Patterns of symptom control and palliative care-focused original research articles in the International Journal of Radiation Oncology *Biology* Physics and the Radiotherapy and Oncology Journal, 2005–2014
Introduction
Symptom control and palliative care (SCPC) plays an important role in the field of radiation oncology, with approximately 30–40% of all radiation treatments delivered with palliative intent (1-3). In the advanced cancer setting, radiotherapy is commonly used to treat symptoms including pain, bleeding, ulceration, and obstruction (4). Furthermore, radiation is part of standard of care for many sites of metastatic disease including bone and brain metastases (5,6). Decisions regarding palliative treatment of these symptoms can often be complex, given that they necessitate careful cost/benefit decision-making in the context of an often-limited life expectancy. Furthermore, radiation is often used in many emergent complications of advanced cancer such as spinal cord compression, hemoptysis, and superior vena cava syndrome, which require rapid decision-making that has the potential to significantly impact quality of life.
Despite the degree to which SCPC is present in the clinical practice, palliative care (PC) in advanced cancer patients is poorly represented in radiation oncology research. Published studies by Barnes et al. found that only 1.3% of abstracts presented from 1993–2000 at The American Society for Therapeutic Radiation Oncology (ASTRO) meetings and 6.7% of abstracts presented from 1992–2002 at the Canadian Association of Radiation Oncologists (CARO) meetings pertained to SCPC topics (7,8). The paucity of SCPC research is especially concerning given that at least half of patients who die from advanced cancer have untreated or undertreated symptoms (9). It is therefore critical that radiation oncologists are not only adequately trained in providing effective SCPC, but also that radiation oncology as field engages in research to improve palliative treatments among this patient population.
In recent years, there has been a growing professional awareness towards PC, with a small but increasing number of academic radiation oncology departments incorporating dedicated PC services. Over the past 15 years, American Society of Clinical Oncology (ASCO) and ASTRO recommendations have called for oncologists to engage in research in advanced cancer populations to improve care and patient quality of life (10,11). However, it is unclear whether this has impacted the amount of SCPC research within the field. The International Journal of Radiation Oncology *Biology* Physics (Red Journal) and the Radiotherapy and Oncology Journal (Green Journal) are two of the largest and highest impact radiation oncology journals in the world [Red Journal impact factor =4.5 (12), Green Journal impact factor =4.8 (13)], and therefore provide a window into the field’s research focus and trajectory of research inquiry. The purpose of this study was to determine the number, content and quality of PC manuscripts in the advanced cancer setting published in the Red Journal and the Green Journal to determine both the prevalence of original PC research and to assess whether that line of research inquiry has changed over a 10-year period [2005–2014].
Methods
Full-length original research articles from 2005–2014 containing the words “palliative” and/or “metastasis” were identified in the Red Journal and Green Journal by a study member (DD Shi) using each journal’s online search function. Articles were included in the analysis if they were original research articles and excluded if they were abstracts published solely for presentation at meetings such as ASTRO or if they did not contain original research (e.g., editorials or reviews).
Resulting articles were categorized as PC if they pertained to any aspect of treatment of metastatic cancer, and classified as SCPC if they described patients with metastatic cancer for whom symptom palliation was the stated goal of treatment and/or PC needs was the goal of research inquiry, as defined by the Clinical Practice Guidelines for Quality Palliative Care (14). Studies related to treatment planning of palliative cases were categorized as SCPC, while studies examining outcomes of metastatic cancer patients treated with curative intent were not considered SCPC. Studies related to definitive treatment of oligometastatic disease were not considered SCPC.
SCPC abstracts were further categorized according to symptom palliated, disease site treated, nature of the study [randomized clinical trial (RCT) vs. other], if symptom palliation outcomes were reported, and if these outcomes represented the primary or secondary endpoint. Any article for which categorization was unclear was discussed with a second study member (S Skamene). If study members disagreed with categorization, a third study member (TA Balboni) was consulted, and a joint decision was reached.
Data were analyzed using descriptive statistics (including mean, range and percentages). A chi-square test was conducted to compare the proportions of SCPC abstracts, and a Cochran-Armitage trend test was used to identify publication trends over time. All statistical analyses were performed using R statistical software (version 0.99.902).
Results
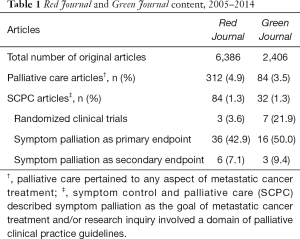
The results are summarized in Tables 1,2. Of the 6,386 articles published from 2005 to 2014 in the Red Journal, 312 (4.9%, range, 1.7–8.4% per year) pertained to PC, and 84 (1.3%, range, 0.2–2.4% per year) were categorized as SCPC. In the Green Journal, 84 (3.5%, range, 0.4–9.9% per year) out of 2,406 total articles pertained to PC, and 32 (1.3%, range, 0.0–3.2% per year) were categorized as SCPC. Randomized control trials accounted for the minority of SCPC articles in both journals, with 3.6% (3/84) in the Red Journal and 21.9% (7/32) in the Green Journal. The symptomatic treatment outcome was stated in 50.0% (42/84) of SCPC abstracts in the Red Journal and 59.4% (19/32) of the SCPC abstracts in the Green Journal. Furthermore, 42.9% (36/84) of the Red Journal SCPC articles and 50.0% (16/32) of the Green Journal SCPC articles described palliation of symptoms as a primary rather than a secondary study end point.
Full table
Full table
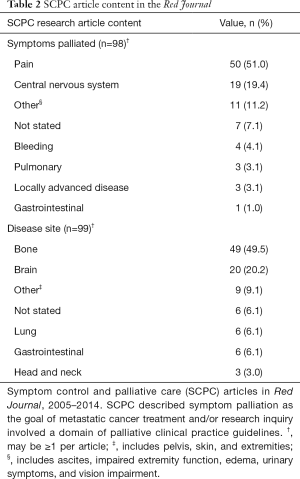
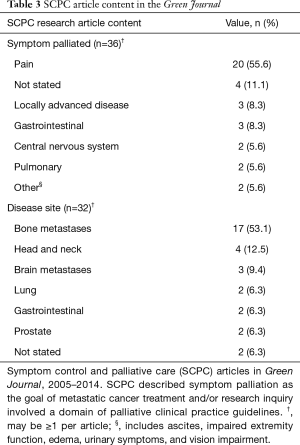
Among SCPC articles in the Red Journal, the most common symptom palliated was pain (51.0%), followed by central nervous system (CNS) (19.4%), and other (11.2%) (Table 2). The most common disease sites treated were bone metastases (49.5%), followed by brain metastases (20.2%), and other (9.1%). Among SCPC articles published in the Green Journal, the most common symptoms palliated were pain (55.6%), not stated (11.1%), and locally advanced disease (8.3%). The most common disease sites treated were bone metastases (53.1%), head and neck (12.5%), and brain metastases (9.4%) (Table 3).
Full table
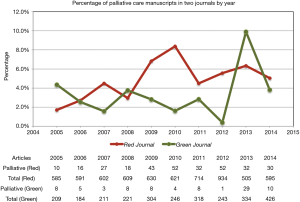
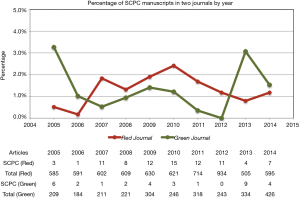
There was no change in annual proportion of articles pertaining to PC over time in the Red Journal (P=0.43). There was a trend towards increasing proportion of PC articles over time in the Green Journal that was not statistically significant (1.7% at study start to 5.0% at study end) (P=0.07) (Figure 1), and an significant increasing trend among both journals in aggregate (P=0.04). There was no significant trend over time in the proportion of SCPC articles in the Red Journal (P=0.76), the Green Journal (P=0.48), or in both journals in aggregate (P=0.38) (Figure 2).
Discussion
Research focused on SCPC in radiation oncology accounted for 1.3% of published manuscripts between 2005–2014 in both the Red Journal and Green Journal. Only 3.5% of articles from the Red Journal and 21.9% from the Green Journal represented randomized controlled trials in SCPC. In addition to the low representation of SCPC articles in these journals, there were mixed patterns of publication trends over the study period. While the Red Journal did not demonstrate a trend in proportions of either palliative or SCPC articles over time, there was a trend towards increasing annual proportion of palliative articles in Green Journal, with no trend in annual proportion of SCPC articles over time. Overall in both journals in aggregate, there was a significant increasing trend in annual proportion of palliative articles, but no trend in annual proportion of SCPC articles over time.
Our data is overall consistent with published prevalence of PC research in radiation oncology, with 1.3% of abstracts at ASTRO and 6.7% of abstracts presented at CARO pertaining to SCPC. Even in examining trends among oncology in general, PC topics are underrepresented in research, with 6.3% of abstracts at ASCO pertaining to SCPC (15). While the proportion of SCPC abstracts presented at annual assemblies has been shown to have increased over time for CARO, there was no change in the proportion of SCPC abstracts at ASTRO, and a significant decrease in SCPC abstracts presented at the ASCO annual assemblies (7,8,15). Our results indicate that the presence of SCPC focused research in radiation oncology remains stagnant overall. Notably, the Green Journal, which publishes heavily from Canada and Europe, published lower rates of SCPC research compared to the proportion of SCPC abstracts presented at CARO (1.3% vs. 6.7%), while the Red Journal, which publishes relatively more research from the United States, mirrors the lower proportion of SCPC abstracts presented at the American conference, ASTRO (1.3% in both).
The poor representation of PC and SCPC publications in these two journals stands in contrast to the approximately 30–40% of radiation therapy that is palliative in intent. Both ASCO and ASTRO have published recommendations for more involvement of oncologists and radiation oncologists with end-of-life care in advanced cancer patients (11,16). Despite these recommendations, the amount of resources dedicated to SCPC research and educations remains disproportionately low compared to its representation in clinical practice. The reasons for this are likely multifactorial. First, the discrepancy between research publications and clinical practice and guidelines in PC within radiation oncology is likely reflective of the paucity of radiation oncologists dedicating their academic careers to PC and/or research among advanced cancer populations. There has been some growth in academic emphasis in PC among radiation oncologists in recent years, for example as evidenced by the development or organizations such as the Society for Palliative Radiation Oncology (17).
Second, the current structure of radiation oncology residency training in the United States has variable emphasis on PC within radiation oncology. A survey of 404 U.S. radiation oncology residents indicated that 79% perceive inadequacies in their training across palliative radiation oncology competencies, and 81% desire further palliative oncology education (18). Furthermore, only select academic centers have dedicated palliative radiation oncology services, further limiting training within palliative radiation oncology to residents (19,20). Without adequate exposure to palliative clinical management during residency, trainees are less likely to be exposed to relevant clinical questions, and less likely to become engaged in PC research among this patient population.
A third challenge to research in SCPC within radiation oncology regards the general challenges of conducting rigorous clinical research among advanced cancer patients. Research in this field can be plagued by difficulties in accrual due to poor performance status and loss to follow-up due to clinical decline and death. Furthermore, primary endpoints for palliative treatments can be difficult to define, often relying on patient-reported outcome measures that have variable degrees of validation (21). Research is also limited by funding, with only a small portion of the national research budget dedicated to PC research. However, this is not to say that large trials among advanced cancer patient populations is infeasible, given that informative randomized controlled trials have been conducted in this patient population, including in bone and brain metastases (22-25).
Our study is not without limitations. The articles were initially identified by searching for the words “palliative” and/or “metastasis” in all content within each journal’s advanced search function, and SCPC or PC articles may have not been captured if they did not contain these search terms. In addition, there may have been potential bias in categorization, though reasons and justifications for categorization were kept consistent throughout. Furthermore, any conflicts in categorization were thus corroborated with two radiation oncologists (S Skamene, TA Balboni) in order to minimize this bias.
Conclusions
The International Journal of Radiation Oncology *Biology* Physics (Red Journal) and Radiotherapy and Oncology Journal (Green Journal) are two of the leading radiation oncology journals and reflect current trends in clinical research. Despite national recommendations for greater integration of PC in oncology, our findings suggest that only a small proportion of articles published in these journals pertained to SCPC topics. Research in SCPC should be further encouraged by academic departments, research funding sources, and residency training programs, as well as national organizations such as ASCO, ASTRO, and CARO. Further SCPC research is necessary to advance care and outcomes for incurable cancer patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Coia LR, Hanks GE, Martz K, et al. Practice patterns of palliative care for the United States 1984-1985. Int J Radiat Oncol Biol Phys 1988;14:1261-9. [Crossref] [PubMed]
- van Oorschot B, Rades D, Schulze W, et al. Palliative radiotherapy--new approaches. Semin Oncol 2011;38:443-9. [Crossref] [PubMed]
- Tseng YD, Krishnan MS, Jones JA, et al. Supportive and palliative radiation oncology service: impact of a dedicated service on palliative cancer care. Pract Radiat Oncol 2014;4:247-53. [Crossref] [PubMed]
- Lutz ST, Jones J, Chow E. Role of Radiation Therapy in Palliative Care of the Patient With Cancer. J Clin Oncol 2014;32:2913-9. [Crossref] [PubMed]
- Lutz S, Balboni T, Jones J, et al. Palliative radiation therapy for bone metastases: Update of an ASTRO Evidence-Based Guideline. Pract Radiat Oncol 2017;7:4-12. [Crossref] [PubMed]
- Tsao MN, Rades D, Wirth A, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol 2012;2:210-25. [Crossref] [PubMed]
- Barnes EA, DeBoer G, Chow E. Symptom control and palliative care content of abstracts presented at the Canadian Association of Radiation Oncologists annual meetings. Support Care Cancer 2004;12:91-4. [Crossref] [PubMed]
- Barnes EA, Palmer JL, Bruera E. Prevalence of symptom control and palliative care abstracts presented at the Annual Meeting of the American Society for Therapeutic Radiology and Oncology. Int J Radiat Oncol Biol Phys 2002;54:211-4. [Crossref] [PubMed]
- Komurcu S, Nelson KA, Walsh D, et al. Common symptoms in advanced cancer. Semin Oncol 2000;27:24-33. [PubMed]
- Smith TJ, Temin S, Alesi ER, et al. American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 2012;30:880-7. [Crossref] [PubMed]
- SCOPE Steering Committee and Subcommittees. Report of the American Society for Therapeutic Radiology and Oncology Working Group on the scope of radiation oncology (SCOPE). Int J Radiat Oncol Biol Phys 2002;54:317-26. [PubMed]
- International Journal of Radiation Oncology*Biology*Physics Impact Factor. Available online: http://journalinsights.elsevier.com/journals/0360-3016/impact_factor
- Radiotherapy and Oncology impact factor. Available online: http://www.journals.elsevier.com/radiotherapy-and-oncology/
- Clinical Practice Guidelines for Quality Palliative Care. Available online: http://www.nationalcoalitionhpc.org/ncp-guidelines-2013/
- Sweeney C, Beattie-Palmer L, Palmer JL, et al. Changing Patterns of Symptom Control and Palliative Care Paper Presentations at the Annual Meeting of the American Society of Clinical Oncology. J Clin Oncol 2001;19:3438-9. [Crossref] [PubMed]
- Cancer care during the last phase of life. J Clin Oncol 1998;16:1986-96. [Crossref] [PubMed]
- Society for Palliative Radiation Oncology (cited 2017 Mar 8). Available online: http://www.spro.org
- Krishnan M, Racsa M, Jones J, et al. National Radiation Oncology Survey on Palliative Care Education in Radiation Oncology Training. Pract Radiat Oncol 2017;7:e439-48. [Crossref] [PubMed]
- Stavas MJ, Pagan JD, Varma S, et al. Building a palliative radiation oncology program: From bedside to B.E.D. Pract Radiat Oncol 2017;7:203-8. [Crossref] [PubMed]
- Gorman D, Balboni T, Taylor A, et al. The Supportive and Palliative Radiation Oncology Service: A Dedicated Model for Palliative Radiation Oncology Care. J Adv Pract Oncol 2015;6:135-40. [PubMed]
- Bruner DW. Should Patient-Reported Outcomes Be Mandatory for Toxicity Reporting in Cancer Clinical Trials? J Clin Oncol 2007;25:5345-7. [Crossref] [PubMed]
- Murray KJ, Scott C, Zachariah B, et al. Importance of the mini-mental status examination in the treatment of patients with brain metastases: a report from the Radiation Therapy Oncology Group protocol 91-04. Int J Radiat Oncol Biol Phys 2000;48:59-64. [Crossref] [PubMed]
- Hartsell WF, Scott CB, Bruner DW, et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst 2005;97:798-804. [Crossref] [PubMed]
- Gondi V, Pugh SL, Tome WA, et al. Preservation of Memory With Conformal Avoidance of the Hippocampal Neural Stem-Cell Compartment During Whole-Brain Radiotherapy for Brain Metastases (RTOG 0933): A Phase II Multi-Institutional Trial. J Clin Oncol 2014;32:3810-6. [Crossref] [PubMed]
- Mulvenna P, Nankivell M, Barton R, et al. Dexamethasone and supportive care with or without whole brain radiotherapy in treating patients with non-small cell lung cancer with brain metastases unsuitable for resection or stereotactic radiotherapy (QUARTZ): results from a phase 3, non-inferiority, randomised trial. Lancet 2016;388:2004-14. [Crossref] [PubMed]


