
Ethical issues in patients referred for palliative radiation therapy
Introduction
In health care, principles of patient autonomy, beneficence, non-maleficence, and justice serve as a moral framework for patient care (1). Ethical dilemmas often arise when there are tensions between these four principles, and providers must be able to navigate clinical decision-making in these circumstances. The care of oncology patients often involves various ethical dilemmas, related to the doctor-patient relationship, cultural barriers, concepts of hope, spirituality, special ethical considerations in pediatric patients, suffering, and end-of-life (2). These patients often have complex medical issues and various clinical providers, which can make patient autonomy very challenging, as it is not always clear how beneficence can be optimized for patients, as symptom-relief and treatment response are not always predictable (3,4). Many cancer therapies themselves, whether palliative or curative in intent, can cause harm or toxicity, making non-maleficence a difficult principle to uphold. Even when patients have clearly decided to favor palliative intent of treatment over curative, there can still be conflicts in treatment plans, between providers, and between family members. A qualitative study of nurses and physicians regarding end-of-life issues in a population of patients admitted to the ICU showed that uncertainty about the best course of action in patient led to moral distress, and competing values, hierarchy, and communication emerged as common themes (5). Given the complexity of care and the acuity of illness in patients with advanced cancer, providers of these patients are often exposed to ethical dilemmas.
Radiation oncologists often encounter patients with advanced cancer when they are referred for palliative radiation therapy (PRT). PRT is often delivered in the context of complex, urgent, medical scenarios, since palliative radiotherapy is generally delivered when metastatic disease has progressed and become emergently symptomatic and potentially life threatening. These emergencies include brain metastases, spinal cord compression, obstruction from visceral metastases, and bleeding (6). Often, various specialty teams work in parallel to manage these emergencies, and there may not be a clear or most obvious choice of optimal first-line treatment. For example, the management of brain metastases and spinal cord compression involve parallel or sequential care with neurosurgery (7), and obstructive masses and bleeding tumors can involve a variety of other interventional specialties.
While the decision to offer treatment itself may be challenging, there may be additional ethical issues as radiation oncologists consider how to approach PRT for a given patient. Radiation oncologists have to consider the patient’s goals of care and prognosis in order to provide appropriate, patient-centered treatment recommendations. However, it has been demonstrated that physicians typically cannot prognosticate accurately at the end of life, limiting their ability to offer the most appropriate palliative treatment options (8,9). One study demonstrated that physicians estimate that 27% of patients they treated within the last 30 days of life died sooner than expected, suggesting that even though they believe they are maximizing benefit for patients, the magnitude of that benefit is likely overestimated (10). Furthermore, patients and caregivers do not necessarily understand the intent of palliative treatment clearly, mistaking their treatment as curative, which may result in unintended harm (11).
To best educate and prepare radiation oncologists to manage any ethical issues as they care for patients with advanced cancer, a thorough description of the frequency and types of ethical issues that are encountered is required. However, little data are available to describe the frequency and range of ethical issues encountered in patients considered for PRT. Our research fills a critical gap in the literature by describing the frequency and types of ethical issues encountered by radiation oncologists caring for patients referred for PRT through a survey-based study.
Methods
Survey and participants
After receiving approval from the Institutional Review Board of participating radiation oncology centers, we delivered surveys electronically to radiation oncology clinicians who received consultations for PRT through a specific palliative radiation oncology service at 3 hospitals over the course of 4 months. Patients were referred either through our inpatient consultation team, generally comprised of dedicated attending physicians and nurse practitioners who specialize in the care of these patients, and rotating residents, for whom this service is embedded throughout their training. They could also be referred for outpatient evaluation by these same practitioners if they had a palliative intent treatment but were stable enough to be seen as outpatients, such as pain from a bony metastasis. All consultations received between May 19, 2014 and September 26, 2014 were eligible for evaluation if the patient was 21 years of age or older, with incurable, metastatic cancer. Immediately after each PRT consultation, the consulting clinician was sent a survey to be completed within 5 business days of the consultation. Requests to complete the survey were sent three times over the 5-day interval. We sent 15 clinicians, consisting of nurse practitioners, resident physicians, and attending physicians, 162 surveys over the study period. For their participation, survey respondents received one $25 gift card regardless of the number of surveys completed.
The survey was developed as part of a comprehensive assessment of the burden of palliative care issues encountered in palliative radiation consultations, with the survey development methods previously described (12). The domains of palliative care assessed were derived from the National Consensus Project domains of palliative care and the National Comprehensive Cancer Network (13,14). Eight palliative care domains were evaluated—physical symptoms, psychosocial issues, cultural consideration, spiritual needs, care coordination, advanced care planning, goals of care, and ethical and legal issues. Within 1 week of the consultation, clinicians ranked the relevance of each of the eight-palliative care domain to that patient’s care within radiation oncology on a 5-point scale from ‘not relevant’ to ‘extremely relevant’. Within each domain, there were further subdomains (31 in total) to which clinicians indicated the relevance to care as ‘yes’, ‘no’ or ‘not assessed’. Within the ethical issues domain, there were five subdomains of assessment identifying the types of ethical conflicts encountered, including: (I) conflict between clinicians, (II) conflict between caregivers and clinicians, (III) internal conflict, (IV) feeling blocked from doing what was best for the patient, (V) violation of personal morals, and an option for unclassified issues, with an open-ended response.
Patient demographic and disease data were extracted from the electronic medical record corresponding to each completed survey. Demographic information collected included age, gender, and marital status. Disease information collected included primary cancer type, performance status (PS), reasons for radiation therapy consultation, and radiation therapy recommendation and target site.
Statistical analysis
Descriptive statistics were calculated as proportions for categorical variables. Continuous variables were analyzed as a mean and standard deviation or a median and range. Palliative care issue domains were dichotomized as “relevant” or “not relevant” to each consultation. We used univariate (UVA) analyses to initially assess potential predictors of ethical issues, which included gender, age, marital status, primary cancer type, PS, indication for PRT, PRT recommendation, and plan for future anticancer therapy. In addition, we assessed the relationship of ethical issues to other issues identified in the surveys, e.g., the presence of physical symptoms, psychosocial issues, goals of care, care-coordination, cultural issues, or spiritual issues using chi square tests. Our multivariable analysis model included all significant (P<0.05) univariate predictors to assess relationships to ethical issues. We did not control for provider-specific variables as there were insufficient events per provider for meaningful analysis.
Open-ended responses were independently reviewed and coded for similar themes (Author 1 and Author 9) and validated by a third person in the case of disagreement (Author 4).
Results
Characteristics of the patient consultations are shown in Table 1. Over the course of the study, 162 patients were seen in consultation for PRT. Of the 162 surveys sent to clinicians, 140 responses were completed (86% response rate). Patients were most commonly referred for PRT for pain (n=80, 57%) brain metastases (41, 29%) cord compression (18, 13%) and visceral metastases (28, 20%). PRT was recommended in 120 of the 140 consultations (86%).

Full table
Of the 140 patient consultations, 14 (10%) involved ethical issues relevant to the patient’s care, with the majority of ethical issues being highly relevant to the radiation oncologist’s care of the patient. For 3 out 14 patients, radiation was not recommended, and the remainder received PRT. Of those 14, 11 (78%) involved more than one ethical issue relevant to care. Types of ethical issue encountered by radiation oncologists are shown in Figure 1, with 7 (50%) of ethical issues involving conflict between clinicians about the care plan for the patent; half involving conflict between patient/family and clinicians about the care plan; (43%) involved clinician distress or internal conflict within the care for that patient; a small minority (14%) felt impeded from doing what they felt was best for the patient; and no clinician noted the care plan violated personal ethics or morals. Five patient encounters were noted to have other unspecified ethical issues.

Open-ended responses included a variety of conflicts, including disease-related conflict, patient-provider conflict, provider-provider conflict, and financial concerns. Of the 10 open-ended responses, 50% (n=5) identified disease-related conflict, where there were difficult management decisions based on the disease progression or presentation alone, such as two sites of involvement. Examples included a patient presenting with a new mediastinal tumor in the setting of metastatic prostate cancer, a patient presenting with brain metastases as well as an enlarging neck mass; and a new diagnosis of metastatic versus limited disease that impacted staging and subsequent course of care. Additionally, 30% (n=3) identified conflict between the patient or family’s wishes and those of their provider, 10% (n=1) identified conflict between the clinician completing the survey and another provider, and 10% (n=1) identified financial concerns as the source of conflict.
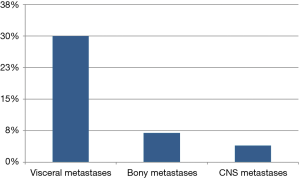
On univariate analysis, ethical conflicts were significantly (P<0.05) associated with PRT referrals for bleeding, dyspnea, or dysphagia due to visceral metastases (30%) versus for CNS indications like brain metastases or cord compression (7%) or bony metastases (4%) (Figure 2), P<0.001. Ethical issues tended to be more common among patients with psychosocial (13% vs. 4%, P=0.13) or spiritual issues (23% vs. 5%, P=0.001). Gender, PS, PRT recommendation and proceeding to hospice/end-of-life care were not significantly associated with the presence of ethical issues (Table 2). We also examined the relationships of other palliative care issues relevant to ethical issues (Table 2), with 23% of patients with spiritual issues present associated with the presence of ethical issues versus 5% of patients without spiritual issues identified associated with ethical issues present (P<0.001). In other words, if patients were likely to have spiritual issues present, they were also more likely to have ethical issues. The presence of psychosocial issues demonstrated a trend of association with the presence of ethical issues (13% vs. 4%, P=0.13), although not statistically significant.

Full table
On multivariate analysis, PRT for visceral metastases (OR 13.0; 95% CI, 2.3–74.6, P<0.001) and presence of spiritual issues (OR 4.0; 95% CI, 1.1–14.5, P=0.04) were significantly associated with ethical issues.
Discussion
Care for patients with advanced cancer can be extremely complex, involving multiple disciplines, medical sub-specialties, and treatment options. Radiation oncologists commonly encounter these patients through consultations for PRT, which are estimated to comprise at least a third of treatments administered by radiation therapy (15). Of these patients, our study finds that approximately 1 in 10 referrals for PRT involve ethical issues relevant to the radiation oncologist’s care of the patient.
Ethical issues may be identified at a higher frequency in consultations for palliative radiation in patients who are referred for bleeding, dysphagia, and dyspnea versus those who are referred for cord compression, brain metastases, and pain. Given that clinician-clinician conflict was identified in this context, one possible hypothesis for this observation is the management of the former end-of-life issues often involves many potential consultants and management options, while the latter conditions of cord compression, brain metastases, and pain typically involve one surgical subspecialty and radiation oncology alone as primary management. This may suggest development of care pathways and further research on the comparative effects of interventions for visceral metastases may be helpful. Future research may better define the clinical threshold for radiation therapy for bleeding metastases after endoscopic approaches.
Furthermore, our study demonstrates that ethical issues may be identified more readily when there are spiritual concerns. Literature on ethical dilemmas often report conflict in the setting of religious or spiritual beliefs, and our findings support this (16). Spiritual distress, while a patient-specific characteristic, was identified by our providers as relevant to the consultation, and therefore may track with the provider’s ability to identify ethical issues. For example, patients who vocalize spiritual concerns, whether it is an existential dilemma at the end of life or they feel aspects of their care conflict with their religious framework, may be more obviously identified by providers as having an ethical conflict, instead of those patients who have coordination of care issues alone. From prior studies, we know providers may lack comfort in discussing spiritual concerns and this may also account for some ethical conflict (17,18). Incorporating training in engaging with patients’ spirituality may help lessen the impact of this on ethical conflict.
The subjective responses recorded provide interesting insights into the types of situations leading to ethical conflict, with themes suggesting that disagreement about the plan of care between various specialties is an important source of moral distress. Future studies may involve examining the role of multidisciplinary review, discussion, and coordinated visits for patients referred for palliative indications on the impact of ethical issues.
Strengths of this study include the prospective identification of ethical conflicts in a population of patients referred for PRT. Other studies examining ethical conflict in oncology populations generally identify patients who have already been referred for ethical consultation (2,19-21), which is often an underutilized service, and may represent a highly selective population. Therefore, this study can give us a greater scope of the range and types of ethical conflicts radiation oncologists can expect to encounter. Furthermore, the open-ended responses provide insight into potential opportunities for further research, intervention, and education. While we captured ethical issues that arise in a palliative setting, there can be many ethical issues and situations fraught with moral distress arising in curative settings, which may be even more difficult to identify. We hope that education in medical ethics will allow providers to identify these issues throughout the course of a patient’s care, regardless of treatment intent.
Limitations of this study are that these responses were elicited from providers, and not patients. It is possible that patients may identify a greater proportion and range of ethical conflicts than were observed and discussed within the consultation. Furthermore, this study asked radiation oncology clinicians about the presence of ethical issues relevant to care of the patients receiving PRT. Though most appropriate to inform the scope of ethical issues encountered in radiation oncology care, this likely underestimates the full scope of ethical issues experienced in the care of patients with advanced cancer. Further studies, which incorporate surveys of all clinical providers, patients, and family members, may enrich the data regarding ethical conflicts and provide additional points for intervention and improvement. While some may raise concern that the majority of the conflicts were identified by nurse practitioners or by residents, we believe that ethical issues can be identified by any member of a clinical team, by patients, or family members. There is no specific reason why attending physicians would be better suited to identifying ethical issues than any other member of the team. In fact, one may argue that recent changes in curriculum better train young trainees in the identification of ethical issues (22,23). Further studies that investigate the level of medical training and identification of ethical issues in these settings may be illustrative as to whether or not the rank or role of the provider has any bearing on these findings. Additionally, the rate of ethical burdens may not be generalizable to centers without a dedicated palliative radiation oncology team.
Conclusions
In conclusion, radiation oncologists seeing patients for consideration of PRT frequently encounter ethical dilemmas with some frequency. Potential predictors identified by this study include indications for PRT for visceral metastases (bleeding, dysphagia, and dyspnea) and the presence of spiritual concerns. These findings highlight a need for further research and clinician education in the realm of medical ethics.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of participating radiation oncology centers. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th edition. Oxford: Oxford University Press, 2001.
- Angelos P. Ethical issues in cancer patient care. Berlin/Heidelberg: Springer Science & Business Media, 2007.
- Walsh J, Young JM, Harrison JD, et al. What is important in cancer care coordination? A qualitative investigation. Eur J Cancer Care (Engl) 2011;20:220-7. [Crossref] [PubMed]
- Bruera E, Hui D. Integrating supportive and palliative care in the trajectory of cancer: establishing goals and models of care. J Clin Oncol 2010;28:4013-7. [Crossref] [PubMed]
- Oberle K, Hughes D. Doctors' and nurses' perceptions of ethical problems in end-of-life decisions. J Adv Nurs 2001;33:707-15. [Crossref] [PubMed]
- Konski A, Feigenberg S, Chow E. Palliative radiation therapy. Amsterdam: Elsevier, 2005:156-64.
- Patchell RA. The management of brain metastases. Cancer Treat Rev 2003;29:533-40. [Crossref] [PubMed]
- Krishnan MS, Epstein-Peterson Z, Chen YH, et al. Predicting life expectancy in patients with metastatic cancer receiving palliative radiotherapy: the TEACHH model. Cancer 2014;120:134-41. [Crossref] [PubMed]
- Glare P, Virik K, Jones M, et al. A systematic review of physicians' survival predictions in terminally ill cancer patients. BMJ 2003;327:195-8. [Crossref] [PubMed]
- Lloyd S, Dosoretz AP, Yu JB, et al. Radiation Oncologists’ Attitudes and Intentions Regarding Palliative Radiation Therapy Near the End of Life. Int J Radiat Oncol Biol Phys 2013;87:S563. [Crossref]
- Chen AB, Cronin A, Weeks JC, et al. Expectations about the effectiveness of radiation therapy among patients with incurable lung cancer. J Clin Oncol 2013;31:2730-5. [Crossref] [PubMed]
- Parker GM, LeBaron VT, Krishnan M, et al. Burden of palliative care issues encountered by radiation oncologists caring for patients with advanced cancer. Pract Radiat Oncol 2017;7:e517-24. [Crossref] [PubMed]
- National Consensus Project for Quality Palliative Care. Clinical Guidelines for Quality Palliative Care. 2013.
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Palliative Care [Internet]. 2013 [cited 2013 Nov 26]. Available online: http://www.nccn.org/professionals/physician_gls/pdf/palliative.pdf
- Janjan NA. An emerging respect for palliative care in radiation oncology. J Palliat Med 1998;1:83-8. [Crossref] [PubMed]
- Ikeda D, Simard R, Bourgeault G. On being human: Where ethics, medicine and spirituality converge. Santa Monica: Middleway Press, 2003.
- Balboni MJ, Sullivan A, Enzinger AC, et al. Nurse and physician barriers to spiritual care provision at the end of life. J Pain Symptom Manage 2014;48:400-10. [Crossref] [PubMed]
- Balboni MJ, Sullivan A, Amobi A, et al. Why is spiritual care infrequent at the end of life? Spiritual care perceptions among patients, nurses, and physicians and the role of training. J Clin Oncol 2013;31:461-7. [Crossref] [PubMed]
- Lo B, Jonsen AR. Ethical decisions in the care of a patient terminally ill with metastatic cancer. Ann Intern Med 1980;92:107-11. [Crossref] [PubMed]
- Shuman AG, McCabe MS, Fins JJ, et al. Clinical ethics consultation in patients with head and neck cancer. Head Neck 2013;35:1647-51. [Crossref] [PubMed]
- Voigt LP, Rajendram P, Shuman AG, et al. Characteristics and Outcomes of Ethics Consultations in an Oncologic Intensive Care Unit. J Intensive Care Med 2015;30:436-42. [Crossref] [PubMed]
- Yerramilli D. On cultivating the courage to speak up: the critical role of attendings in the moral development of physicians in training. Hastings Cent Rep 2014;44:30-2. [Crossref] [PubMed]
- Lee LM, Viers HW, Anderson MA. The Presidential Bioethics Commission: pedagogical materials and bioethics education. Hastings Cent Rep 2013;43:16-9. [Crossref] [PubMed]


