Strengthening palliative care delivery in developing countries: a training workshop model in Botswana
Introduction
Palliative care is a discipline of medicine that aims to provide holistic care to both patients facing life-threatening illness, and also their families. Significant improvement in patients’ quality of life has been observed when palliative care is implemented both at the onset of disease diagnosis and at later stages of disease (1). In 2005, the World Health Organization (WHO) estimation of the need for palliative care was approximately 9.67 million people across Africa (2); however, only 14% of people needing palliative care at the end of life worldwide currently receive it. Despite the increasing prevalence and burden of cancers (3) and other chronic illnesses in Sub-Saharan Africa, the establishment of palliative care services in this region has lagged behind that of other regions (4). In 2014 the World Health Assembly created a global resolution on palliative care, declaring palliative care an essential health service (5). While some sub-Saharan African countries such as Uganda (6) and South Africa (7) have successfully imbedded palliative care into their health care system, palliative care remains in its infancy in Botswana and other countries (8). In 2013 the Botswana Ministry of Health (MOH) launched the National Palliative Care Strategy to build the necessary infrastructure for nationwide provision of palliative care. At present, palliative care primarily exists in the inpatient setting in Botswana. In addition, non-governmental organizations (NGOs) such as Holy Cross Hospice in capital city of Gaborone, provide outpatient support to cancer patients and those living with HIV. Due to the limited geographic scope of these isolated efforts, there remains a significant need for palliative care services throughout the country.
In order for palliative care to be integrated into the current health system in Botswana, ongoing education and training is needed for care providers. In the current study, we provide a model for nursing palliative care training through analysis of a workshop designed to provide basic palliative care education to nursing staff without prior formal training.
Methods
The workshop took place over 2 days on October 6–7th, 2014 in Gaborone, Botswana. Invitations were sent to the public oncology center and a local hospice. Fifteen nurses were ultimately able to attend, with eleven coming from the public oncology center.
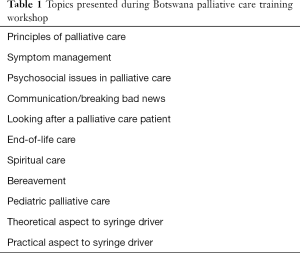
The workshop consisted of blocks of 1-hour sessions. Expert physicians and nurses taught select topics in palliative care (Table 1). Faculty included a palliative care and hospice trained physician from Botswana, a doctorally prepared nurse from the University of Botswana, and a nurse practitioner with expertise in palliative care from the United States. One session was dedicated entirely to morphine administration, during which participants had the opportunity to practice operating syringe drivers, which enable continuous subcutaneous administration.
Full table
A pre-test was administered prior to the start of the workshop. The test was composed of 21 questions. Eighteen questions were in multiple choice format, while the remaining 3 were open-ended questions. A post-test composed of the same 21 questions was administered at the end of the workshop. A copy of the test is included in Supplementary material.
Because this study contained no patient protected health information and did not involve direct patient care, it was exempt from Institutional Review Board approval.
Statistical analysis
Of the 15 participants at the workshop, 10 completed a pre-test and post-test. Five participants did not complete a pre-test and were excluded from statistical analysis. Data analysis was performed using SPSS version 23. Paired sample t-tests were used to compare the average pre-test and post-test scores. Descriptive analysis (average score) was utilized when test questions were divided into subcategories.
Results
There was a statistically significant difference (P=0.001) between the average pre-test score (46.18%) and the average post-test score (64.27%), with 9 out of 10 participants having a higher average post-test than pre-test score. When individual questions were analyzed, the average post-test score was higher than the average pre-test score for 12 questions, lower for 4 questions, and without difference for five questions (Table 2). When questions were divided into subcategories, the most significant improvement in the post-test score average was seen for questions pertaining to communication, end of life, and syringe driver use (Table 2).

Full table
Discussion
With a statistically significant increase of 18% in pre- and post-test scores, and 90% participant improvement in pre- and post-test results, significant improvement in nurses’ knowledge of palliative care principles appears to have resulted from the 2-day workshop we have reported.
One of the categories with the highest improvement was end of life care, with a 36% difference in average pre- and post-test scores. Questions on the syringe driver had the highest post-test average of 92.5%, compared to a pre-test average of 62.5%. The success of the syringe driver session can be largely attributed to the comprehensive material provided by the workshop speakers. Secondly, the effect of the practical section of this session must not be overlooked. Participants were given the opportunity to gain hands on experience with the syringe driver—a training component that likely contributed to the high post-test average score.
Questions on the principles of palliative care were the highest scoring pre-test category at 70% correct responses. The high scores observed in this category are likely secondary to the pre-selected population of nurses who attended the workshop, as they are more apt to have an interest in and some exposure to palliative care. This finding is reassuring, as it suggests that nurses have a baseline understanding of palliative care, despite its infancy in Botswana.
Notably, one category with no improvement in pre- to post-test scores tested the participants’ ability to convert long acting morphine to an appropriate short acting morphine dose. Pain management is a cornerstone of palliative care; therefore, opioid titration and conversion is a critical skill for nurses providing it. Given the scarcity of palliative care trained physicians and the need for interdisciplinary care for this population, nurses must be comfortable with opioid management as they are the front-line providers of pain medication. Emphasis on opioid management is an essential component of palliative care training that must be addressed in future workshops. Education regarding opioids is known to have a positive impact on misinformed and often prevalent beliefs about such medications. Increased knowledge may not only help to dispel misunderstanding but also decrease opioid withholding due to fear of patient harm.
While only one question on spirituality was tested, it had one of the lowest post-test scores. It is difficult to assess the significance of this finding given the limited data available. More questions on spirituality should be included in future testing, as the prevalence of participation in religious services or activities in Botswana makes spirituality an important aspect of palliative care in the country. Several studies conducted in sub-Saharan Africa have found that spiritual distress noticeably impairs quality of life, while spiritual support is capable of improving palliative and end of life experiences for both patients and their loved ones (9).
Nevertheless, several limitations existed in this study, the first of which is small sample size. Only 15 nurses participated in the workshop, and of this number, only 10 completed both a pre-test and post-test. Data from 5 of the participants was unable to be used, eliminating one third of the initial sample size. While there were differences seen in the pre-test and post-test scores in our analysis, some of the results were not statistically significant given the sample size. As previously mentioned, participation in the workshop was voluntary; thus, the nurses who attended were more likely to have established interest in and prior exposure to palliative care. The pre-test scores therefore may have been influenced by this baseline knowledge, potentially minimizing the difference observed in the pre-test and post-test averages.
Palliative care training for nurses has been identified as a means to address the insufficient number of trained clinicians in the field, and the persistently unmet palliative care need that has resulted. Training of link-nurses in palliative care is one way to utilize nurses in this field, as described in a recent study in Mulago Hospital in Uganda (10). Link-nurses received concentrated training in the basics of palliative care and were stationed in different wards to provide palliative care training, in addition to routine nursing care. After less than 2 years of implementation, the number of patients receiving palliative care services increased from 611 to 1,788. The link-nurses cared for approximately 75% of patients needing palliative care while the remaining 25%, who required more complex care, were referred to the specialist palliative care team (10). Using the workshop, we have described as core training for nurses could provide a framework to trial such utilization of link-nurses in Botswana.
Conclusions
Training of nurses in core principles of palliative care is essential to achieving the goal of providing care to all patients in Botswana in need of palliative services. Basic training and continued education on palliative care should be integrated as a routine element of all undergraduate medical and nursing education, and as part of in-service training of caregivers at the primary care level, including health care workers, caregivers addressing patients’ spiritual needs and social workers. Intermediate training should be offered to all health care workers who routinely work with patients with life-threatening illnesses, including those working in oncology, infectious diseases, pediatrics, geriatrics and internal medicine. Our study demonstrated that knowledge of topics in palliative care significantly improved among nurses after a 2-day workshop. Further training in palliative care will provide these nurses with the skill set and resources they need to successfully deliver palliative services to patients at their clinical sites.
- Opioid use at end-of-life:
- Is rarely needed, except for patients with metastatic cancer;
- Frequently prevents patients from relating to loved ones;
- Is precluded if an intravenous device cannot be placed or maintained;
- Should be minimized to avoid the possibility of “hastening death”;
- Can be used to manage increased work of breathing.
- A woman with metastatic pancreatic cancer is losing weight and spending >75% of time in bed or lying down, no further anti-neoplastic treatments are planned. The patient asks you: “How much time do you think I have?” The best approach is to say:
- “I believe time is short, only a few weeks to a few months”;
- “I really can’t tell how much time you have left”;
- “Life is mystery, you must not give up hope”;
- “On average patients with your condition live for about six-nine months”;
- “Only God can determine how long someone has to live”.
- A long-term patient of yours comes to see you 3 months after the death of his wife. He says that he sometimes thinks that his wife is in the house talking with him, that he imagines he hears her voice; he has gained 10 pounds since her death, but otherwise feels well. Concerned that he is “going crazy”. These symptoms are most consistent with:
- Complicated grief reaction;
- Major depression;
- Minor depression;
- Normal grief reaction;
- Psychotic disorder.
- A patient has been taking 60 mg of long-acting morphine (MST) every 12 hours and an additional 40 mg of PRN doses of short acting morphine. You want to start him on an equivalent dose of a subcutaneous morphine infusion; how much morphine would you give?
- 60 mg;
- 30 mg;
- 80 mg;
- 120 mg;
- 160 mg.
- A 67-year-old man with prostate cancer has increasing pain over the left hip over the past six weeks requiring increasing doses of opioid analgesics. The pain is constant, aching, and well localized; there is no referred pain. Pain in this patient most likely represents:
- Drug seeking behavior;
- New onset depression;
- Opioid addiction;
- Opioid tolerance;
- Worsening metastatic cancer.
- The primary source of assessment of pain in a patient should be:
- Abnormal vital signs;
- Physical exam findings;
- Patient’s self-report of pain;
- Patient’s facial grimacing;
- Physician’s perception of patient’s pain.
- A patient has had good pain control with regular doses of morphine. He is now unconscious and near death and has begun to moan and be restless. You should administer:
- Oxygen;
- Morphine;
- Hyoscine butylbromide (buscopan);
- Midazolam;
- Fluids.
- Which one of the following statements about the dying process is most accurate?
- Active dying is characterized by depression, tachypnea and polyuria;
- Imminent death is heralded by delirium, tachycardia and warm extremities;
- “Bubbly” or “gurgling” respirations are distressing to patients and require suctioning;
- Physical signs and symptoms allow reliable prediction of when death will occur;
- Signs and symptoms related primarily to decreasing circulation.
- The single most important supplemental therapy to consider when starting patients on opioids for pain is:
- Steroids to increase alertness;
- Antidepressants to supplement pain relief;
- Antiemetic to treat nausea;
- Laxative (bisacodyl or liquid paraffin) to prevent constipation;
- Ibuprofen to treat inflammation.
- The single best predictive factor determining prognosis in patients with metastatic cancer is:
- Functional ability;
- Number of metastatic lesions;
- Presence of brain metastasis;
- Serum albumin;
- Severity of pain.
- Spirituality is best defined as a person’s understanding of:
- Heaven and hell in the context of imminent death;
- How a higher being values life accomplishments;
- The origins of life and the universe;
- Their relationship between one’s self, others and the universe;
- Their religious traditions and rituals.
- WHO defines palliative care as?
- Care that prevents or alleviate the symptoms of disease without a cure;
- A program of care in a variety of settings that supports the patient and family through the dying process;
- An approach which improves the quality of life of patients and their families facing life-threatening illness or progressive, incurable illness;
- Care that supports favorable outcomes of end-of-life care.
- The primary goals of palliative care include all of the following except:
- Relieving pain and distress;
- Eliminating invasive diagnostic procedures;
- Promoting autonomy;
- Enhancing the quality of patients’ lives.
- Which of the following statements is not true about palliative care?
- Palliative care can only be offered in a hospice setting;
- Palliative care uses a team approach;
- Use of effective communication is integral to palliative care;
- Palliative care affirms life and regards dying as a normal process.
- Name a way to assess pain severity in a 5-year-old child.
- Name 3 ways children communicate.
- At what age do children understand death is permanent, irreversible, and universal?
- Your patient Mrs. Smith has a syringe driver in situ. Her symptoms have been well-controlled, however, she is now complaining of an exacerbation of her symptoms. Possible reasons may include:
- Syringe driver malfunction;
- Medications require review for effectiveness;
- Mrs. Smith’s condition is changing or deteriorating;
- All of the above.
- Mrs. Smith’s infusion finishes 2 hours early. Possible explanations include:
- Incorrect volume (less than required) added to syringe during preparation;
- Failure to account for infusion volume required to prime the tube;
- Syringe driver rate incorrect;
- All of the above.
- Mr. Boot is concerned that the subcutaneous infusion may not manage his pain. What information would you give him to reassure him about this?
- A syringe driver will always manage pain, and no other medication will be necessary;
- If a syringe driver fails to manage his pain, little can be done about this;
- If pain occurs, breakthrough medication can be administered;
- No more pain medication can be given due to possible side effects.
- Regular patient assessment should include:
- Effectiveness of symptom management;
- Site inspection/assessment;
- Checking patency of tubing and syringe volume remaining;
- All of the above.
Pre- and Post-test Palliative Care Workshop 6–7th October 2014
Pediatric palliative care
Syringe driver questions
Acknowledgements
The authors would like to thank the Department of Radiation Oncology at the University of Pennsylvania for providing travel and salary support for one of the workshop faculty members.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Bain LE. Are we doing enough for our patients with terminal cancer? A moral imperative to step up palliative care practice in Sub-Saharan Africa. BMJ Support Palliat Care 2015;5:467-8. [Crossref] [PubMed]
- Abratt RP, Vorobiof DA. Cancer in Africa. Lancet Oncol 2003;4:394-6. [Crossref] [PubMed]
- Grant L, Downing J, Namukwaya E, et al. Palliative care in Africa since 2005: good progress, but much further to go. BMJ Support Palliat Care 2011;1:118-22. [Crossref] [PubMed]
- Sixty-Seven World Health Assembly. Strengthening of Palliative Care as a Component of Comprehensice Care Throughout the Life Course. 2014:1-6 Available online: http://apps.who.int/gb/ebwha/pdf_files/EB134/B134_R7-en.pdf
- Lewington J, Namukwaya E, Limoges J, et al. Provision of palliative care for life-limiting disease in a low income country national hospital setting: how much is needed? BMJ Support Palliat Care 2012;2:140-4. [Crossref] [PubMed]
- Mpanga Sebuyira L, Mwangi-Powell F, Pereira J, et al. The Cape Town Palliative Care Declaration: home-grown solutions for sub-Saharan Africa. J Palliat Med 2003;6:341-3. [Crossref] [PubMed]
- Lazenby M, Sebego M, Swart NC, et al. Symptom Burden and Functional Dependencies Among Cancer Patients in Botswana Suggest a Need for Palliative Care Nursing. Cancer Nurs 2016;39:E29-38. [PubMed]
- Philips PL, Lazenby M. The emotional and spiritual well-being of hospice patients in Botswana and sources of distress for their caregivers. J Palliat Med 2013;16:1438-45. [Crossref] [PubMed]
- Downing J, Batuli M, Kivumbi G, et al. A palliative care link nurse programme in Mulago Hospital, Uganda: an evaluation using mixed methods. BMC Palliat Care 2016;15:40. [Crossref] [PubMed]


