
Perceived knowledge of palliative care among immigrants to the United States: a secondary data analysis from the Health Information National Trends Survey
Introduction
Immigrants and those with language barriers have been shown to have worse access to healthcare, suffer numerous adverse health outcomes in the in-patient and out-patient setting and perceive that the quality of healthcare they receive is poor (1-14). The adverse consequences of this disparity may become most stark and damaging at end of life. The United States (US) has long been a country of immigrants. The number of immigrants in the US has increased steadily since the 1980s, and comprised approximately 44 million or 13.5% of the population in 2016 (15). Immigrants face many difficulties on arrival in a new country including, for some, language barriers. Fifty to eighty percent of the individuals who are born outside the US have limited English proficiency (LEP) (16,17). A person with LEP is an individual who speaks English less than “very well” per the US Census Bureau’s classification (17). The language skills of those born outside the US are usually a reflection of their age at immigration and length of time in the US (16,18). The most commonly spoken language among immigrants in the US are Spanish and Chinese (17).
Palliative care focuses on enhancing quality of life by integrating the emotional, psychological, social, and physical aspects of care. Palliative care can be instigated in a variety of clinical scenarios including to improve care during ongoing chronic illness as well as for symptom control during end of life (19-21). The Institute of Medicine’s 2014 report “Dying in America” served as a call to action for increased public education and engagement about end-of-life care (22,23).
Although there are widespread efforts to promote palliative care as a means to improve quality of life and death, knowledge of and access to these resources remain elusive for many patient populations, including immigrants (24). There is evidence of a limited understanding of the concept of palliative care for some who immigrate to the US (25). While some educational materials about palliative care exist in languages other than English and the US National Library of Medicine has a range of resources in multiple languages, it is likely that most easily accessible resources will be in English (26). Additionally, these resources may not be written at the recommended 3rd to 7th grade reading levels even in English (27).
Previous studies have shown that immigrants and those with LEP receive more interventions at the end of life and are less likely to withdraw life sustaining treatments, have advance care planning in place, accept do-not-resuscitate orders, or receive comfort measures prior to imminent death (28,29). It is unclear if these differences reflect knowledge and understanding of palliative care options or are true preferences (30). If indeed knowledge is lacking or communication is poor, this could represent a disparity in care (31).
The primary objective of this study was to measure and describe levels of perceived knowledge about palliative care among immigrants to the US compared to those born in the US. Our secondary objective was to identify trusted sources for seeking information about palliative care among immigrants and to compare these trusted sources with those born in the US. We hypothesized that immigrants would have less knowledge of palliative care than those born in the US and use different trusted sources for information about palliative care. To investigate these objectives, we used data from the 2018 administration of the National Cancer Institute (NCI)’s Health Information National Trends Survey (HINTS), a nationally representative survey whose primary aim is to collect information on the general public’s perceptions and use of health-related information, health communication, and health-related behaviors (32,33).
Methods
Study population and data sources
We analyzed data from the HINTS 5, Cycle 2 iteration. HINTS 5, Cycle 2 questionnaires were administered via mail between January and May 2018 to a population-based sample of non-institutionalized adults ages 18 and older in the US, in English and Spanish (upon request). Cover letters were provided in Spanish with circulated surveys and phone-lines available with Spanish speakers to answer questions and requests about Spanish language materials. In order to capture a nationally representative sample, a probability-based sampling frame was used in a two-stage design process. Initially, based on data from Marketing Systems Group (MSG) a stratified sample of residential addresses was identified, from these households one adult was selected randomly to participate in the survey. Oversampling of those living in central Appalachia and those from minority groups was attempted. Survey response rate was 32.9% (n=3,504). Additional information regarding survey methodology is elaborated in the HINTS methodology report (34). Imputation strategies were conducted by Westat when missing responses for select sensitive items occurred or respondents selected more than one response inappropriately. For the purposes of these analyses, the respondent data used was restricted to those who responded to items regarding whether they were born in the US. The study was approved by the NIH IRB prior to delivery and is a publically available data set that is sufficiently de-identified so as not to require additional IRB approval.
Demographic and language-related variables
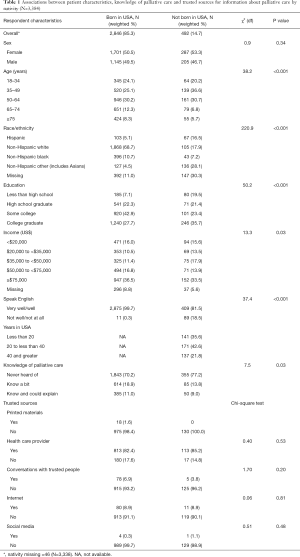
Sociodemographic variables examined included sex, age category, race/ethnicity, education, and income (Table 1). Respondents were also asked to indicate their English language proficiency with the question: “How well do you speak English?” (“very well”, “well”, “not well”, or “not at all”). The primary predictor variable was nativity (i.e., whether an individual was born in the US).
Full table
Immigrants or foreign born are people residing in the US who were not US citizens at birth. Among this population are those who are naturalized citizens, lawful permanent residents, people on a temporary work or student visas, those admitted as a refugee or with asylum status, as well as those living in the US without documentation (15). The relative proportion of each of these groups within the cohort is unknown. For those who were not born in the US, the number of years of residence in the US was calculated using the year of survey administration [2018] minus the self-reported year the respondent arrived in the US.
US born includes those born within the 50 states and District of Columbia, US territories, and those born abroad to a parent or parents with US citizenship (15).
Outcome measures
The primary outcome of interest was perceived knowledge of palliative care, assessed using the item “How would you describe your level of knowledge about palliative care?” Potential responses included: “I’ve never heard of it,” “I know a little bit about palliative care,” and “I know what palliative care is and could explain it to someone else.” For the purposes of these analyses, this variable was dichotomized based on response distribution; the resultant categories were either “I’ve never heard of it/I know a little bit” and “I know what palliative care is and could explain it to someone”.
The secondary outcome of interest was determining which sources respondents trusted for information about palliative care; this was done using the item “Imagine you had a strong need to get information about palliative care, which of the following would you most trust as a source of information about palliative care?” Respondents were asked to select one of the following: “printed material (for example, newspapers, and magazines),” “health care provider (doctor, nurse, social worker),” “conversations with people you trust (friends, relatives, co-workers),” “internet (google or another search engine, WebMD or another medical website),” or “social media (Facebook, Instagram, and Twitter).”
Data analyses
All analyses were complete case analyses and conducted with survey commands using SAS 9.3 (SAS Institute Inc, Cary, NC, USA); to accommodate the complex sampling procedure and jackknife replicate weights used for population-level estimates. We examined differences in the covariates and outcome measures as a function of nativity/English proficiency using bivariate analytic techniques (χ2 tests and Rao Scott modified chi-square test) (Table 1). To be included in the multivariate analyses respondents had to have indicated whether they were US or foreign born (3,338/3,504).
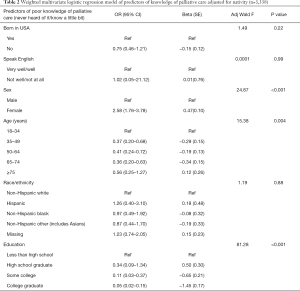
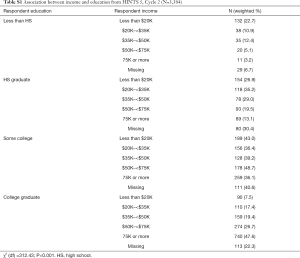
We used multivariable logistic regression to examine associations between knowledge of palliative care and nativity adjusting for statistically significant and theoretically relevant sociodemographic variables. All models were adjusted for sex, age, race/ethnicity, and education. In order to maintain as parsimonious a model as possible, we did not include income in the final model (Table 2). Collinearity between income and education was examined and demonstrated (Table S1).
Full table
Full table
Due to the small numbers of respondents who answered the question about trusted sources and the lack of notable differences between those born in the US and those not born in the US, we did not do further multivariate analysis on this outcome.
Results
We restricted analyses to those who responded to the question about nativity (complete case analysis). Of the 3,388 who answered the question about nativity, 2,846 (85.3% weighted) were born the US and 492 (14.7% weighted) were not born in the US. Fourteen people completed the survey in Spanish.
Unadjusted associations between sociodemographic characteristics and knowledge of palliative care
Bivariate analyses were used to examine the relationship between nativity and poor knowledge of palliative care as well as trusted sources of palliative care knowledge. Table 1 shows weighted proportions and means for relevant sociodemographic variables, covariates, and outcome measures for USA born compared to non-USA born.
There were no significant differences in sex distribution between US and foreign-born respondents, with about half of each group being female (P=0.34) (Table 1). A larger proportion of US natives were over 65 years old (P<0.0001). There were larger proportions of Hispanics and non-Hispanic other (including Asians) among those not born in the US and a larger proportion of non-Hispanic whites within the USA-born group. Although the proportions of college graduates were similar between the two cohorts, over twice as many foreign-born respondents had less than a high school education than those respondents born in the US (19.5% weighted versus 7.1% weighted, respectively, P<0.001). There were some small income differences between the groups, although specific trends were difficult to identify. A higher proportion of those born in the US reported speaking English “very well” or “well” as compared to those not born in the US (99.7% weighted versus 81.5%weighted, respectively, P<0.001). About one third of foreign-born respondents had been here less than 20 years, over 40% had been here between 20 and 40 years, and just over 20% had been here longer than 40 years (Table 1).
There were some differences in knowledge of palliative care between those born in the US and those not born in the US. A smaller proportion of those born in the US had never heard of palliative care (70.2% weighted versus 77.2% weighted, respectively); a larger proportion of those born in the US knew a bit or knew a bit and could explain (29.9% weighted versus 21.8% weighted) (P=0.03).
Unadjusted associations between sociodemographic characteristics and trusted sources of palliative care information
There were few differences in preferred trusted sources of palliative care information based on nativity (Table 1). Neither group used printed materials or social media as trusted sources of palliative care information. Both groups’ most preferred trusted source of palliative care information was “health care provider,” with over 80% of respondents in each group selecting this option. The “internet” and “conversations with trusted people” were the least frequent selections, making up less than 10% of each cohort (Table 1).
Adjusted associations of knowledge of palliative care and nativity
We then conducted multivariable binomial logistic regression modelling of nativity on palliative care knowledge to control for potential confounding or effect modifying variables (age group, sex, race/ethnicity, and education, LEP). No significant associations were found between poor knowledge of palliative care and nativity. Neither race/ethnicity nor LEP was a reliable predictor of poor knowledge of palliative care (Table 2).
After controlling for other variables, analyses demonstrated that female respondents had a 2.5 increased odds of self-reporting low levels of knowledge of palliative care when compared to male respondents (OR =2.58; 95% CI, 1.76–3.78; P<0.001). There was an increased odds of poor knowledge of palliative care among the youngest age group (18–34 years). An independent relationship existed between education and poor knowledge of palliative care. Respondents with less than high school education endorsed poor knowledge compared with high school graduates, those with some college, and college graduates. We also examined years in the USA and its association with knowledge of palliative care and we did not find any relationship.
Discussion
In this study, the HINTS 5 Cycle 2 data were used to assess perceived knowledge about palliative care among immigrants to the US. We also analyzed trusted sources of information about palliative care among this population as compared to those born in the USA. We expected perceived knowledge to be lower in this population and for this population to have different trusted sources of information about palliative care; however, our study did not show the expected differences.
Among the predictors of perceived poor knowledge of palliative care, we did not find that nativity or immigration status was significant. Additionally, trusted sources of palliative care knowledge among immigrants were very similar to those born in the US. The preferred sources of knowledge among both immigrants and non-immigrants were healthcare providers. Printed materials and social media were the least popular trusted sources among both groups. Education, however, was an important predictor of knowledge and as education increased from high school to college, perceived knowledge of palliative care also increased. Among the youngest age group (18–34 years), the odds of poor knowledge of palliative care were highest and, although statistically significant differences were seen in some age categories, no specific trends were identified from which to derive inferences.
An unexpected finding of our study was that women were 2.5 times as likely to perceive they had poor knowledge of palliative care as men. The reason for this finding is not entirely clear and unanticipated particularly considering that women more often than men take on caregiver roles during chronic illness and at end of life (either informally or formally). Qualitative research of women with gynecological cancers indicated that women manifested little knowledge about palliative care and considered it “a place to die” but formal testing of actual knowledge among the general female population has not been done (35). It is possible that either women underestimate their knowledge or men over-estimate their knowledge. A validated test of actual knowledge comparing men and women would elucidate this better but has not been done.
Previous studies have demonstrated that immigrant groups receive more interventions at the end of life (28). Our findings contrast with some of the evidence about knowledge of palliative care. A literature review about end of life care among minority ethnic groups in the UK noted that inadequate knowledge of the structures of medical care as well as inadequate awareness of palliative care offerings were among several factors explaining the lower use of palliative care among these populations (36-39). Although that study did not focus only on immigrants it is likely that similar issues could arise in the US for immigrants and our study did not detect this. It is possible that structural mechanisms at the level of healthcare institutions may contribute to these differences in end of life care among immigrant populations with inadequate communication for those who have LEP and low health literacy or education levels. Other potential mediators and moderators of these differences may include individual patient-level factors that result in differences in receptivity to palliative care such as cultural and faith-based beliefs that influence conceptual understanding of, discussion of, and acceptance of palliative care (40). It is difficult to parse out the complex interactions between language, immigration status, access, and other social determinants of health that may mediate or moderate receptivity to palliative care.
The most impactful finding of this work was that perceived knowledge of palliative care was poor among both those born in the US and those not born in the US, with over 70% in each group declaring they had “never heard of” palliative care and only about 10% in each group declaring they knew “what palliative care is and could explain it to someone else.” These findings corroborate the Institute of Medicine’s report from 2014 recommending that increased public engagement and education to improve knowledge of palliative care was a priority (23,41). Other studies have also shown that misunderstandings about options at end of life are common (42) particularly regarding withdrawal of treatment at end of life, even if knowledge of with-holding of life sustaining treatment was fairly robust.
Based on our findings that overall self-perceived knowledge of palliative care is poor in the population and associated with low levels of education, we should continue to focus our efforts on improving learning about palliative care being especially mindful about reaching those with functional and health literacy issues and tailor educational materials to meet their needs (43,44). Furthermore, this awareness campaign and service provision (e.g., advance care planning) should continue to integrate with chronic disease management toward a goal of reducing symptom burden during the course of illness and continuum of disease. Sound knowledge of palliative care would be very useful in a variety of situations and could improve quality of life for some of the 60% of the population managing chronic illness even if they are not at end of life (45). Since clinicians are cited in the survey as the preferred trusted source of palliative care information and may lack sufficient training and knowledge about palliative care, the onus should be on clinicians to educate themselves with a view to further educating their patients and families about what palliative care is and when it can be beneficial (23).
The primary limitation of this cross-sectional survey study is the fact that it can only be taken in English or Spanish. Those who would like to complete the survey in Spanish must request a paper copy be mailed to their postal address. In this case, only 14 surveys were completed in Spanish. It is likely that participants who do not speak either of these languages will be less inclined to complete the survey, or to misinterpret the questions. Therefore the immigrant population we captured did not include a representative proportion of those with LEP, over 50% of foreign-born populations (17). These factors may cause selection and response bias. The immigrants who participated may be more likely to speak English and potentially be more integrated into US society than newly arrived immigrants who have language barriers and do not have permanent addresses. Our response rate was 33%, comparable to many national surveys. Since we were conducting secondary data analysis on the HINTS data, we were limited by the sampling strategy used, therefore some groups may have been underpowered. Those who are immigrants, particularly recent immigrants may be less likely to have permanent addresses and therefore may be less likely to be within the sampling frame. Furthermore, since we are doing secondary data analysis of a cross-sectional survey, we are restricted by the inherent flaws of the research design and the questions and response choices. For example, our secondary outcome about trusted sources did not specify any options for faith-based sources of information. Community engagement of the public to increase education about healthcare issues particularly minority groups, is increasingly occurring through faith-based congregations and organizations (46,47). It is possible that the question in its current format could not capture this information. Another limitation is the fact that our analysis was done on a survey question about perceived knowledge of palliative care rather than actual knowledge of palliative care. Knowledge of palliative care is difficult to quantify as access to palliative care and standardization of palliative care services and quality may vary nationally, regionally and by county and hospital (48).
Notwithstanding the limitations noted above, this study has several strengths, including the use of national surveillance data. As the survey is distributed among the general population, the findings are more generalizable than data generated from panel or hospital-based surveys. HINTS uses a sampling frame that oversamples minority populations and those who live in Appalachia. This enhances the precision of measurements from minority populations, secondary to larger sample sizes. However, it should be noted since the survey can only be taken in English or Spanish it does not capture minorities with LEP that speak other languages. Additionally, as HINTS is a rich source of data that incorporates a wide variety of sociodemographic variables, we were able to include these in our model of predictors of poor knowledge of palliative care, something that other studies have not been able to do.
In conclusion, this study demonstrated no difference in perceived knowledge about palliative care among immigrant populations in the US compared with non-immigrant populations. These findings should be validated with alternative research approaches in view of the potential biases outlined above. The results however do suggest that more invasive end of life interventions and lower advance care planning among these populations may be related to organizational factors including sub-optimal communication from healthcare teams or individual patient level factors not measured here. Further research is needed to examine potential; underlying causes including communication differences between clinicians and immigrant populations in the context of palliative care to understand why these differences are noted. The high proportion of the overall US population with perceived poor knowledge of palliative care should serve as a catalyst to engage the public (23). Any future action to disseminate knowledge about palliative care should be mindful of the potential differences in education that may contribute to functional and health literacy deficits and therefore understanding about palliative care. The finding that both immigrants and non-immigrants considered health providers to be a reliable source for knowledge about palliative care is encouraging and clinicians should be aware of this as they care for patients and families.
Acknowledgments
The authors wish to thank Dr. Wen-Ying (Sylvia) Chou, Dr. Erin Kent, Dr. Bradford Hesse, for thoughtful insights about Health Information National Trends Survey (HINTS) methodology. HINTS is funded by the National Cancer Institute’s (NCI). The authors would also like to thank Dr. Anthony Windebank for additional feedback and comments.
Funding: This study was supported by Grant Number UL1 TR002377 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the NIH IRB prior to delivery and is a publically available data set that is sufficiently de-identified so as not to require additional IRB approval.
References
- Orom H. Nativity and perceived healthcare quality. J Immigr Minor Health 2016;18:636-43. [Crossref] [PubMed]
- John-Baptiste A, Naglie G, Tomlinson G, et al. The Effect of English Language Proficiency on Length of Stay and In-hospital Mortality. J Gen Intern Med 2004;19:221-8. [Crossref] [PubMed]
- Karliner LS, Kim SE, Meltzer DO, et al. Influence of language barriers on outcomes of hospital care for general medicine inpatients. J Hosp Med 2010;5:276-82. [Crossref] [PubMed]
- Ngo-Metzger Q, Sorkin DH, Phillips RS, et al. Providing high-quality care for limited English proficient patients: the importance of language concordance and interpreter use. J Gen Intern Med 2007;22 Suppl 2:324-30. [Crossref] [PubMed]
- Schenker Y, Karter AJ, Schillinger D, et al. The impact of limited English proficiency and physician language concordance on reports of clinical interactions among patients with diabetes: the DISTANCE study. Patient Educ Couns 2010;81:222-8. [Crossref] [PubMed]
- Linderoth G, Hallas P, Lippert FK, et al. Challenges in out-of-hospital cardiac arrest - A study combining closed-circuit television (CCTV) and medical emergency calls. Resuscitation 2015;96:317-22. [Crossref] [PubMed]
- Harmsen JA, Bernsen RM, Bruijnzeels MA, et al. Patients' evaluation of quality of care in general practice: what are the cultural and linguistic barriers? Patient Educ Couns 2008;72:155-62. [Crossref] [PubMed]
- Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med 2007;22 Suppl 2:283-8. [Crossref] [PubMed]
- Woloshin S, Schwartz LM, Katz SJ, et al. Is language a barrier to the use of preventive services? J Gen Intern Med 1997;12:472-7. [Crossref] [PubMed]
- Flores G, Abreu M, Olivar MA, et al. Access barriers to health care for Latino children. Arch Pediatr Adolesc Med 1998;152:1119-25. [Crossref] [PubMed]
- Kirkman-Liff B, Mondragon D. Language of interview: relevance for research of southwest Hispanics. Am J Public Health 1991;81:1399-404. [Crossref] [PubMed]
- Ferguson WJ, Candib LM. Culture, language, and the doctor-patient relationship. Fam Med 2002;34:353-61. [PubMed]
- Hampers LC, Cha S, Gutglass DJ, et al. Language barriers and resource utilization in a pediatric emergency department. Pediatrics 1999;103:1253-6. [Crossref] [PubMed]
- Manson A. Language concordance as a determinant of patient compliance and emergency room use in patients with asthma. Med Care 1988;26:1119-28. [Crossref] [PubMed]
- Migration Policy Institute. Available online: https://www.migrationpolicy.org/
- Espenshade TJ, Fu H. An Analysis of English-Language Proficiency among U.S. Immigrants. Am Sociol Rev 1997;62:288-305. [Crossref]
- American Community Survey, Detailed Languages Spoken at Home and Ability to Speak English for the Population 5 Years and Over. 2009-2013.
- Stevens G. Age at immigration and second language proficiency among foreign-born adults. Lang Society 1999;28:555-78. [Crossref]
- NIH National Insitute of Aging. US Department of Health and Human Services. 2018. Available online: https://www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care
- NCI Dictionary of Cancer Terms. In: NCI Dictionary of Cancer Terms. NIH National Cancer Institute. 2018. Available online: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/palliative-care?redirect=true
- Ferrell B, Connor SR, Cordes A, et al. The national agenda for quality palliative care: the National Consensus Project and the National Quality Forum. J Pain Symptom Manage 2007;33:737-44. [Crossref] [PubMed]
- Tulsky JA. Improving quality of care for serious illness: findings and recommendations of the Institute of Medicine report on dying in America. JAMA Intern Med 2015;175:840-1. [Crossref] [PubMed]
- Dying in America: Improving Quality and Honoring Individual Preferences Near End of Life. Washington: National Academies Press, 2015.
- O'Neill J, Marconi K. Access to palliative care in the USA: why emphasize vulnerable populations? J R Soc Med 2001;94:452-4; discussion 456-7. [Crossref] [PubMed]
- Paal P, Bükki J. "If I had stayed back home, I would not be alive any more…" - Exploring end-of-life preferences in patients with migration background. PLoS One 2017;12:e0175314. [Crossref] [PubMed]
- NIH. MedlinePlus. In: US National Library of Medicine. Available online: https://medlineplus.gov/languages/palliativecare.html
- Prabhu AV, Crihalmeanu T, Hansberry DR, et al. Online palliative care and oncology patient education resources through Google: Do they meet national health literacy recommendations? Pract Radiat Oncol 2017;7:306-10. [Crossref] [PubMed]
- Yarnell CJ, Fu L, Manuel D, et al. Association Between Immigrant Status and End-of-Life Care in Ontario, Canada. JAMA 2017;318:1479-88. [Crossref] [PubMed]
- Barwise A, Jaramillo C, Novotny P, et al. Differences in Code Status and End-of-Life Decision Making in Patients With Limited English Proficiency in the Intensive Care Unit. Mayo Clin Proc 2018;93:1271-81. [Crossref] [PubMed]
- Searight HR, Gafford J. Cultural diversity at the end of life: issues and guidelines for family physicians. Am Fam Physician 2005;71:515-22. [PubMed]
- Harhay MO, Halpern SD. End-of-life care among immigrants: Disparities or differences in preferences? JAMA 2017;318:1448-9. [Crossref] [PubMed]
- Health Information National Trends Survey. Available online: https://hints.cancer.gov/
- Nelson DE, Kreps GL, Hesse BW, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. J Health Commun 2004;9:443-60; discussion 81-4. [Crossref] [PubMed]
- Westat. Health Information National Trends Survey 5. Available online: https://hints.cancer.gov/data/methodology-reports.aspx
- Rugno FC, Paiva BS, Nunes JS, et al. "There won't' be anything else..it's over": perceptions of women referred to palliative care only. Eur J Oncol Nurs 2014;18:261-6. [Crossref] [PubMed]
- Evans N, Meñaca A, Andrew EV, et al. Appraisal of literature reviews on end-of-life care for minority ethnic groups in the UK and a critical comparison with policy recommendations from the UK end-of-life care strategy. BMC Health Serv Res 2011;11:141. [Crossref] [PubMed]
- Elkan R, Avis M, Cox K, et al. The reported views and experiences of cancer service users from minority ethnic groups: a critical review of the literature. Eur J Cancer Care (Engl) 2007;16:109-21. [Crossref] [PubMed]
- Firth S. Wider horizons: care of the dying in a multicultural society. National Council for Hospice and Specialist Palliative Care Services London; 2001.
- Gunaratnam Y. Ethnicity, Older People and Palliative Care: A Joint Publication from the Policy Research Institute on Aging and Ethnicity and the National Council for Palliative Care. Available online: https://www.priae.org/assets/palcope/National_Council_for_Palliative_Care.PDF
- Broom A, Good P, Kirby E, et al. Negotiating palliative care in the context of culturally and linguistically diverse patients. Intern Med J 2013;43:1043-6. [Crossref] [PubMed]
- Meghani SH, Hinds PS. Policy brief: the Institute of Medicine report Dying in America: Improving quality and honoring individual preferences near the end of life. Nurs Outlook 2015;63:51-9. [Crossref] [PubMed]
- Silveira MJ, DiPiero A, Gerrity MS, et al. Patients' knowledge of options at the end of life: ignorance in the face of death. JAMA 2000;284:2483-8. [Crossref] [PubMed]
- Jarvis P, Wilson AL. International dictionary of adult and continuing education. London: Psychology Press, 1999.
- Volandes AE, Paasche-Orlow M, Gillick MR, et al. Health literacy not race predicts end-of-life care preferences. J Palliat Med 2008;11:754-62. [Crossref] [PubMed]
- Chronic Conditions in America: Price and Prevalence In: RAND review. Available online: https://www.rand.org/blog/rand-review/2017/07/chronic-conditions-in-america-price-and-prevalence.html
- Sun A, Bui Q, Tsoh JY, et al. Efficacy of a Church-Based, Culturally Tailored Program to Promote Completion of Advance Directives Among Asian Americans. J Immigr Minor Health 2017;19:381-91. [Crossref] [PubMed]
- Bullock K. Promoting advance directives among African Americans: a faith-based model. J Palliat Med 2006;9:183-95. [Crossref] [PubMed]
- Dumanovsky T, Augustin R, Rogers M, et al. The Growth of Palliative Care in U.S. Hospitals: A Status Report. J Palliat Med 2016;19:8-15. [Crossref] [PubMed]


