The effect of early versus delayed radiation therapy on length of hospital stay in the palliative setting
Introduction
Radiation therapy (RT) is frequently utilized to improve local control and survival outcomes in cancer patients. However, it is estimated that half of all RT is delivered in the palliative setting in the United States (1,2). Radiotherapy offers non-invasive, cost-effective, safe and effective symptomatic improvement in patients with locally advanced or metastatic disease. Research has demonstrated palliative RT’s efficacy in multiple cancer sites, including thoracic and gastrointestinal tumors, and is particularly effective in symptomatic control for brain and bone metastases (3-6). Recent technologic advances have led to the ability to deliver higher ablative doses of radiation in fewer fractions with less radiation exposure to the neighboring anatomy, which may further expand radiation oncology’s role in palliative therapy.
Despite the well-established role of RT in the palliative setting, there are several obstacles in effective delivery. Providing palliative RT (PRT) often requires efficient coordination across multiple disciplines, particularly in the inpatient setting. Difficulties in this coordination of care may result in delayed referral for PRT, leading to undue discomfort and suffering. Despite the need for timely intervention, no study to date has investigated temporal relationships between time to consult, time to care, and resultant effect on hospital stay in the inpatient setting. We investigated patterns of care and outcomes in patients who received palliative RT in this setting.
Methods
This retrospective chart review was approved by the Banner Health Research institutional review board (IRB) (No. 017768). This was a retrospective analysis of patients at a single institution. Records were reviewed between August 2014 and October 2016. Inclusion criteria were patients in the inpatient setting that were referred to the radiation oncology department for palliative therapy, received treatment, and were discharged from the hospital. Patient therapy intent was determined to be palliative using the radiation oncologist’s discretion. Exclusion criteria were any patients that did not receive RT, had incomplete demographic or treatment records, or were referred to radiation oncology for definitive management. Collected information on patients included basic demographics and time between admission, consult, initiation of RT, and discharge were recorded. All patients were divided into two groups by time periods (greater than or less than 2 days). This time period was selected because patients with malignant spinal cord compressions have significantly worse prognosis if treatment is delayed beyond 48 hours (7,8). Comparison of mean days by group was statistically evaluated using independent two-sample t-tests. The threshold for statistical significance was P<0.05.
Results
Overall, 135 patients received PRT. However, patients who received PRT in the outpatient setting were excluded. After all inclusion/exclusion criteria, there were 60 patients with complete evaluable records. As per Table 1, the median age was 70 but had a broad range. Fractionation schemes ranged from 1–15 and with a median of 5. The median dose was 20 Gy. The most common primary disease sites were lung (32%) and breast (22%). The most frequently treated sites were bone (58%), brain (22%), and lung (17%). The most common indications for PRT were pain (37%), and neurological compromise (37%), or airway obstruction/dyspnea (18%). Of note, only two patients with neurological compromise were due to malignant spinal cord compression.
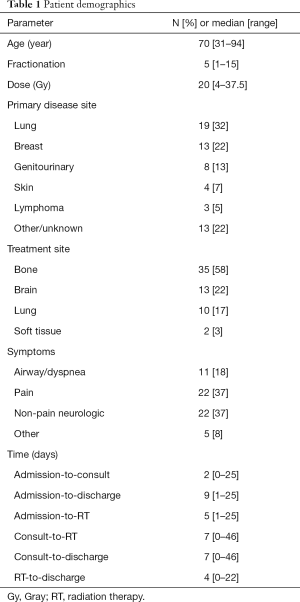
Full table
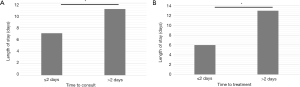
Analysis of temporal relationships demonstrated that patients who received radiation oncology consultation within 2 days (n=36) versus greater than 2 days (n=24) of admission had significantly decreased admission to discharge times (median 7 versus 11 days, respectively; P=0.02) (Figure 1A). Similarly, patients who received PRT within 2 days of admission (n=43) versus greater than 2 days of admission (n=17) had significantly shorter admission to discharge times (median 6 versus 13 days, respectively; P=0.03) (Figure 1B). Significance persisted across all reported time periods using 1, 3, and 4 days as thresholds for comparison.
Discussion
Evaluating temporal patterns of care in palliative therapy may reveal how delayed consultation and treatment might affect other important system parameters, such as length of stay. This study highlights the typical demographic of patients seen for palliative RT in the United States (1,3,9), with the majority of patients referred for palliation of brain or bone metastases. Our data demonstrate that time from admission to consult and from admission to PRT are significantly associated with total days spent in the hospital. Although not proving causation, our study suggests that further investigation into similar temporal relationships in the inpatient palliative setting are warranted.
These data support the hypothesis that early intervention may lead to reduced length of hospitalization. Interestingly, other significant temporal relationships between length of hospital stay, time from admission to consultation, time from admission to treatment, and time from consult to treatment were found as well (P<0.05 for all), demonstrating the multifactorial nature of this process. We chose to highlight the possibility that timely care in the palliative inpatient setting has meaningful impacts to the system and the patient and hope to generate further studies considering this important and systemically addressable item.
Although data are limited on this topic, Pintova and colleagues attempted to address a similar issue in a small retrospective study of 7 patients who received inpatient PRT (10). Their small cohort had an appreciably longer average length of stay of 40 versus 9 days in this study. Of note, 5 of the 7 patients opted to remain hospitalized for therapy, despite recommendation by the physical therapist to discharge home and seek outpatient treatment, which at least partially explains the substantially increased average length of stay. In light of this and other significant differences in patient selection criteria, direct comparisons cannot be accurately drawn.
Several interesting trends were identified during the analysis. First, duration of hospital stay was reduced in patients all patients referred to radiation oncology within 2 days, independently of whether or not these patients received PRT. Second, it was common for patients to be seen by radiation oncology and discharged shortly thereafter. One hypothesis for this observation is the fact that the consulting radiation oncologist may be able to propose options for palliative therapy previously not considered by the inpatient team, even if these palliative options did not include radiation. Additionally, the radiation oncology team may have recommended outpatient palliative care, allowing for more rapid discharge, whether or not the radiation was initiated in the inpatient setting.
Previously studies have highlighted numerous barriers to care in the use of RT in the palliative setting (11,12). Lutz and colleagues surveyed palliative facilities in the United States and found that, despite recognizing the importance of RT as an effective palliative measure, less than 3% of the hospice patients in the surveyed hospices received PRT during the year (11). In a similar study, researchers surveyed physician members of the American Society for Therapeutic Radiation Oncology (ASTRO), the American Academy of Hospice and Palliative Medicine (AAHPM) and the American Society of Clinical Oncology (ASCO) to assess the perceived role of PRT and barriers to effective use (13). The results highlighted that the majority agree that these professional societies should better promote effective multidisciplinary care and involvement of radiation oncology in palliative settings.
There are limitations to this study inherent to all retrospective analyses. First, we are unable to control for selection bias in our cohort, as alluded to above, though we attempted to counter this effect by utilizing a continuous series of patients from a particular time frame as noted above. Consideration of comorbidities has been correlated with outcomes in PRT (14) but was unavailable in our cohort. Second, patients may have been unstable on admission to the hospital and therefore the primary team did not feel a palliative consult was appropriate. However, we contend that this thinking may be flawed and early palliative considerations may be beneficial, even if not appropriate at that immediate time. This is supported by ASCO, which previously published their recommendation that, based on existing evidence, palliative care should be incorporated concurrently with standard oncology care to optimize patient quality of life, caregiver outcomes, improved symptomatic control, limitation of futile care, and much more (15). Lastly, our study was comprised of a small cohort, making subset analysis and more sophisticated statistical analysis difficult.
This retrospective analysis provides valuable, hypothesis-generating data highlighting a need in palliative treatment. It is clear that coordination of care and early involvement of the palliative team, including PRT, has numerous benefits including potentially decreased length of stay with benefits to the system and the patient. Prospective studies are needed to further delineate temporal relationships and outcomes in palliative radiation oncology.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective chart review was approved by the Banner Health Research institutional review board (IRB) (No. 017768).
References
- Janjan NA. An emerging respect for palliative care in radiation oncology. J Palliat Med 1998;1:83-8. [Crossref] [PubMed]
- Richter MP, Coia LR. Palliative radiation therapy. Semin Oncol 1985;12:375-83. [PubMed]
- Lutz ST, Jones J, Chow E. Role of Radiation Therapy in Palliative Care of the Patient With Cancer. J Clin Oncol 2014;32:2913-9. [Crossref] [PubMed]
- Wu JS, Wong R, Johnston M, et al. Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J Radiat Oncol Biol Phys 2003;55:594-605. [Crossref] [PubMed]
- Jones JA, Lutz ST, Chow E, et al. Palliative radiotherapy at the end of life: a critical review. CA Cancer J Clin 2014;64:296-310. [Crossref] [PubMed]
- Tey J, Back MF, Shakespeare TP, et al. The role of palliative radiation therapy in symptomatic locally advanced gastric cancer. Int J Radiat Oncol Biol Phys 2007;67:385-8. [Crossref] [PubMed]
- Chaichana KL, Woodworth GF, Sciubba DM, et al. Predictors of ambulatory function after decompressive surgery for metastatic epidural spinal cord compression. Neurosurgery 2008;62:683-92; discussion 683-92. [Crossref] [PubMed]
- Furstenberg CH, Wiedenhofer B, Gerner HJ, et al. The effect of early surgical treatment on recovery in patients with metastatic compression of the spinal cord. J Bone Joint Surg Br 2009;91:240-4. [Crossref] [PubMed]
- Chow E, Harris K, Fan G, et al. Palliative Radiotherapy Trials for Bone Metastases: A Systematic Review. J Clin Oncol 2007;25:1423-36. [Crossref] [PubMed]
- Pintova S, Holcombe RF, Blacksburg S, et al. Impact of inpatient radiation on length of stay and health care costs. J Community Support Oncol 2015;13:399-404. [Crossref] [PubMed]
- Lutz S, Spence C, Chow E, et al. Survey on Use of Palliative Radiotherapy in Hospice Care. J Clin Oncol 2004;22:3581-6. [Crossref] [PubMed]
- Lutz S, Korytko T, Nguyen J, et al. Palliative radiotherapy: when is it worth it and when is it not? Cancer J 2010;16:473-82. [Crossref] [PubMed]
- McCloskey SA, Tao ML, Rose CM, et al. National survey of perspectives of palliative radiation therapy: role, barriers, and needs. Cancer J 2007;13:130-7. [Crossref] [PubMed]
- Murphy JD, Nelson LM, Chang DT, et al. Patterns of Care in Palliative Radiotherapy: A Population-Based Study. J Oncol Pract 2013;9:e220-7. [Crossref] [PubMed]
- Smith TJ, Temin S, Alesi ER, et al. American Society of Clinical Oncology Provisional Clinical Opinion: The Integration of Palliative Care Into Standard Oncology Care. J Clin Oncol 2012;30:880-7. [Crossref] [PubMed]


