Advance care planning for patients with advanced neurology diseases
Introduction
Advanced neurology diseases including motor neuron disease (MND) are usually progressive life-limiting illness and could be devastating for patients, families and caregivers (1-3). Although medical technologies, such as enteral feeding and non-invasive ventilation, may prolong life expectancies of patients, their utilization prompts important ethical questions in regards to patients’ quality of life (QoL) (4).
End-of-life (EOL) decision-making in the context of advanced neurology disease may be complex and challenging for patients, families and health professionals as patients suffering from the disease involve variety in age groups. In this context, advance care planning (ACP), that could encourage the discussion of patient’s preference in some form of advance directive (AD) before physical or cognitive decline, could help facilitating patient in the acceptance of the disease with documentation. APC would ideally occur prior to initiating life-sustaining treatments, such as nutritional support or non-invasive ventilation, and the circumstances under which patients would want these withdrawn should be considered (4). Circumstances under which patients who were undergoing the nutritional or ventilator support would want these withdrawn anytime should be carefully considered as well. ADs are designed to enable patients to participate in critical life-sustaining decisions (e.g., refusal of life-sustaining treatment), in consideration to patient autonomy and dignity towards EOL (5).
In clinical practice, caregivers and other relatives would be asked to make EOL or critical medical decisions if patients had not undersigned AD. Such decision-making was proven to elicit distress in family members (6) and in addition did not always lead to decisions consistent with patients’ wishes (7).
Various efforts have been made in the last three decades in supporting a certain amount of patients to make informed decisions at the EOL, the most notable being the ACP (7). During the ACP process, patients are encouraged to complete AD documenting specific medical treatment preferences (e.g., a living will) and to designate a healthcare proxy (i.e., durable power of attorney for health care or healthcare proxy) in the event that they are unable to make decisions for themselves (8). The use of ADs in the Hong Kong has been steadily increasing, with completion rates as high as 70% reported in some studies (9).
Nowadays, healthcare professionals generally agree that facilitation of ACP discussions between the patient and proxy and provision of information reflecting the evolving course of the neurology disease should occur regularly during admissions or patient clinic visits (10). Both AD with refusal of cardiopulmonary resuscitation and do not attempt cardiopulmonary resuscitation (DNACPR) order could be updated in the electronic health care system. This could facilitate a comprehensive care process and reduce unnecessary invasive interventions when patients were admitted under acute medical conditions.
According to the literature, few extant studies of EOL care in patients with advanced neurology diseases have focused on general experiences of EOL caregiving (11). We are unaware of any published studies on ACP practice among patients with different neurology diseases. In our study, we assessed EOL care preferences, documentation, and communication in patients with various types of advanced neurology diseases.
Methods
By using retrospective chart review, advanced neurology patients who referred to the neuro-palliative care team (NPCT) in a local acute hospital in Hong Kong. The diagnoses of advanced neurology disease were confirmed by attending neurologists. During the visit, each patient was evaluated by a collaborative NPCT consisted of a neurologist, a palliative physician, a palliative nurse and a social worker.
NPCT has regular joint activities including ward round and palliative clinic outpatients involving both neurology and palliative care (PC) teams. The joint round is held in both neurology and also PC wards. The purpose of joint ward round is to screen PC needs, provide on-site symptom advice, psychosocial support and end of life for advanced neurology patients. The parent team will introduce PC team to patients, explain the disease prognosis and consider any other alternatives for medical treatments.
During these consultative visits, any discussion on EOL care, preferences on ventilation and others like DNACPR would be noted in the patient’s chart. Other documentation included duration of the disease, lung function test and bulbar function. Those on invasive mechanical ventilation will be excluded. All statistical analyses were performed by SPSS 22.
Those adult patients (>18 years old) referred to the NPCT from the period of January 2016 to March 2017 were included in this study. The demographical and clinical data were received from hospital electronic record (HER). The neurology diseases included bad stroke, end-stage myopathy, MND, advanced multiple sclerosis and end-stage Parkinsonism. Other neurology diagnosis including intracranial hemorrhage or brain metastasis will be excluded.
NPCT consultation was hand abstracted from the HER if there was a subspecialty PC consultation note during the study period. Hand abstraction of data also included any content related to ACP (AD, DNACPR, ventilator support, artificial feeding, patient wishes, legacy) which are the NPCT standard discussion.
Statistical analysis
The overall data was summarized, and divided into two subgroups based on the category of AD (i.e., AD and non-AD). t-test was used to examine the relationship between AD and continuous variables while the Fisher exact test or chi-squared test for categorical variables. P value of less than 0.05 was regarded as statistically significant.
Results
The sample populations
Between January 2016 and March 2017, a total of 28 patients were referred based on the inclusion criteria. The range of participants’ age was 23–91 years, including 15 males and 13 females; all Hong Kong Chinese patients; 15 (56%) were married. EOL issues were discussed at the first consultative visit in 26 participants (93%). Six (24%) out of 25 patients were mentally incompetent.
One patient was excluded as he was on ventilator in the first consultation. Ten participants (75%) made the decision for AD in case of their condition deteriorated in PC consultative visits. No patient asked for use of mechanical ventilation.
From 10 participants with AD, 7 (70%) had MND diagnosis. The range of time between diagnosis and first consultative visit was 1–94 months (mean, 6.8 months). However, 80% of patients decided AD at the initial visit of NPCT.
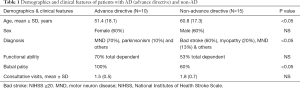
The mean (SD) age of AD participants was 51.4 (18.1) years old and 60% of them were female (Table 1). AD Patients were younger, more likely to have MND diagnosis and bulbar palsy than non-AD patients (P<0.05). The mean number of PC consultations (1.5 vs. 1.8, P<0.05) are similar in both groups. The types and contents of the ACP are summarized in Table 2.
Full table
Full table
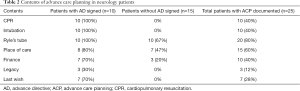
For patient who signed AD, cardiopulmonary resuscitation (100%), mechanical ventilation (100%), artificial nutrition and hydration (80%) was mentioned more frequently than other EOL interventions. For patients who had ACP but without AD, the most common diagnosis is bad stroke (60%). Place of death, artificial nutrition and hydration were most mentioned EOL interventions in this group of patients.
Discussion
It is often crucial for healthcare workers to draw attention to the decision of EOL for advanced neurology patient. Our result is encouraging as it showed most MND patients could sign their AD in the initial PC consultative visits. Previous study showed patients with MND would like the chance to get involved for EOL discussion with their doctors in-charge (2). Our finding was coherent to this. A significant portion of our patients also took part in discussion of EOL issues at the first clinic visit by NPCT.
One study showed that although majority (>80%) of patients believed that their doctors in-charge would like to understand their preferences for EOL management, only small number of patients (<10%) had actually made the discussion with them (2). Therefore, there remains a marked discrepancy between patient expectation and actual discussion for EOL management in MND patients.
Although there are extensive studies for EOL issues in patients with advanced oncology diseases or some advanced medical illness (11), there is only patchy information regarding the counterparts for advanced neurology patient. As a result, consensus is difficult to be made if EOL issues are to be discussed with such group of patients. Given the gradual deterioration of MND, it usually allows enough time to prepare patients and their families for EOL discussions (12). Another study showed that approaches for EOL in patients with MND might vary due to several demographical factors (12). However, little has been mentioned in the literature when EOL issues should be addressed.
Despite there are usually several months after the diagnosis of MND till the DNACPR order (12), our study showed that most patients would decide for EOL issues at their first visit. It may be postulated that most MND patients have considered their EOL wishes well before the topic is raised by their healthcare providers. We advocate that decisions regarding resuscitation should be explored early in the disease course, especially at the point of initial diagnosis. This is supported by the fact that not only patients are willing to consider EOL care early; it should also be discussed in a timely manner before debilitation. It is well understood that no premature EOL discussion should be initiated before the diagnosis of MND is supported by a neurologist. However, as patient may deteriorate rapidly and unpredictably after each visit, they may become too moribund for any meaningful communication in the future, exploration of EOL plan and introduction of PC early in the disease course would be advisable. For example, during the natural course of MND, there might be unfavorable scenarios having MND patients with respiratory distress undergoing emergency intubation against his or her wishes because there was no EOL decision in place.
Our initiative for early discussion of EOL care echoed the views by other investigators (4). As patient’s preferences may differ over the course of the disease (11), we suggest open discussion and continuous education with patients during subsequent follow up visits.
In fact, PC, neurology and respiratory physicians have pivotal role in patients suffered from MND. As commonly observed, the terminal event in these patients involves a progressive respiratory distress, as reflected by a deteriorating lung function test. However, it is very often difficult to discuss such sensitive issue when the patient’s condition becomes unfit. And respiratory physician might not be in their good position to discuss in-depth with the advanced neurology patients without the support from the PC team.
Bearing this in mind, this retrospective analysis seems to stress the key role of the clinicians for patients with MND. Although any health care professional can help patients with MND for early discussion of EOL, since PC physicians are more experienced in managing terminal illness, the PC physicians are perhaps the most competent personnel to address EOL issues with these patients. However, currently many neuromuscular centers may not be equipped with a PC physician/nurse to see MND or other advanced neurology disease patients. As a result, our collaborative NPCT set up a good example to provide ACP for those advanced neurology patients in an acute hospital.
From previous studies, factors that seemed to have minimal influence in EOL decision making include time to definitive diagnosis and the severity of the restrictive lung condition. One study found that MND patients’ functional status would not affect their EOL decision (13). One of the drawbacks of our study is the fact that it consisted of retrospective analysis and the disease groups are quite heterogeneous. Apart from that, as only one center was involved in carrying out all the EOL discussion, it is understandable that the limited number of physicians involved may influence patients’ perception and decision. One study by Moss and colleagues found, in 1993, that physician bias can affect EOL decision making in MND patients (14). As a result, efforts were taken to minimize the effect of personal bias.
Many ADs addressed life-prolonging or EOL treatments such as invasive mechanical ventilation and artificial nutrition. These results are similar to those of other studies involving patients with heart failure (15), left ventricular assist devices (16), implantable cardiac defibrillators (17), pacemakers (18), and renal palliative patients (19). Today, many AD forms prompt patients to document their EOL preferences pertaining to specific life-prolonging measures.
Our NPCT would also address on legacy and last wish for ACP. This is important as most of our patients are expected to be young and has active roles, thus accompanied with many unfinished business (20). Our approach would help to address the psycho-spiritual stress suffered.
On the other hand, those non-AD patients especially bad stroke patients referred to NPCT were unable to discuss their AD in our study. This group of patients might require closer follow up for their EOL decision by providing necessary information, explanation and some might even require emotional and practical support when facing challenges. It is suggested that PC team could provide home visit in order to help them to complete their ACP.
Conclusions
EOL decision making in patients with advanced neurology disease is often delayed. This study showed that MND patients were likely to be ready to discuss their EOL issues and signed their AD. The NPCT can play an important role in EOL discussions in patients with advanced neurology diseases under collaboration between the PC and the neurology teams.
Acknowledgements
The authors would like to thank all medical and nursing staff of both Grantham Hospital and Queen Mary Hospital for their advice and support in taking care of neurology palliative care patients in our study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional review boards at the University of Hong Kong and Hospital Authority Hong Kong West Cluster (HKWC) (No: UW 16-187).
References
- Mitchell JD, Borasio GD. Amyotrophic lateral sclerosis. Lancet 2007;369:2031-41. [Crossref] [PubMed]
- Kiernan MC, Vucic S, Cheah BC, et al. Amyotrophic lateral sclerosis. Lancet 2011;377:942-55. [Crossref] [PubMed]
- Turner MR, Hardiman O, Benatar M, et al. Controversies and priorities in amyotrophic lateral sclerosis. Lancet Neurol 2013;12:310-22. [Crossref] [PubMed]
- Bradley MD, Orrell RW, Clarke J, et al. Outcome of ventilatory support for acute respiratory failure in motor neurone disease. J Neurol Neurosurg Psychiatry 2002;72:752-6. [Crossref] [PubMed]
- Salmond SW, David E. Attitudes toward advance directives and advance directive completion rates. Orthop Nurs 2005;24:117-27. [Crossref] [PubMed]
- Nolan MT, Hughes MT, Kub J, et al. Development and validation of the Family Decision-Making Self-Efficacy Scale. Palliat Support Care 2009;7:315-21. [Crossref] [PubMed]
- Sharma RK, Hughes MT, Nolan MT, et al. Family understanding of seriously-ill patient preferences for family involvement in healthcare decision making. J Gen Intern Med 2011;26:881-6. [Crossref] [PubMed]
- Walczak A, Butow PN, Davidson PM, et al. Patient perspectives regarding communication about prognosis and end-of-life issues: how can it be optimised? Patient Educ Couns 2013;90:307-14. [Crossref] [PubMed]
- Chung RY, Wong EL, Kiang N, et al. Knowledge, Attitudes, and Preferences of Advance Decisions, End-of-Life Care, and Place of Care and Death in Hong Kong. A Population-Based Telephone Survey of 1067 Adults. J Am Med Dir Assoc 2017;18:367.e19-367.e27. [Crossref] [PubMed]
- Vianello A, Arcaro G, Palmieri A, et al. Survival and quality of life after tracheostomy for acute respiratory failure in patients with amyotrophic lateral sclerosis. J Crit Care 2011;26:329.e7-14. [Crossref] [PubMed]
- Lightowler JV, Wedzicha JA, Elliott MW, et al. Non-invasive positive pressure ventilation to treat respiratory failure resulting from exacerbations of chronic obstructive pulmonary disease: Cochrane systematic review and meta-analysis. BMJ 2003;326:185. [Crossref] [PubMed]
- Moss AH, Oppenheimer EA, Casey P, et al. Patients with amyotrophic lateral sclerosis receiving long-term mechanical ventilation. Advance care planning and outcomes. Chest 1996;110:249-55. [Crossref] [PubMed]
- Silverstein MD, Stocking CB, Antel JP, et al. Amyotrophic lateral sclerosis and life-sustaining therapy: patients' desires for information, participation in decision making, and life-sustaining therapy. Mayo Clin Proc 1991;66:906-13. [Crossref] [PubMed]
- Moss AH, Casey P, Stocking CB, et al. Home ventilation for amyotrophic lateral sclerosis patients: outcomes, costs, and patient, family, and physician attitudes. Neurology 1993;43:438-43. [Crossref] [PubMed]
- Swetz KM, Mueller PS, Ottenberg AL, et al. The use of advance directives among patients with left ventricular assist devices. Hosp Pract (1995) 2011;39:78-84. [Crossref] [PubMed]
- Tajouri TH, Ottenberg AL, Hayes DL, et al. The use of advance directives among patients with implantable cardioverter defibrillators. Pacing Clin Electrophysiol 2012;35:567-73. [Crossref] [PubMed]
- Pasalic D, Tajouri TH, Ottenberg AL, et al. The prevalence and contents of advance directives in patients with pacemakers. Pacing Clin Electrophysiol 2014;37:473-80. [Crossref] [PubMed]
- Singer PA, Thiel EC, Naylor CD, et al. Life-sustaining treatment preferences of hemodialysis patients: implications for advance directives. J Am Soc Nephrol 1995;6:1410-7. [PubMed]
- Chan KY, Yip T, Yap DY, et al. Enhanced Psychosocial Support for Caregiver Burden for Patients With Chronic Kidney Failure Choosing Not to Be Treated by Dialysis or Transplantation: A Pilot Randomized Controlled Trial. Am J Kidney Dis 2016;67:585-92. [Crossref] [PubMed]
- Chan KY, Chan ML, Yau TC, et al. Quality of life for Hong Kong Chinese patients with advanced gynecological cancers in the palliative phase of care: a cross-sectional study. J Palliat Care 2012;28:259-66. [PubMed]


