety, stress and somatoform disorders in primary care. Asia Pac Psychiatry 2013;5:E29-38. [Crossref] [PubMed]
- Qin X, Phillips MR, Wang W, et al. Prevalence and rates of recognition of anxiety disorders in internal medicine outpatient departments of 23 general hospitals in Shenyang, China. Gen Hosp Psychiatry 2010;32:192-200. [Crossref] [PubMed]
- Qin X, Wang W, Jin Q, et al. Prevalence and rates of recognition of depressive disorders in internal medicine outpatient departments of 23 general hospitals in Shenyang, China. J Affect Disord 2008;110:46-54. [Crossref] [PubMed]
- Löwe B, Spitzer RL, Williams JB, et al. Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment. Gen Hosp Psychiatry 2008;30:191-9. [Crossref] [PubMed]
- Lecrubier Y. Widespread underrecognition and undertreatment of anxiety and mood disorders: results from 3 European studies. J Clin Psychiatry 2007;68 Suppl 2:36-41. [PubMed]
- Ormel J, Koeter MW, van den Brink W, et al. Recognition, management, and course of anxiety and depression in general practice. Arch Gen Psychiatry 1991;48:700-6. [Crossref] [PubMed]
- Wells KB, Hays RD, Burnam MA, et al. Detection of depressive disorder for patients receiving prepaid or fee-for-service care: results from the Medical Outcomes Study. JAMA 1989;262:3298-302. [Crossref] [PubMed]
- Rao JK, Weinberger M, Kroenke K. Visit-specific expectations and patient-centered outcomes–a literature review. Arch Fam Med 2000;9:1148-55. [Crossref] [PubMed]
- Mitchell AJ, Vaze A, Rao S. Clinical diagnosis of depression in primary care: a meta-analysis. Lancet 2009;374:609-19. [Crossref] [PubMed]
- Hansen MS, Fink P, Frydenberg M, et al. Mental disorders among internal medical inpatients. Prevalence, detection, and treatment status. J Psychosom Res 2001;50:199-204. [Crossref] [PubMed]
- Pasacreta JV, Massie MJ. Nurses’ reports of psychiatric complications in patients with cancer. Oncol Nurs Forum 1990;17:347-53. [PubMed]
- Maguire P, Tait A, Brooke M, et al. Effect of consultation on the psychiatric morbidity associated with mastectomy. Br Med J 1980;281:1454-6. [Crossref] [PubMed]
- Hardman A, Maguire P, Crowther D. The recognition of psychiatric morbidity on an oncology ward. J Psychosom Res 1989;33:235-9. [Crossref] [PubMed]
- Phillips MR, Zhang J, Shi Q, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet 2009;373:2041-53. [Crossref] [PubMed]
- Seekles WM, Cuijpers P, van de Ven P, et al. Personality and perceived needs for mental health care among primary care patients. J Affect Disord 2012;136:666-74. [Crossref] [PubMed]
- Prins MA, Verhaak PF, van der Meer K, et al. Primary care patients with anxiety and depression: Needs for care from the patient's perspective. J Affect Disord 2009;119:163-71. [Crossref] [PubMed]
- Wisely JA, Tarrier N. A survey of the needs for psychological input in a follow-up service for adult burn-injured patients. Burns 2001;27:801-7. [Crossref] [PubMed]
- Hodgkinson K, Butow P, Hunt GE, et al. Breast cancer survivors’ supportive care needs 2-10 years after diagnosis. Support Care Cancer 2007;15:515-23. [Crossref] [PubMed]
- Jackson JL, Kroenke K. The effect of unmet expectations among adults presenting with physical symptoms. Ann Intern Med 2001;134:889-97. [Crossref] [PubMed]
- Rohrbaugh M, Rogers JC. What did the doctor do? When physicians and patients disagree. Arch Fam Med 1994;3:125-8. [Crossref] [PubMed]
- Richards HL, Fortune DG, Werdmann A, et al. Detection of psychological distress in patients with psoriasis: Low consensus between dermatologist and patient. Br J Dermatol 2004;151:1227-33. [Crossref] [PubMed]
- Kroenke K, Spitzer RL, Williams JB, et al. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry 2010;32:345-59. [Crossref] [PubMed]
- Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ 2012;184:E191-6. [Crossref] [PubMed]
- Bian CD, He XY, Qian J, et al. The reliability and validity of a modified patient health questionnaire for screening depressive syndrome in general hospital outpatients. Journal of Tongji University 2009;30:136-40. (Medical Science).
- Kroenke K, Spitzer RL, Williams JB, et al. Anxiety Disorders in Primary Care: Prevalence, Impairment, Comorbidity, and Detection. Ann Intern Med 2007;146:317-25. [Crossref] [PubMed]
- Witthöft M, Hiller W, Loch N, et al. The Latent Structure of Medically Unexplained Symptoms and Its Relation to Functional Somatic Syndromes. Int J Behav Med 2013;20:172-83. [Crossref] [PubMed]
- He XY, Li CB, Qian J, et al. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients. Shanghai Arch Psychiatry 2010;22:200-3.
- Prins MA, Verhaak PF, Bensing JM, et al. Health beliefs and perceived needs for psychological care of anxiety and depression-the patients' perspective explored. Clin Psychol Rev 2008;28:1038-58. [Crossref] [PubMed]
- Craske MG, Edlund MJ, Sullivan G, et al. Perceived unmet needs for mental health treatment and barriers to care among patients with panic disorder. Psychiatr Serv 2005;56:988-94. [Crossref] [PubMed]
- Johnson U. Coping strategies among long-term injured competitive athletes. A study of 81 men and women in team and individual sports. Scand J Med Sci Sports 1997;7:367-72. [Crossref] [PubMed]
- Simon GE, VonKorff M. Recognition, management, and outcomes of depression in primary care. Arch Fam Med 1995;4:99-105. [Crossref] [PubMed]
- Chew-Graham CA, Mullin S, May CR, et al. Managing depression in primary care: another example of the inverse care law? Fam Pract 2002;19:632-7. [Crossref] [PubMed]
- Gonzalez EW. Relationships of nurses’ critical thinking ability and perceived patient self-disclosure to accuracy in assessment of depression. Issues Ment Health Nurs 1996;17:111-22. [Crossref] [PubMed]
- McDonald MV, Passik SD, Dugan W, et al. Nurses’ recognition of depression in their patients with cancer. Oncol Nurs Forum 1999;26:593-9. [PubMed]
- Worden JW, Weisman AD. Do cancer patients really want counseling? Gen Hosp Psychiatry 1980;2:100-3. [Crossref] [PubMed]
- Kwon DH, Tisnado DM, Keating NL, et al. Physician-reported barriers to referring cancer patients to specialists: prevalence, factors, and association with career satisfaction. Cancer 2015;121:113-22. [Crossref] [PubMed]


