
Dying well with diabetes
Introduction
Dying is an inevitable part of living. How death is experienced is important for the individual, their family and carers and the healthcare professionals who provide care. Much has been written on the palliative care needs at the end of life (1-3). Such guidance is generic and co-existing conditions such as diabetes are not always addressed. In the United States (US), studies decry the lack of quality palliative care for people with conditions such as frailty, cardiopulmonary failure, and end stage renal disease compared with those with dementia or cancer (4). While diabetes is not included in the US article, diabetes complications include cardiovascular disease and renal disease. National consensus guidance on diabetes and end of life was first published in Australia in 2010 (5). National guidance for the care of people with co-morbidities such as diabetes was recommended in 2013 in the United Kingdom (UK); this report demanded condition specific recommendations (6). At that time, “diabetes specific” consensus UK guidance had already been published and was accessible to all health care professionals (7). The American Diabetes Association published a short position statement [2017] on medical standards for adults end of life care giving a summary of recommendations (8). In addition, the International Diabetes Federation made recommendations for end of life care aligned to the UK consensus guidance in 2013 (9).
In the UK, despite up to 74% of individuals expressing a wish to die at home, 58% die in the hospital setting (10). Over half a million people die every year (1), of these around 75,000 will have diabetes (11). Most will not die as a result of acute diabetes complications but of other comorbidities associated with the condition such as, cancer, stroke, respiratory disease, or cardiovascular disease (12). A variety of healthcare professionals will care for these individuals; they will have differing levels of skills, training, and competence in the management of diabetes in the dying and so guidance and clear recommendations is important. This article provides practical guidance on the care of dying people with diabetes (11).
When does the “end of life” begin?
The General Medical Council (GMC) advises that people are approaching “end of life” when they are likely to die within the next 12 months stating that:
“This includes people:
- Whose death is imminent (expected within a few hours or days);
- With advanced, progressive, incurable conditions;
- With general frailty and co-existing conditions that mean they are expected to die within 12 months existing conditions;
- Who are at risk of dying from a sudden acute crisis in their condition;
- With life-threatening acute conditions caused by sudden catastrophic events.” (13).
The GMC describes the most challenging ethical areas as being whether to withdraw medications or fluids, while acknowledging that there needs to be consideration into the risk/benefit of continuing or stopping these (13).
How do health care professionals know if a person can be said to be in the last year of life?
If an individual has a terminal illness for example, advanced stages of cancer, the prognosis and expected time to live may be recorded in the individuals’ notes. For many people with other conditions there may be no indication of prognosis. The Gold Standard Framework whilst not diabetes specific for end of life identifies three factors that can aid in determining this (14):
- The surprise question;
- General indicators of decline and increasing needs;
- Specific clinical indicators.
The surprise question
When considering whether the person is in the last year of life and after assessing clinical, social and other elements; health care professionals (HCP) should ask themselves, “For patients with advanced disease or progressive life limiting conditions, would I be surprised if the person were to die in the next year, months, weeks, days?”
If the HCP would not be surprised then this can be used to address future measure to support quality of life and if there is further decline.
General indicators of decline and increasing needs
There are many factors than assist the HCP in determining whether end of life care is needed (Table 1).

Full table
Specific clinical indicators
These relate to the specific conditions such as, heart disease and stroke, chronic obstructive pulmonary disease (COPD), liver disease, renal failure, frailty, cancer, and dementia. Diabetes is not included although people with the aforementioned but frequently occur in combination with those listed.
The Framework defines four main phases of illness:
- Stable from diagnosis (usually lasting years);
- Unstable, advanced disease (usually lasting months);
- Deteriorating, exacerbations (usually lasting weeks);
- Last days of life (usually lasting days) (14).
End of life care in diabetes
The Diabetes UK End of Life Clinical Care Recommendation document was updated in 2018 (11). It was acknowledged in the initial guidance that there was a dearth of evidence supporting diabetes care at that time and this is still the same today. The 3rd edition of the original document was required because of changing developments in policy for end of life care and the need to address special populations of those with diabetes. Newer therapies to control blood glucose had been reviewed and approved by the UK National Institute for Clinical and healthcare Excellence (NICE) (15,16) including insulin and non-insulin preparations, and the authors wanted to respond to the many constructive comments and feedback from practising clinicians in the field about the earlier revisions.
The document was developed for all HCPs working in the health and social care setting caring for people with diabetes and families during the last year of life. The recommendations aimed to ensure a consistent quality approach to care accompanied by a set of standards, and emphasise the importance of workforce as well as encouraging partnership working within established palliative care planning.
Planning for end of life
The overriding principle of any care offered is to “first do no harm” as described by Thomas Inman in 1860 (17). Each time an individual is treated there is a risk of causing harm and this is no less true in diabetes management. Acknowledging that some individuals may not wish to know that they are entering the last stages in life; some who have capacity and wish to management their diabetes for as long as they are able should be enabled to discuss and decide on treatment options. These should include blood glucose monitoring, potential drug side effects and what treatments they would prefer to have or be discontinued should their health deteriorate. When individuals are nearing the end of their lives this capacity may be impaired or absent. The development of care planning documents such as “Advance Directives” can enable this discussion to take place much earlier. There are three types of advance planning documents in the UK (11):
- An advance decision: this document is legally binding—it should be signed and witnessed. It informs all those involved in the individual’s care e.g., family, carers, health professionals, that the individual has a specific wish to refuse specific treatments in the future and this becomes essential if that individual loses the ability to communicate effectively.
- An advance statement: this document is not legally binding but sets out the individuals’ wishes, preferences and beliefs about future care.
- Emergency Health Care Planning (EHCP): an EHCP makes communication easier in the event of a healthcare emergency. It includes shared decision making and recording around expectations and capabilities of the individual and carers in the event of predictable situations or emergencies. The plan should include a list of regular and PRN medications, and indications for any rescue medications left in the individual’s home for emergency use. It could include a plan for insulin adjustment or rescue doses of short acting insulin analogues.
It is important that individuals are able to consider using these tools while they still have capacity and that, families, carers and the general practitioner are aware of their existence.
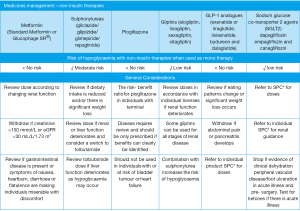
Clinical care recommendations
Throughout the life of a person living with diabetes they are encourage to meet specific clinical targets such as those required for blood glucose, blood pressure and lipids as defined by NICE and the American Diabetes Association (15,16,18). These targets are recommended in order to avoid acute and long-term complications. When individuals are in the last year of life these targets can be relaxed as the aim would then be to provide symptomatic relief from hypo or hyperglycaemia rather than tight glycaemic control. In glycaemia management it is important that the relaxation of any clinical targets be discussed with the individual, their families and or carers, as some may perceive this change as demonstrating that the HCP is “giving up on them”. They may also wish to continue with their usual glucose targets so any care plan would need to be a joint decision.
Blood glucose targets in the last year of life are recommended as capillary blood glucose readings of between 6.0–15.0 mmol/L. If the readings are kept between these parameters there will be a low risk of hypoglycaemia (blood glucoses readings below 4.0 mmol/L) and of overt hyperglycaemia that could lead to acute metabolic diabetes complications such as:
- Diabetic ketoacidosis (DKA) in people with type 1 diabetes (15). People with type 2 diabetes treated with SGLT2 inhibitors are also at risk of developing euglycaemic DKA especially when they are unwell or dehydrated (19).
- Hyperosmolar hyperglycaemic state (HHS) in those presenting with newly diagnosed type 2 diabetes or people already diagnosed with type 2 diabetes or in (20).
Equally important is the feeling of wellbeing if glycaemic levels are kept between those recommended, as lower blood glucose readings will lead to hypoglycaemic symptoms and raised blood glucose readings to hyperglycaemic symptoms such as thirst, tiredness and dehydration.
Blood glucose monitoring
As the individual passes through the latter stages of the dying process, blood glucose testing may become less important, it is important to determine the individual preferences in this area of care. In type 1 diabetes, testing will need to be continued once or twice a day to rule out hypoglycaemia or overt hyperglycaemia leading to DKA. In type 2 diabetes, often most glucose lowering treatments will have been discontinued so testing may not be necessary unless the individual is taking a medication that can result in hypoglycaemia such as a sulphonylurea or insulin.
Hypoglycaemia
Hypoglycaemia, where the blood glucose is recorded as less than 4 mmol/L presents challenges in the care of people in end of life and impacts adversely on quality of life. Every effort should be made to minimise the risk of hypoglycaemia; this include reductions or changes in diabetes medications, relaxation of glycaemic targets and relaxing of food restrictions. Strict avoidance of added glucose foods is not required if food choices or appetites are diminished.
Individuals at higher risk of hypoglycaemia include those who are said to have:
- Frailty;
- Dementia/cognitive impairment;
- Nutritionally depleted/anorexic;
- Nauseated or vomiting;
- Renal impairment;
- Liver impairment;
- Treated to “tight” glycaemic targets;
- Treated with sulphonylurea agents;
- A previous gastrectomy;
- Treated with insulin.
The signs and symptoms of hypoglycaemia are shown in Table 2 but it should be noted that signs and symptoms of hypoglycaemia can be atypical in older people; they usually present with more cognitive symptoms such as confusion (21).
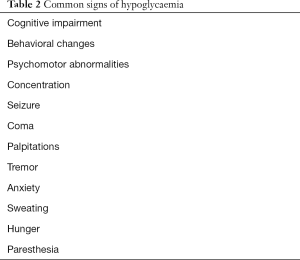
Full table
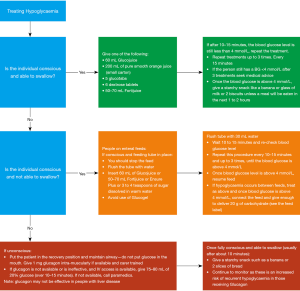
The treatment of hypoglycaemia is shown in Figure 1.
Nutrition
Changes in meal sizes and long gaps between meals impact on the management of diabetes and loss of appetite. Perhaps more importantly it is often of great concern to the individual and their carers. Eating is a very social activity and helps people feel better; loss of appetite may mean the person loses part of this interaction and enjoyment (22). Chemotherapy is recognised to lead to nausea and vomiting in some instances but one side effect not always considered is the change in taste it can bring. In these cases small meals with little or no restriction in those with added sugars can help. Calorie dense food such as chocolate is also encouraged. Some individuals will prefer cold meals if they are nauseated. Dietetic review in useful in these circumstances and advice should be sought. If there is difficulty is swallowing diabetes medications and raised blood glucose levels are causing hyperglycaemia (23), repaglinide a very short acting medication can be used in those with type 2 diabetes or low dose insulin in people with type 1 and in type 2 diabetes (16).
Medicines management in type and type 2 diabetes
Type 1 diabetes
People with type 1 diabetes require insulin for life. These individuals will probably have been taking insulin for many years. Where possible they should be supported to manage their own self-blood glucose testing and administer their own insulin. This will depend on capacity and dexterity. It may be that whereas an individual could usually competently manage insulin adjustment or, for example an insulin pump or pen device; in the later stages of the dying process they may need to be changed to a different insulin device or regimen or a third party may need to administer the insulin.
Without insulin people with type 1 diabetes will rapidly develop diabetic ketoacidosis, a condition characterised by severe dehydration, acidosis, and blood glucose readings usually above 20.0 mmol/L. The symptoms of DKA are unpleasant and to be avoided at all times. Therefore insulin treatment can never be discontinued in these individuals even if they are not able to eat or drink. Insulin doses can often be significantly reduced however with individuals only requiring a daily dose of long acting insulin in the last few weeks and days of life. The treatment of choice would be once-daily long-acting insulin such as insulin glargine or insulin degludec (11).
Type 2 diabetes
People with type 2 diabetes are often taking a plethora of medications to treat blood pressure, hyperlipidaemia and blood glucose. Many of these can be discontinued or reduced depending on the dying phase. Table 3 offers a comprehensive guide aligned to the Gold Standards Framework (14). Medications such as sulphonylureas and insulin have a higher risk of hypoglycaemia (24) as both are reliant on regular nutrition to prevent hypoglycaemia. Renal impairment also leads to poor excretion of insulin and sulphonylureas so hypoglycaemia is more common. These glucose-lowering agents should be avoided in these individuals and particularly when appetite is poor and there is weight loss. Insulin can often be discontinued in individuals with type 2 diabetes. Other glucose lowering agents and the risk of hypoglycaemia is shown in Figure 2. A guide to insulin management in type 1 and type 2 diabetes is shown in Table 4.
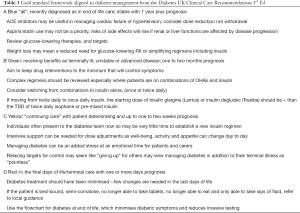
Full table

Full table
If blood glucose readings remain high in people with type 2 diabetes they may become at risk of hyperosmolar hyperglycaemic state (HHS), a condition characterised by severe dehydration, an osmolality of more than 320 mmHg, and blood glucose readings more than 40 mmol. Mortality rates are high in people with HHS but the condition is relatively rare and usually only found in older fail people with diabetes who are treated with either diet or diet and metformin and in those taking corticosteroid therapy (25).
Diabetes and steroid therapy
Steroid treatments are often used in palliative care for symptom control. The most commonly used are prednisolone or dexamethasone. Steroids can cause hyperglycaemia and its associated symptoms in those known to have diabetes and in those without a previous diagnosis on diabetes. Once daily steroid treatment taken in the morning will usually cause a substantial rise in blood glucose in the late afternoon or early morning. This can be managed by the use on a sulphonylurea such as Gliclazide or a basal insulin such as Humulin I®, Insulatard® or Insuman Basal® administered in the morning (21) (Figure 3). Early discussions with a member of the diabetes specialist team can help with the planning of a suitable regimen to manage glucose excursions (25).

When to withdraw treatment
A simple flowchart for diabetes management is shown in Figure 4.

Fluids
The withdrawal of fluids is controversial. Fluids should not be withdrawal unless it is the expressed wish of the individual, if they lack the capacity to decide this then family and or carers should be consulted (6).
There is no evidence to support whether the withdrawal of fluids will hasten death or that the offering of clinical rehydration prolongs life. If the individual is demonstrating marked signs and symptoms of dehydration such as thirst, delirium or inability to speak because of dry mouth a therapeutic trail of clinically assisted rehydration should be considered and the individual reviewed over a 12-hour time span. If there are signs of harm including fluid overload or if the person requests that they no longer wish for fluids they should be discontinued (11).
Diabetes treatments
When the individual is entering the last phases of life, withdrawal in whole or in part of diabetes treatments should be considered if:
- Frequent treatment related hypoglycaemia is causing distress or significant management difficulties;
- Where the continuing of food or fluids are not the choice of the individual;
- Where the benefits of stricter glycaemic control cannot be justified (11);
Factors than can influence this decision are: advance care planning, concerns by family of a euthanasia approach, and the individuals’ preferences and wishes.
Insulin treatment should not be stopped in people with type 1 diabetes.
Staff competencies
It is important that all staff including those who do not work in specialist care have the knowledge and skills needed to manage people in end of life care (6,11). Nursing competencies for the care of people with diabetes in end of life care are available in the UK (26).
Summary of recommendations
Diabetes impacts on every facet of life in the person living with diabetes and this included when that individual is dying. The management of diabetes and the associated risks and side effects related to diabetes can complicate the dying process and make the experience more difficult and unpleasant. Simple measure can be put into place to ensure that the diabetes does not get in the way of a peaceful death; staff need to be trained and competent in the management of diabetes to ensure that this final act of caring is in place.
Dame Tessa Jowell; a British Member of Parliament has the last word when she stated in the House of Lords just prior to her death from cancer in May 2018 (27), “In the end, what gives a life meaning is not only how it is lived, but how it draws to a close”.
Acknowledgements
Dr. Rob Gregory, Dr. Jean MacLeod, Dr. James Burton, Professor Alan Sinclair.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- National Institute for Health and Clinical Care Excellence (NICE) Clinical Care Summaries, Palliative Care: General Issues. Available online: https://cks.nice.org.uk/palliative-care-general-issues#!topicsummary. 2016. Accessed 6/5/18.
- National Institute for Health and Clinical Care Excellence, NICE, Quality standards for End of Life care in Adults (QS13). Available online: https://www.nice.org.uk/guidance/qs13/chapter/Introduction-and-overview. Updated 2017 Accessed 6/5/18.
- Winston WT, McMillan JM. Palliative Cancer Care Guidelines. Available online: https://emedicine.medscape.com/article/2500043-overview. 2017, accessed 6/5/18.
- Wachterman MW, Pilver C, Smith D, et al. Quality of end of life care provided to patients with different serious diseases. JAMA Intern Med 2016;176:1095-102. [Crossref] [PubMed]
- Trisha Dunning Peter Martin Sally Savage Nicole Duggan Guidelines for Managing diabetes at the end of life, 2010. Available online: file:///Users/June/Desktop/Master%20folder%20Dropbox/Managing_Diabetes_at_the_End_of_Life_-_Guidelines[1].pdf. Accessed 5/1/18.
- Department of Health, More care less pathway: an independent review of the Liverpool Care Pathway, 2013. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/212450/Liverpool_Care_Pathway.pdf. Accessed 6/5/18.
- Diabetes UK. End of life diabetes care: full strategy document 2nd ed. 2012. Available online: http://www.leicestershirediabetes.org.uk/uploads/documents/V2EOL_Full_Doc.pdf. Accessed 6/5/18.
- American Diabetes Association. Older adults: Standards of Medical Care in Diabetes—2018. Diabetes Care 2018;41:S119-25. [Crossref] [PubMed]
- International Diabetes Federation; Global guideline for managing diabetes in older people with type 2 diabetes. Available online: file:///Users/June/idf-guideline-older-people-T2D.pdf. Accessed 6/5/18.
- The National Council for Palliative Care, What people want to live and die well, 2011. Available online: http://www.ncpc.org.uk/sites/default/files/NCPC_Future_Forum_Evidence_May_2011.pdf. Accessed 13/5/18.
- Diabetes UK. End of life diabetes care, 3rd Ed. Available online: https://diabetes-resources-production.s3.eu-west-1.amazonaws.com/resources-s3/2018-03/EoL_Guidance_2018_Final.pdf. Accessed 6/11/18.
- World Health Organisation. The top 10 causes of death, 2017. Available online: http://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed 1/11/18.
- General Medical Council, GMC, Treatment and care towards the end of life: good practice in decision making. Available online: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/treatment-and-care-towards-the-end-of-life/guidance. Accessed 6/5/18.
- The Gold Standards Framework, Proactive Identification Guide. Available online: file:///Users/June/NEW%20PIG%20-%20%20%20Updated%2010.8.17%20KT%20vs17.pdf. Accessed 6/5/18.
- National Institute for Heath and Care Excellence, NICE NG 17, 2015, Type 1 Diabetes: Diagnosis and management. Available online: https://www.nice.org.uk/guidance/ng17. Accessed 13/5/18.
- National Institute for Heath and Care Excellence, NICE NG 28, Type 2 diabetes in Adults, 2015. Available online: https://www.nice.org.uk/guidance/ng28. Accessed 13/5/18.
- Inman T. Foundation for a New Theory and Practice of Medicine. London, UK: John Churchill, 1860.
- American Diabetes Association, Medical standards of care indiabetes. 2018. Available online: http://care.diabetesjournals.org/content/diacare/suppl/2017/12/08/41.Supplement_1.DC1/DC_41_S1_Combined.pdf. Accessed 7/11/18.
- Diabetes UK. Position Statements, The management of diabetic ketoacidosis in Adults, 2013, 2nd ed. Available online: http://www.diabetologists-abcd.org.uk/JBDS/JBDS_IP_DKA_Adults_Revised.pdf. Accessed 22/5/18.
- Scott AR. Management of hyperosmolar hyperglycaemic state in Adults with diabetes, 2015, Diabetic Medicine. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/dme.12757. Accessed 23/5/18.
- Abdelhafiz AH, Rodríguez-Mañas L, Morley JE, et al. Hypoglycaemia in Older People - A Less Well Recognized Risk Factor for frailty. Aging Dis 2015;6:156-67. [Crossref] [PubMed]
- Dunbar RIM. Breaking bread: the functions of social eating. Adaptive Human Behavior and Physiology 2017;3:198-211. [Crossref]
- Thomas R. Nutritional support for the dying or severely demented patients MSD Manual Professional Version, 2018. Available online: https://www.msdmanuals.com/en-gb/professional/nutritional-disorders/nutritional-support/nutritional-support-for-dying-or-severely-demented-patients. accessed 6/11/18.
- British National Formulary, BNF. Available online: https://bnf.nice.org.uk/. Accessed 13/5/18.
- Diabetes UK. Position Statements Management of hyperglycaemia and steroid (glucocorticoid) therapy: a guideline from the Joint British Diabetes Societies –for Inpatient Care Group (JBDS-IP). doi: 10.11/dme.13675. Accessed 19/7/18.
- TREND-UK. An integrated career and competency framework for diabetes nursing 4th ed., 2015. Available online: www.trend-uk.org.uk. Accessed 6/11.18.
- Statesman N, Jowell T. May 2018. Available online: https://www.newstatesman.com/politics/health/2018/01/tessa-jowell-1947-2018-end-what-gives-life-meaning-not-only-how-it-lived-ho. Accessed 13/5/18.w


