Persistent pain after breast cancer treatment
Introduction
Breast cancer is the commonest cancer affecting women with a 5-year survival over 80% as a result of earlier diagnosis and improved management. With improved survival rates, increasing attention is focused on the quality of life of these breast cancer survivors.
The major factors that affect survivors’ quality of life are some cancer treatment-related side effects that occur in up to 90% of patients during treatment and can persist for months or years after treatment has ended (1). Chemotherapy, radiation therapy and hormonal therapy can all contribute to the development and persistence of side effects, including: upper extremity restricted lymphedema, cognitive impairment (2-9), fatigue (10-12), sleep difficulty (13), pain (14-16), chemotherapy-induced peripheral neuropathy, cardiotoxicity (17,18), and bone loss (19,20). All these side effects accompanied with breast cancer treatments negatively influence quality of life and daily activities, lead to non-compliance treatments, and ultimately affect prognostic and survival outcomes (21,22). Interventions to alleviate side effects are needed to reduce symptom burden, enhance quality of life and functional capacity, and improve adherence to therapy (1).
One potential debilitating problem that breast cancer survivors may suffer with is persistent pain after breast cancer treatment (PPBCT) that is a common side effect with prevalence as high as 50% (23,24). The International Association for the Study of Pain (IASP) has established that pain can be considered chronic when it has persisted beyond the normal time of healing, with 3 months being considered ‘the most convenient point of division between acute and chronic pain’ (25). It was further proposed in the IASP taxonomy that when pain is associated with cancer, ‘3 months can be too long to wait before considering the pain as chronic’ (25).
A multivariate analysis of the presence of chronic pain in breast cancer survivors revealed that only younger age was associated with a significantly increased risk of developing chronic pain at 3 months after surgery (26). Furthermore, more invasive surgery, radiation therapy after surgery, and clinically meaningful acute postoperative pain but not Preoperative emotional status each independently predicted more intense chronic pain at 3 months after surgery (26).
The etiology of PPBCT is probably multifactorial (27). According to a recent systematic review of the prevalence and etiology of neuropathic pain in 13,683 cancer patients identified in 22 eligible studies, either sensory abnormality or diagnostic lesion was confirmed to contribute to the PPBCT in 14 studies (28). Although breast cancer treatment includes different types of surgical interventions (e.g., mastectomy, lumpectomy, sentinel lymph node biopsy, and axillary lymph node dissection), and adjuvant therapies like chemotherapy, radiation and endocrine therapies, only pre-existing nerve damage and radiotherapy appear to be significant risk factors (27). The detailed etiology of PPBCT needs further research efforts.
The mechanisms involved in PPBCT are uncertain and may involve peripheral as well as spinal and supraspinal structures. Event-related potentials (ERPs) of PPBCT patients, cancer treatment without persistent pain patients and healthy volunteers show different characteristics (29). PPBCT is associated with stimulus processing that is both delayed [i.e., increased latency of the ERP positivity between 250-310 ms (P260)], and enhanced (i.e., enhanced P260 amplitude) when compared with breast cancer treatment without persistent pain patients. However, breast cancer treatment without persistent pain is associated with accelerated stimulus processing (reduced P260 latency) and shows a tendency to be less intense (lower P260 amplitude) that the healthy volunteers. These results suggest that treatment and persistent pain have opposite effects on cortical responsiveness (29).
Global PPBCT epidemiology
The global epidemiology of PPBCT is still incomplete probably because of the neglected recognition of PPBCT. It is conceivable that the incidence of PPBCT may be underestimated, since there may be multiple barriers for patients to report their pain to their physicians. Ongoing pain after treatment is an unexpected reality for some women with breast cancer and may induce anxiety about cancer recurrence (30), and some women may not report persistent pain for fearing that they may find out to be cancer recurrence. Barriers to asking questions about pain also include fearing the answer that it is inevitable, and that concerns about pain will be ignored (31). Additionally, multiple other barriers may exists including: fear of bothering their busy physician, fear that their physicians may think less of them (or be annoyed at them), fear that if they complain about their pain - this might distract their physician and take valuable time away during their short interaction that they would rather have focused on discussions about cancer/prognosis.
Peretti-Watel et al. conducted in-depth interviews with French breast cancer survivors 24 months after cancer diagnosis and treatment (32). Fifty percent of participants reported suffering from significant chronic pain. Most of the time, this pain was not captured by the World Health Organization Quality of Life (WHOQOL) questionnaire and was not medically treated. Patients “normalized” their pain in various ways: they considered it either as a necessary step on the road to recovery, as the proof of treatment efficacy, or as a permanent condition one must learn to live with (32). Although there are fragmentary reports on the epidemiology of PPBCT, more efforts should be put on this issue in the future.
Persistent pain after breast cancer surgery (PPBCS)
Almost all of the 226,870 women diagnosed with breast cancer in 2012 will undergo surgery (33), which raises the focus on the most commonly studied complications, the persistent pain following breast cancer surgery (PPBCS) (26,34). PPBCS is different from other painful syndromes because it is typically localized to the anterior or lateral region of thorax, axillary and/or medial upper arm, causing burning pain, shooting pain, pressure sensation or numbness (35-37). The incidence of pain syndrome 6 months post-breast cancer surgical treatment was 52.9%. In relation to sensitive alteration, 52.6% patients have shown intercostobrachial pain, 1.3% neuroma and 3.2% have related phantom breast pain. Pain on the shoulder and/or thoracic-scapular area as a consequence of breast cancer surgical treatment was observed in 27.2% patients [relative risk (RR) ¼ 5.23 95% confidence interval (CI): 1.11e24.64] and (RR ¼ 2.01 95% CI: 1.08-3.75). Younger women (<40 years) and those who were submitted to axillary lymphadenectomy (with more than 15 removed lymph nodes) have shown risk of developing pain syndrome after breast cancer surgical treatment (38).
In general, incidences of PPBCS have been estimated as: about 10% for inguinal herniotomy (39), 25% to 50% for thoracotomy (40), and about 25% to 60% after breast cancer treatment (41). The severity of PPBCS may vary significantly depending on the surgical procedure performed (41). Gärtner and colleagues conducted a nationwide cross-sectional questionnaire study of 3,754 women aged 18 to 70 years who received surgery and adjuvant therapy (if indicated) for primary breast cancer in Denmark between January 1, 2005, and December 31, 2006 (41). A total of 1543 patients (47%) reported pain in 1 or more areas, of which 201 (13%) reported severe pain (scores of 8-10 on the numeric rating scale of 0-10 scores), 595 (39%) reported moderate pain (scores of 4-7), and 733 (48%) reported light pain (scores of 1-3) (41). Among women reporting severe pain, 77% experienced pain every day, whereas only 36% of women experiencing light pain had pain every day. A total of 278 patients (18%) reported pain in only 1 area, 435 (28%) in 2 areas, 429 (28%) in 3 areas, and 400 (26%) in all 4 areas. The most frequently reported area of pain was the breast area (n=1,331; 86%), followed by axilla (n=975; 63%), arm (n=872; 57%), and side of the body (n=857; 56%) (41). Mastectomy had no significant association on OR for reporting pain compared with BCS, but those women reporting pain after mastectomy had a higher risk of moderate to severe pain compared with light pain OR, 1.37; 95% CI: 1.00-1.87; P=0.048) (41). ALND was associated with an increased risk of pain (OR, 1.77; 95% CI: 1.43-2.19; P=0.001) compared with SLND, and also a risk factor for moderate to severe pain (OR, 1.39; 95% CI: 1.03-1.88; P=0.03) (41).
A substantial number of women who undergo axillary lymph node surgery continue to experience pain or physical discomfort during the year after treatment (42). Andersen et al. examined PPBCT, sensory disturbances and functional impairment in patients treated with a 2-step axillary lymph node dissection compared to patients with an sentinel lymph node biopsy (SLNB) followed by an immediate axillary lymph node dissection (ALND), and patients with ALND without a prior SLNB (43). Overall prevalence of PPBCT and sensory disturbances was high, with about 55% reporting PPBCT and 77% reporting sensory disturbances in all groups. No differences were found between the groups on prevalence and intensity of PPBCT (P=0.92), sensory disturbances (P=0.32), and functional consequences (P=0.35) (43).
Foley and colleagues (44) described a distinct syndrome of pain and sensory abnormalities following mastectomy that they termed post-mastectomy pain syndrome (PMPS). In PMPS, pain is typically localized to the axilla, medial upper arm, and/or the anterior chest wall on the affected side (34). Damage to the intercostobrachial nerve, which can occur with axillary node dissection, has been considered the most common cause of PMPS. For example, in a series of 38 patients who had undergone mastectomy with axillary node dissection, a lesion of the intercostobrachial nerve was considered the cause of pain in seven of eight patients with persistent pain revealed during neurologic examination (35,45).
A study specifically evaluating pain after breast reconstruction was conducted in 1996 (46). Women whose reconstruction involving breast implants had a greater prevalence of pain (53%) than patients who had reconstruction without implants (30%), and those women who had reconstruction without implants had a very similar prevalence of pain as patients who had mastectomy without reconstruction. There is some evidence that the incidence of chronic pain following breast cancer surgery, its intensity (47), and associated sensory abnormalities decrease over time. Ivens et al. [1992] found that the likelihood of chronic pain diminished from 31% at 1-2 years to 20% after more than 4 years following breast cancer surgery (48).
Bokhari et al. conducted a prospective, quantitative, longitudinal pilot survey before surgery and at 2 days, 10 days, and 3 months postsurgery in efforts to provide a preliminary determination of the prevalence rate of women who suffer from neuropathic pain post breast cancer surgery (PPBCS) and explored potential risk factors associated with its development (49). Twenty-three percent of the patients developed PPBCS. Younger age (younger than 50 years old), more invasive surgery, acute postoperative pain, and less analgesic use during the acute postoperative period were factors associated with the development of PPBCS (before surgery and 2 days, 10 days, and 3 months postsurgery (49).
Sipilä and colleagues conducted a prospective study to develop a screening tool to identify presurgical demographic, psychological and treatment related factors that predict persistence of significant pain in the operated area after 6 months from surgery (50). A six-factor risk index was developed to estimate the risk of developing significant PPBCS. Report of preoperative chronic pain, more than four or more previous operations, preoperative pain in the area to be operated, high body mass index, previous smoking and older age were included in the six-factor model that best predicted significant pain at the follow-up in the 489 women studied (A six-factor risk index was developed to estimate the risk of developing significant pain after breast cancer surgery). Most of the risk factors (e.g., old age, chronic pain conditions, previous smoking and a high number of previous operations) cannot, however, be specifically targeted in efforts to actively modify PPBCS (50).
Miaskowski and colleagues recruited 398 patients prior to breast cancer surgery and followed them for 6 months (51). Using growth mixture modeling, patients were classified into no (31.7%), mild (43.4%), moderate (13.3%), and severe (11.6%) pain groups based on ratings of worst breast pain. Patients in the moderate and severe pain classes reported higher preoperative levels of depression, anxiety, and sleep disturbance than the no pain class. Findings suggest that approximately 25% of women experience significant and persistent levels of breast pain in the first 6 months following breast cancer surgery. Severe breast pain is associated with clinically meaningful decrements in functional status and quality of life (51).
Carriers of the minor allele for a single nucleotide polymorphism (SNP) in interleukin (IL) 1-receptor 1 (IL1R1) (rs2110726) were less likely to report breast pain prior to surgery (P=0.007). Carriers of the minor allele for a SNP in IL13 (rs1295686) were more likely to report breast pain prior to surgery (P=0.019) (52). These findings suggest that breast pain occurs in over a quarter of women who are about to undergo breast cancer surgery likely in part due to difference in inflammatory mechanisms (52).
Edwards and colleagues used quantitative sensory testing to compare psychophysical responses to standardized noxious stimulation in two groups of women who had previously underwent breast cancer surgery: women with (n=37) and without (n=34) persistent postoperative pain (53). Their findings suggested that women with persistent pain after breast cancer surgery display enhanced temporal summation of mechanical pain, deficits in endogenous pain inhibition, and more intense painful aftersensations compared with those without long-term pain, suggesting that persistent postoperative pain may be associated with alterations in central nervous system (CNS) pain-modulatory processes (53).
It appears that not only is there a significant degree of persistent pain after breast cancer surgery, but there is also a significant degree of sleep disturbances after breast cancer surgery. Van Onselen et al. published the findings of 390 women who completed self-report measures for a variety of symptoms, 28.2% reported pain in their breast prior to surgery (54). A higher percentage of women in the pain group (i.e., 66.7% versus 53.5%) reported clinically meaningful levels of sleep disturbance (54).
Classification of PPBCS
Jung and colleagues distinguished four different types of PPBCS based on the studies of the epidemiology, mechanisms, and treatment for PPBCS (35). Other contributors to the neuropathic pain following breast cancer surgery are damages to the medial and lateral pectoral, long thoracic, or thoracodorsal nerves, which are routinely spared but may be injured by scarring or by traction during mastectomy (Table 1) (35,55).
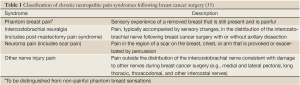
Full table
Estimates for the risk of a painful neuroma following breast cancer surgery also vary widely, ranging from 23% to 49% (35). Neuroma pain may be more common following lumpectomy than mastectomy; Tasmuth et al. (56) [1995] reported that patients who had lumpectomy, axillary dissection, and radiotherapy were significantly more likely to have scar pain than those who had a modified radical mastectomy. Anecdotal reports suggest that resection of intercostal neuromas may alleviate chronic pain after breast cancer surgery (57). However, because a neuroma can reform following excision, relocation to a protected site and attempts to improve regeneration using nerve grafts are the current major neurosurgical treatment options (58,59).
Although there are many etiologies for post-operative pain, the diagnosis of an intercostal neuroma is important as this can be treated surgically. Nguyen and colleagues described three cases of an intercostal neuroma in patients with breast implants (60). A Tinel’s sign can be elicited along the lateral chest wall and a local anesthetic block temporarily alleviates this pain. Surgical management with identification and clipping of the intercostal neuroma and burying it into the underlying muscle significantly decreases post-operative pain for the long term (60).
Kojima and colleagues mailed a questionnaire to 647 specialist members of the Breast Cancer Society in Japan. While PPBCS was recognized by as much as 70.5% of responding physicians, it was treated by as little as 47.7% of the responders (61). In contrast to a prevalent use of non-steroidal anti-inflammatory drugs (NSAIDs), which were proved to be ineffective for PPBCS, were used by 78.4% of the responders, more effective drugs were rarely used; therefore, the treatment was considered ineffective by 69.5% (61). Thus, it appears that a significant number of physicians may not be familiar with optimal therapeutic strategies to address PPBCS.
Treatment strategies to ameliorate PPBCS
There are very few randomized, double-blind, placebo controlled trials on PPBCS. In the only randomized controlled trial of topical capsaicin, crossover treatment with capsaicin versus placebo in 25 patients diagnosed with PPBCS was associated with significantly greater pain relief and reduction in jabbing pain, although the treatment groups did not differ in the relief of steady pain and allodynia (62).
Few drugs have been systematically tested in randomized clinical trials for efficacy specifically for post-mastectomy/lumpectomy pain (PMLP). However, gabapentin, an antiepileptic drug, and venlafaxine, a serotonin-norepinephrine reuptake inhibitor (SNRI), appear to be effective in multiple trials involving PMLP. Both drugs attenuated existing chronic pain in women who had previously received breast cancer surgery (63,64). When administered before surgery, gabapentin decreased the time to first post-operative analgesic administration as well as pain scores and adjuvant analgesic use within the first 10 days. However, no effect was observed on long-term chronic pain in the two studies that inquired 3 and 6 months post-surgery (65-67).
Amitriptyline has been examined in a randomized, double-blind, placebo-controlled, crossover trial of neuropathic pain following breast cancer surgery (68). Pain relief was significantly greater with amitriptyline than placebo, and eight of 15 patients reported at least 50% decrease in their pain intensity; five of these patients, however, did not want to continue treatment after the trial ended because of adverse effects.
Tasmuth and colleagues conducted a randomized, double-blind, placebo-controlled, crossover trial and failed to reveal a significant benefit of venlafaxine versus placebo on the primary endpoint (daily pain diary ratings) but did report a greater relief associated with venlafaxine treatment for two secondary endpoints, pain relief and maximum pain (64).
Perioperative treatment with eutectic mixture of local anesthetics (EMLA), mexiletine, or gabapentin appeared to reduce acute post-operative pain, including spontaneous and movement-associated pain, and decreased postoperative analgesic consumption (66,69), however, in the initial study gabapentin and mexiletine did not diminish the incidence or intensity of PPBCS. An eutectic cream mixture of local anesthetics (EMLA) alone may be beneficial as a pre-surgical treatment preventing chronic postoperative pain. When topically administered to the breast and arm area at one day prior to surgery, EMLA decreased analgesic consumption between 2 and 6 days post-surgery and the incidence and intensity of pain 3 months after surgery (69). Similar results were obtained when the same investigators combined EMLA and gabapentin in pre-operative treatment (70).
Grigoras and colleagues conducted a prospective randomized, double-blinded study regarding PPBCT and found that intravenous perioperative lidocaine decreases the incidence and severity of PPBCS (71). Two (11.8%) patients in the lidocaine group and 9 (47.4%) patients in the control group reported PPBCS at 3 months follow-up (P=0.031). McGill Pain Questionnaire revealed greater present pain intensity-visual analog scale (VAS) in the control group (14.6±22.5 vs. 2.6±7.5, P=0.025). Secondary hyperalgesia (pain outside the surgical area) was significantly less in the lidocaine group compared with control group (0.2±0.8 vs. 3.2±4.5 cm, P=0.002) (71).
Dexmedetomidine shows a dose-dependent antiallodynic effect on mechanical and cold stimuli in vincristine-evoked neuropathic rat models (72). Jain and colleagues conducted a prospective double-blind trial to analyze the role of perioperatively administered dexmedetomidine on the occurrence of chronic pain in women who underwent surgery for breast cancer (73).
In total, 84 cases (42 in group D and 42 in group C) were analyzed for acute pain and 69 (34 in group D and 35 in group C) for chronic pain. The consumption of isoflurane/fentanyl intra-operatively and acetaminophen postoperatively was significantly lower in dexmedetomidine group. The verbal numerical score (VNS) at rest and after movement was significantly lower in dexmedetomidine group at corresponding times (except at 60 min) throughout the assessment period. The brief pain inventory (BPI) and the short-form of the revised McGill Pain Questionnaire (SF-MPQ2) scores were significantly lower in dexmedetomidine group in most of the factors. The quality of life scale (QOLS) score was significantly better in dexmedetomidine group in almost all items (73). They concluded that the perioperative infusion of dexmedetomidine has a pivotal role in attenuating the incidence and severity of chronic pain and improving the quality of life in cases undergoing breast cancer surgery (73).
Paravertebral nerve blocks (PVB) during breast cancer surgery have been reported to decrease acute pain and opioid consumption immediately following surgery in multiple randomized clinical trials (74-76). Andreae and Andreae performed a Cochrane Review which included RCTs comparing local anesthetics or regional anesthesia versus conventional analgesia with a pain outcome at six or 12 months after surgery (77). They pooled two studies on PVB for breast cancer surgery; the pooled data of 89 participants with outcomes at five to six months favored PVB with an OR of 0.37 (95% CI: 0.14 to 0.94).The methodological quality of the included studies was intermediate. They concluded that PVB may reduce the risk of chronic pain after breast cancer surgery in about one out of every five women treated, although limitations of the study may include performance bias, short comings in allocation concealment attrition, and incomplete outcome data (77).
There are also risk factors for PPBCS, chronic preoperative pain, axillary surgery and psychological robustness significantly predicted acute pain outcomes after surgery for breast cancer. Preoperative identification and targeted intervention of risk subgroups could conceivably enhance the recovery trajectory in cancer survivors (78). Strategies aimed at controlling acute and chronic pain in patients receiving mastectomy and breast reconstruction include: minimally invasive therapies for breast cancer, such as breast conserving therapies of mastectomies and breast reconstruction, sentinel node biopsies, and early treatments of radiation and chemotherapy (79).
Persistent pain after breast cancer hormonal therapy (PPBCHT)
Previous studies suggested that hormonal disturbance contribute to breast cancer, thus hormonal therapies are recommend. Arthralgias, a common side effect of aromatase inhibitors, can produce painful mobility limitations and impaired daily activities (80,81). Compared with tamoxifen, aromatase inhibitors (AIs) such as anastrozole, letrozole, and exemestane show increased disease-free survival benefits; they have therefore become the standard of care for adjuvant endocrine treatment of postmenopausal women with hormone receptor - positive early breast cancer (82).
Din et al. reviewed the incidence of musculoskeletal symptoms in phase III clinical trials of anastrozole, letrozole, and exemestane (83), and women on those AIs have shown significantly higher rates of arthralgia than with tamoxifen. In a specific study investigating arthralgia in 200 patients on AIs, 47% of patients reported AI-related joint pain, and 44% reported stiffness (84). Typically, patients on AIs experience stiffness, aches, or pain that is frequently symmetric, occurring in the hands, arms, knees, feet, and pelvic and hip bones (85,86). In addition, patients on AIs may develop tenosynovial changes, including fluid in the tendon sheath, increased tendon thickness, trigger finger, and carpal tunnel syndrome (87-89).
Robidoux and colleagues conducted a prospective pilot study investigating the musculoskeletal pain in postmenopausal breast cancer patients receiving aromatase inhibitor therapy (90). Over the 24-week study period, 20 participants (67%) showed no pain symptoms; 5 (17%) experienced low or moderate pain at baseline, which did not increase with AI treatment. During therapy, 5 (17%) showed exacerbation of pain attributable to osteoarthritis of the hand and to finger flexor tenosynovitis. Although all 30 participants had some degree of musculoskeletal conditions before anastrozole therapy started, the pre-existing conditions did not necessarily predispose the women to increased pain during anastrozole treatment (90).
Baseline musculoskeletal assessment showed pre-existing causes for pain in most of the study patients before initiation of the AIs. Exacerbation of existing osteoarthritis pain and tenosynovial symptoms was the primary contributors of pain increase. Musculoskeletal pain assessment at baseline and prompt treatment of pain symptoms may help optimize adherence to AI therapy. The value of routinely assessing inflammatory markers such as C-reactive protein and erythrocyte sedimentation rate was not supported by the pilot study. Gene expression profiles in peripheral blood mononuclear cells may be further explored in larger-scale studies as stratification markers to identify patients at risk of developing arthralgia (90).
Persistent pain after breast cancer chemotherapy (PPBCC)
During the advanced stage for breast cancer, metastasis is a big challenge to patients and physicians and are currently be dealt with chemotherapy using drugs including anthracyclines, taxanes, alkylating agents, vinca alkaloids, capecitabine, gemcitabine, and the platinum agents, --- carboplatin and cisplatin. The taxanes, platinum agents, and vinca alkaloids are most likely to cause PPBCC (35,91).
Thus, women with metastatic breast cancer may have high chance of developing CIPN because of increased exposure to taxanes, antimetabolite chemotherapies, and other standard medications associated with peripheral neuropathy (92). CIPN poses both psychosocial and physical problems that may lead to decrease or halt potentially effective treatments because of dose related toxicity (93,94). Symptoms of CIPN include numbness, tingling, weakness, and pain that can impair function and activities of daily living, as well as balance, leading to falls and injury (93,95).
Andersen and colleagues compared patients treated with cyclophosphamide, epirubicin and fluorouracil (CEF) and cyclophosphamide and epirubicin + docetaxel (CE + T) in relation to PPBCT, sensory disturbances, peripheral sensory disturbances and functional impairment (96). Patients treated with CE + T had a lower risk of sensory disturbances in the surgical area compared with CEF, OR 0.75 (95% CI: 0.62-0.90), P=0.002. More CE + T patients reported peripheral sensory disturbances in the hands, OR 1.56 (95% CI: 1.27-1.92), P<0.0001, and in the feet, OR 2.0 (95% CI: 1.66-2.42) P<0.0001, compared to CEF. There was no difference in functional impairment (P=0.62). Docetaxcel as adjuvant treatment for breast cancer does not increase the risk of PPBCT, sensory disturbances in the surgical area or functional impairment, but increase risk for peripheral sensory disturbances (96).
Golan-Vered and Pud stated that the three major main findings of their descriptive study of breast cancer patients who received paclitaxel (97) were: (I) 2 distinct groups of patients with breast cancer, namely Low Cluster and High Cluster, were identified on the basis of their experiences with 4 highly prevalent symptoms (depression, fatigue, sleep disturbances, pain); (II) 50% of the patients treated with paclitaxel developed CINP; (III) a combination of CINP and clusters revealed a subgroup with no evidence of CINP within the Low Cluster group (35%) and a subgroup with CINP within the High Cluster group (22.5%). These 2 subgroups may be viewed as “double lucky” and “double unlucky”, respectively (97).
Paclitaxel is one of the chemotherapeutic treatments of breast cancer that is associated with a high frequency of peripheral neuropathy in a dose- and exposure-dependent manner. It is characterized first by paresthesias, followed by dysesthesias (91,98).
Reyes-Gibby and colleagues conducted a survey of breast cancer patients who had participated in clinical trials of paclitaxel (99). Results showed that 64% experienced CIPN during paclitaxel treatment. Follow-up survey data revealed that 27% of those with CIPN were subsequently diagnosed with neuropathic pain (NP). Logistic regression analyses showed that those who had experienced CIPN were 3 times more likely to develop NP. (95% CI: 1.2-7.2; P<0.001), which persisted in the multivariate logistic model. In addition, NP patients reported twice as many visits to their health care provider (P=0.02) and had taken more prescription (50% vs. 19%; P=0.001) and over-the-counter medications (62.5% versus 45%; P=0.08) for pain than those without NP (99). There are no specific therapies for PPBCC, the treatment of PPBCC is essentially the same as for any treatment of pain after chemotherapy treatments.
Persistent pain after breast cancer radiation (PPBCR)
Radiotherapy may cause persistent pain in the breast cancer survivors (100). No specific therapies for PPBCR are now available, and patients receive the general treatment of pain after radiation treatments.
Hofsø and colleagues conducted a study in which they evaluated the changes in and predictors of occurrence, severity, and distress of six common symptoms (lack of energy, worrying, difficulty sleeping, feeling drowsy, sweats, and pain) during radiation therapy (RT) for breast cancer (23). Their findings suggest that these six symptoms occur at relatively high rates, are of moderate severity, and are associated with moderate levels of distress. An important finding is that some of the symptoms (e.g., feeling drowsy) exhibited complex trajectories of occurrence, severity and distress. In contrast, some symptoms (e.g., pain) persisted (at the same level) over the six months of the study (23).
The risk of developing any late complications after conventionally fractionated megavoltage radiotherapy is estimated to be as below as 1% (101). Although, not entirely clear, it appears that pain in the arm or shoulder due to radiation-induced brachial plexopathy (RBP) may be more likely after hypofractionation in radiotherapy than after conventional treatment employ 2 Gy/day fraction (101-103).
The most common radiation-induced neural insult is RBP. Pierce et al. (104) in their review of 1,624 patients revealed RBP in 1.8% of patients. Other investigators (105-107) have found the incidence of this complication to be less than 1%, whereas Olsen and co-workers (108) in a study of 161 breast cancer patients with a median follow-up period of 50 months, reported that 5% and 9% had a disabling and mild RBP, respectively. Symptoms began from six months to 20 years after radiotherapy (median time 1.5 years) (109). Most patients developed symptoms within three years, but late presentations at 8-20 years later were encountered. Symptoms were progressive in all patients, though the rate did vary. Pain was common and persisted indefinitely in all but one patient. Progressive weakness was universal and resulted in loss of any useful hand function in all but three patients. The time taken to loss of useful hand function ranged from six weeks to five years (median 1.25 years). Three patterns of upper limb weakness were identified, distal limb weakness only (13 patients), global limb weakness that was more marked distally (11 patients), and completely flaccid arm (10 patients). Seventeen patients required long-term morphine to palliate pain. A chemical sympathectomy benefited three of six patients that received the injection (109).
The pathophysiology of radiation-induced neuropathies is incompletely understood. It is currently possible to target radiation-induced fibrosis and associated factors such as ischemia, oxidative stress and inflammation as well as other pathophysiologic mechanisms suspected of contributing to radiation-induced neuropathies (110,111). A phase III trial evaluating the association of pentoxifylline, tocopherol and clodronate (PENTOCLO, NCT01291433) in radiation-induced neuropathies is now recruiting (110).
Non-pharmacologic treatment of PPBCT
Exercise programs that combine aerobic exercise and resistance training as well as various rehabilitation physical medicine techniques among breast cancer patients and survivors may effectively reduce side effects (112-120). A few of these studies are presented. Early stage breast cancer survivors receiving chemotherapy and/or radiation who participated in an aerobic and resistance exercise intervention 2 days a week for 12 weeks reported improvements in CRF, QOL, satisfaction with life, and also improvement in physical function compared to usual care (121,122). Mustian and colleagues (123) have also demonstrated the benefits of performing aerobic and resistance exercise during radiation treatment. A four week individually tailored, home based aerobic and resistance training program resulted in improved CRF, QOL, sleep, aerobic capacity, strength and immune function (123-124).
Women with breast cancer have reported using many of these Complementary and Alternative medicine (CAM) techniques in conjunction with their treatment or after the completion of their treatment. CAM includes natural products, mind body medicine, and manipulative and body-based practices, Mindfulness-based stress reduction (MBSR) [mediation, postures], Mindfulness-based exercise [Tai Chi Chuan, Yoga], as well as acupuncture.
Jensen et al. performed a pilot study to provide initial support for hypnosis alleviating PPBCT as well as other symptoms (125).
An 8-week water therapy program was effective for improving neck and shoulder/axillary pain, and reducing the presence of trigger points in breast cancer survivors as compared with usual care; however, no significant changes in widespread pressure pain hyperalgesia were found (126).
Wong and colleagues evaluated breast cancer patients with moderate-to-severe PPBCT at 3-6 months after completion of all adjuvant treatments in a pilot study (127). These patients participated in a 12-week comprehensive health improvement program (CHIP) involving exercise training. Intensity was adjusted to reach 65-85% of the patient’s maximal heart rate.
Before the CHIP and at 1 and 6 months after completion of the CHIP, QOL and pain were measured using questionnaires [European Organization for Research and Treatment of Cancer Quality of Life core and breast cancer modules (qlq-C30, -BR23) and the McGill Pain Questionnaire short form] completed by the patients. The CHIP team consists of an internist, an oncologist or palliative care physician, a psychologist, a nurse, a physiotherapist, a dietician, and a clinic manager, who together provide the patient with information, treatment, and support. After the CHIP, patients reported significant and clinically important improvements in QOL and symptoms. At 1 and 6 months post-CHIP, patients in the study felt, on average, better in overall QOL than did historical control subjects.
Surgery and radiotherapy are thought to cause acute and chronic breast pain, tenderness, and shoulder impairments in up to 50% of patients who complete breast-conserving therapy (56,128-132). The U.K. START (Standardization of Breast Radiotherapy) trial, which compared hypofractionation with conventional fractionation of adjuvant radiotherapy for breast cancer, assessed the QOL of 2208 patients over 5 years (102). It was observed that 20% and 30% of the patients from both arms of the study experienced breast and arm pain respectively at 5 years of follow-up (102). Randomized controlled studies have shown that, compared with control patients who received no interventions, breast cancer patients directed to exercise more frequently after their diagnosis experienced improvements in physical functioning, overall QOL, and cardiopulmonary functioning (133,134). In 2006, the McGill CHIP, which was originally developed for patients with cardiovascular disease, started to include an exercise rehabilitation program to help cancer survivors recover and reach their full health potential once they had completed their cancer treatments.
Summary
Improved breast cancer survival rates appear to have contributed to the revelation of the significant clinical issue of PPBCT. Persistent pain may occur after surgical treatment, hormonal treatment, chemotherapy and/or radiotherapy. Treatment approaches for PPBCT may include pharmacologic, interventional, and nonpharmacolgic strategies. Currently therapy for PPBCT remains suboptimal, however, it is hoped that a greater appreciation of the diagnosis, evaluation, and management of PPBCT may lead to improved overall patient outcomes with better analgesia and less adverse effects.
Acknowledgements
The author would like to thank Pya Seidner for her enormous assistance in the preparation of this manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Janelsins MC, Mustian KM, Peppone LJ, et al. Interventions to Alleviate Symptoms Related to Breast Cancer Treatments and Areas of Needed Research. J Cancer Sci Ther 2011;S2. pii:S2-001.
- Janelsins MC, Kohli S, Mohile SG, et al. An update on cancer- and chemotherapy-related cognitive dysfunction: current status. Semin Oncol 2011;38:431-8.
- Ahles TA, Saykin AJ, McDonald BC, et al. Longitudinal assessment of cognitive changes associated with adjuvant treatment for breast cancer: impact of age and cognitive reserve. J Clin Oncol 2010;28:4434-40.
- Ahles TA, Saykin A. Cognitive effects of standard-dose chemotherapy in patients with cancer. Cancer Invest 2001;19:812-20.
- Wefel JS, Vardy J, Ahles T, et al. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol 2011;12:703-8.
- Wieneke MH, Dienst ER. Neuropsychological assessment of cognitive functioning following chemotherapy for breast cancer. Psycho-Oncology 1995;4:61-6.
- Wagner LI, Sweet J, Butt Z, et al. Measuring Patient Self-Reported Cognitive Function: Development of the Functional Assessment of Cancer Therapy-Cognitive Function Instrument. J Support Oncol 2009;7:32-9.
- van Dam FS, Schagen SB, Muller MJ, et al. Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: high-dose versus standard-dose chemotherapy. J Natl Cancer Inst 1998;90:210-8.
- Schagen SB, van Dam FS, Muller MJ, et al. Cognitive deficits after postoperative adjuvant chemotherapy for breast carcinoma. Cancer 1999;85:640-50.
- Morrow GR, Shelke AR, Roscoe JA, et al. Management of cancer-related fatigue. Cancer Invest 2005;23:229-39.
- Mustian KM, Peppone LJ, Palesh OG, et al. Exercise and cancer-related fatigue. US Oncol 2010;6:20-3.
- Fan HG, Houédé-Tchen N, Yi QL, et al. Fatigue, menopausal symptoms, and cognitive function in women after adjuvant chemotherapy for breast cancer: 1- and 2-year follow-up of a prospective controlled study. J Clin Oncol 2005;23:8025-32.
- Palesh OG, Roscoe JA, Mustian KM, et al. Prevalence, demographics, and psychological associations of sleep disruption in patients with cancer: University of Rochester Cancer Center-Community Clinical Oncology Program. J Clin Oncol 2010;28:292-8.
- Baum M, Buzdar A, Cuzick J, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early-stage breast cancer: results of the ATAC (Arimidex, Tamoxifen Alone or in Combination) trial efficacy and safety update analyses. Cancer 2003;98:1802-10.
- Coates AS, Keshaviah A, Thürlimann B, et al. Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1-98. J Clin Oncol 2007;25:486-92.
- BIG 1-98 Collaborative Group, Mouridsen H, Giobbie-Hurder A, et al. Letrozole therapy alone or in sequence with tamoxifen in women with breast cancer. N Engl J Med 2009;361:766-76.
- Diller L, Chow EJ, Gurney JG, et al. Chronic disease in the Childhood Cancer Survivor Study cohort: a review of published findings. J Clin Oncol 2009;27:2339-55.
- Mertens AC, Yasui Y, Neglia JP, et al. Late mortality experience in five-year survivors of childhood and adolescent cancer: the Childhood Cancer Survivor Study. J Clin Oncol 2001;19:3163-72.
- Chen Z, Maricic M, Pettinger M, et al. Osteoporosis and rate of bone loss among postmenopausal survivors of breast cancer. Cancer 2005;104:1520-30.
- Twiss JJ, Waltman N, Ott CD, et al. Bone mineral density in postmenopausal breast cancer survivors. J Am Acad Nurse Pract 2001;13:276-84.
- Reid-Arndt SA, Yee A, Perry MC, et al. Cognitive and psychological factors associated with early posttreatment functional outcomes in breast cancer survivors. J Psychosoc Oncol 2009;27:415-34.
- Ma AM, Barone J, Wallis AE, et al. Noncompliance with adjuvant radiation, chemotherapy, or hormonal therapy in breast cancer patients. Am J Surg 2008;196:500-4.
- Hofsø K, Rustøen T, Cooper BA, et al. Changes Over Time in Occurrence, Severity, and Distress of Common Symptoms During and After Radiation Therapy for Breast Cancer. J Pain Symptom Manage 2012. [Epub ahead of print].
- Burton AW, Fanciullo GJ, Beasley RD, et al. Chronic pain in the cancer survivor: a new frontier. Pain Med 2007;8:189-98.
- Merskey H, Bogduk N. eds. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms, 2nd ed. Seattle: IASP Press, 1994.
- Poleshuck EL, Katz J, Andrus CH, et al. Risk factors for chronic pain following breast cancer surgery: a prospective study. J Pain 2006;7:626-34.
- Andersen KG, Kehlet H. Persistent pain after breast cancer treatment: a critical review of risk factors and strategies for prevention. J Pain 2011;12:725-46.
- Bennett MI, Rayment C, Hjermstad M, et al. Prevalence and aetiology of neuropathic pain in cancer patients: a systematic review. Pain 2012;153:359-65.
- van den Broeke EN, de Vries M, van Goor H, et al. Patients with persistent pain after breast cancer surgery show both delayed and enhanced cortical stimulus processing. J Pain Res 2012;5:139-50.
- Rosedale M, Fu MR. Confronting the unexpected: temporal, situational, and attributive dimensions of distressing symptom experience for breast cancer survivors. Oncol Nurs Forum 2010;37:E28-33.
- Bender JL, Hohenadel J, Wong J, et al. What patients with cancer want to know about pain: a qualitative study. J Pain Symptom Manage 2008;35:177-87.
- Peretti-Watel P, Bendiane MK, Spica L, et al. Pain narratives in breast cancer survivors. Pain Res Treat 2012;2012:153060.
- Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin 2012;62:283-98.
- Stevens PE, Dibble SL, Miaskowski C. Prevalence, characteristics, and impact of postmastectomy pain syndrome: an investigation of women's experiences. Pain 1995;61:61-8.
- Jung BF, Ahrendt GM, Oaklander AL, et al. Neuropathic pain following breast cancer surgery: proposed classification and research update. Pain 2003;104:1-13.
- Stubblefield MD, Custodio CM. Upper-extremity pain disorders in breast cancer. Arch Phys Med Rehabil 2006;87:S96-9; quiz S100-1.
- Carpenter JS, Andrykowski MA, Sloan P, et al. Postmastectomy/postlumpectomy pain in breast cancer survivors. J Clin Epidemiol 1998;51:1285-92.
- Alves Nogueira Fabro E, Bergmann A, do Amaral E Silva B, et al. Post-mastectomy pain syndrome: incidence and risks. Breast 2012;21:321-5.
- Aasvang E, Kehlet H. Chronic postoperative pain: the case of inguinal herniorrhaphy. Br J Anaesth 2005;95:69-76.
- Wildgaard K, Ravn J, Kehlet H. Chronic post-thoracotomy pain: a critical review of pathogenic mechanisms and strategies for prevention. Eur J Cardiothorac Surg 2009;36:170-80.
- Gärtner R, Jensen MB, Nielsen J, et al. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA 2009;302:1985-92.
- Levangie PK, Drouin J. Magnitude of late effects of breast cancer treatments on shoulder function: a systematic review. Breast Cancer Res Treat 2009;116:1-15.
- Andersen KG, Jensen MB, Tvedskov TF, et al. Persistent pain, sensory disturbances and functional impairment after immediate or delayed axillary lymph node dissection. Eur J Surg Oncol 2013;39:31-5.
- Foley KM. Pain syndromes in patients with cancer. Med Clin North Am 1987;71:169-84.
- Vecht CJ. Arm pain in the patient with breast cancer. J Pain Symptom Manage 1990;5:109-17.
- Wallace MS, Wallace AM, Lee J, et al. Pain after breast surgery: a survey of 282 women. Pain 1996;66:195-205.
- de Vries JE, Timmer PR, Erftemeier EJ, et al. Breast pain after breast conserving therapy. Breast J 1994;3:151-4.
- Ivens D, Hoe AL, Podd TJ, et al. Assessment of morbidity from complete axillary dissection. Br J Cancer 1992;66:136-8.
- Bokhari FN, McMillan DE, McClement S, et al. Pilot study of a survey to identify the prevalence of and risk factors for chronic neuropathic pain following breast cancer surgery. Oncol Nurs Forum 2012;39:E141-9.
- Sipilä R, Estlander AM, Tasmuth T, et al. Development of a screening instrument for risk factors of persistent pain after breast cancer surgery. Br J Cancer 2012;107:1459-66.
- Miaskowski C, Cooper B, Paul SM, et al. Identification of patient subgroups and risk factors for persistent breast pain following breast cancer surgery. J Pain 2012;13:1172-87.
- McCann B, Miaskowski C, Koetters T, et al. Associations between pro- and anti-inflammatory cytokine genes and breast pain in women prior to breast cancer surgery. J Pain 2012;13:425-37.
- Edwards RR, Mensing G, Cahalan C, et al. Alteration in Pain Modulation in Women With Persistent Pain After Lumpectomy: Influence of Catastrophizing. J Pain Symptom Manage 2012. [Epub ahead of print].
- Van Onselen C, Aouizerat BE, Dunn LB, et al. Differences in sleep disturbance, fatigue and energy levels between women with and without breast pain prior to breast cancer surgery. Breast 2012. [Epub ahead of print].
- Wallace AM, Wallace MS. Postmastectomy and postthoracotomy pain. Anesth Clin North Am 1997;15:353-70.
- Tasmuth T, von Smitten K, Hietanen P, et al. Pain and other symptoms after different treatment modalities of breast cancer. Ann Oncol 1995;6:453-9.
- Wong L. Intercostal neuromas: a treatable cause of postoperative breast surgery pain. Ann Plast Surg 2001;46:481-4.
- Burchiel KJ. Neurosurgical procedures of the peripheral nerves. In: North RB, Levy RM. eds. Neurosurgical management of pain. New York: Springer-Verlag, 1997:133-61.
- Campbell JN. Peripheral nerve injury and sympathetically maintained pain: mechanisms and surgical approach. In: North RB, Levy RM. eds. Neurosurgical management of pain. New York: Springer-Verlag, 1997:75-82.
- Nguyen JT, Buchanan IA, Patel PP, et al. Intercostal neuroma as a source of pain after aesthetic and reconstructive breast implant surgery. J Plast Reconstr Aesthet Surg 2012;65:1199-203.
- Kojima KY, Kitahara M, Matoba M, et al. Survey on recognition of post-mastectomy pain syndrome by breast specialist physician and present status of treatment in Japan. Breast Cancer 2012. [Epub ahead of print].
- Watson CP, Evans RJ. The postmastectomy pain syndrome and topical capsaicin: a randomized trial. Pain 1992;51:375-9.
- Patarica-Huber E, Boskov N, Pjevic M. Multimodal approach to therapy-related neuropathic pain in breast cancer. J BUON 2011;16:40-5.
- Tasmuth T, Härtel B, Kalso E. Venlafaxine in neuropathic pain following treatment of breast cancer. Eur J Pain 2002;6:17-24.
- Amr YM, Yousef AA. Evaluation of efficacy of the perioperative administration of Venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain 2010;26:381-5.
- Fassoulaki A, Patris K, Sarantopoulos C, et al. The analgesic effect of gabapentin and mexiletine after breast surgery for cancer. Anesth Analg 2002;95:985-91, table of contents.
- Grover VK, Mathew PJ, Yaddanapudi S, et al. A single dose of preoperative gabapentin for pain reduction and requirement of morphine after total mastectomy and axillary dissection: randomized placebo-controlled double-blind trial. J Postgrad Med 2009;55:257-60.
- Kalso E, Tasmuth T, Neuvonen PJ. Amitriptyline effectively relieves neuropathic pain following treatment of breast cancer. Pain 1996;64:293-302.
- Fassoulaki A, Sarantopoulos C, Melemeni A, et al. EMLA reduces acute and chronic pain after breast surgery for cancer. Reg Anesth Pain Med 2000;25:350-5.
- Fassoulaki A, Triga A, Melemeni A, et al. Multimodal analgesia with gabapentin and local anesthetics prevents acute and chronic pain after breast surgery for cancer. Anesth Analg 2005;101:1427-32.
- Grigoras A, Lee P, Sattar F, et al. Perioperative intravenous lidocaine decreases the incidence of persistent pain after breast surgery. Clin J Pain 2012;28:567-72.
- Park HJ, Kim YH, Koh HJ, et al. Analgesic effects of dexmedetomidine in vincristine-evoked painful neuropathic rats. J Korean Med Sci 2012;27:1411-7.
- Jain G, Bansal P, Ahmad B, et al. Effect of the perioperative infusion of dexmedetomidine on chronic pain after breast surgery. Indian J Palliat Care 2012;18:45-51.
- Kairaluoma PM, Bachmann MS, Rosenberg PH, et al. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg 2006;103:703-8.
- Moller JF, Nikolajsen L, Rodt SA, et al. Thoracic paravertebral block for breast cancer surgery: a randomized double-blind study. Anesth Analg 2007;105:1848-51, table of contents.
- Coveney E, Weltz CR, Greengrass R, et al. Use of paravertebral block anesthesia in the surgical management of breast cancer: experience in 156 cases. Ann Surg 1998;227:496-501.
- Andreae MH, Andreae DA. Local anaesthetics and regional anaesthesia for preventing chronic pain after surgery. Cochrane Database Syst Rev 2012;10:CD007105.
- Bruce J, Thornton AJ, Scott NW, et al. Chronic preoperative pain and psychological robustness predict acute postoperative pain outcomes after surgery for breast cancer. Br J Cancer 2012;107:937-46.
- Vadivelu N, Schreck M, Lopez J, et al. Pain after mastectomy and breast reconstruction. Am Surg 2008;74:285-96.
- Winters L, Habin K, Flanagan J, et al. “I feel like I am 100 years old!” managing arthralgias from aromatase inhibitors. Clin J Oncol Nurs 2010;14:379-82.
- Winters-Stone KM, Schwartz AL, Hayes SC, et al. A prospective model of care for breast cancer rehabilitation: bone health and arthralgias. Cancer 2012;118:2288-99.
- Burstein HJ, Prestrud AA, Seidenfeld J, et al. American Society of Clinical Oncology clinical practice guideline: update on adjuvant endocrine therapy for women with hormone receptor-positive breast cancer. J Clin Oncol 2010;28:3784-96.
- Din OS, Dodwell D, Wakefield RJ, et al. Aromatase inhibitor-induced arthralgia in early breast cancer: what do we know and how can we find out more? Breast Cancer Res Treat 2010;120:525-38.
- Crew KD, Greenlee H, Capodice J, et al. Prevalence of joint symptoms in postmenopausal women taking aromatase inhibitors for early-stage breast cancer. J Clin Oncol 2007;25:3877-83.
- Burstein HJ, Winer EP. Aromatase inhibitors and arthralgias: a new frontier in symptom management for breast cancer survivors. J Clin Oncol 2007;25:3797-9.
- Dizdar O, Ozçakar L, Malas FU, et al. Sonographic and electrodiagnostic evaluations in patients with aromatase inhibitor-related arthralgia. J Clin Oncol 2009;27:4955-60.
- Henry NL, Giles JT, Ang D, et al. Prospective characterization of musculoskeletal symptoms in early stage breast cancer patients treated with aromatase inhibitors. Breast Cancer Res Treat 2008;111:365-72.
- Morales L, Pans S, Paridaens R, et al. Debilitating musculoskeletal pain and stiffness with letrozole and exemestane: associated tenosynovial changes on magnetic resonance imaging. Breast Cancer Res Treat 2007;104:87-91.
- Sestak I, Sapunar F, Cuzick J. Aromatase inhibitor-induced carpal tunnel syndrome: results from the ATAC trial. J Clin Oncol 2009;27:4961-5.
- Robidoux A, Rich E, Bureau NJ, et al. A prospective pilot study investigating the musculoskeletal pain in postmenopausal breast cancer patients receiving aromatase inhibitor therapy. Curr Oncol 2011;18:285-94.
- Jung BF, Herrmann D, Griggs J, et al. Neuropathic pain associated with non-surgical treatment of breast cancer. Pain 2005;118:10-4.
- Clinical Practice Guidelines in Oncology — Breast Cancer. Fort Washington, PA: National Comprehensive Cancer Network, 2011.
- Tofthagen C. Patient perceptions associated with chemotherapy-induced peripheral neuropathy. Clin J Oncol Nurs 2010;14:E22-8.
- Guglielmino J. Getting a grip on neuropathy. Insights on Metastatic Breast Cancer: Living Beyond Breast Cancer Newsletter. Spring 2010;1.
- Stubblefield MD, McNeely ML, Alfano CM, et al. A prospective surveillance model for physical rehabilitation of women with breast cancer: chemotherapy-induced peripheral neuropathy. Cancer 2012;118:2250-60.
- Andersen KG, Jensen MB, Kehlet H, et al. Persistent pain, sensory disturbances and functional impairment after adjuvant chemotherapy for breast cancer: cyclophosphamide, epirubicin and fluorouracil compared with docetaxel + epirubicin and cyclophosphamide. Acta Oncol 2012;51:1036-44.
- Golan-Vered Y, Pud D. Chemotherapy-Induced Neuropathic Pain and Its Relation to Cluster Symptoms in Breast Cancer Patients Treated with Paclitaxel. Pain Pract 2013;13:46-52.
- Vahdat L, Papadopoulos K, Lange D, et al. Reduction of paclitaxel-induced peripheral neuropathy with glutamine. Clin Cancer Res 2001;7:1192-7.
- Reyes-Gibby CC, Morrow PK, Buzdar A, et al. Chemotherapy-induced peripheral neuropathy as a predictor of neuropathic pain in breast cancer patients previously treated with paclitaxel. J Pain 2009;10:1146-50.
- Ewertz M, Jensen AB. Late effects of breast cancer treatment and potentials for rehabilitation. Acta Oncol 2011;50:187-93.
- Gałecki J, Hicer-Grzenkowicz J, Grudzień-Kowalska M, et al. Radiation-induced brachial plexopathy and hypofractionated regimens in adjuvant irradiation of patients with breast cancer--a review. Acta Oncol 2006;45:280-4.
- Hopwood P, Haviland JS, Sumo G, et al. Comparison of patient-reported breast, arm, and shoulder symptoms and body image after radiotherapy for early breast cancer: 5-year follow-up in the randomised Standardisation of Breast Radiotherapy (START) trials. Lancet Oncol 2010;11:231-40.
- Friberg S, Rudén BI. Hypofractionation in radiotherapy. An investigation of injured Swedish women, treated for cancer of the breast. Acta Oncol 2009;48:822-31.
- Pierce SM, Recht A, Lingos TI, et al. Long-term radiation complications following conservative surgery (CS) and radiation therapy (RT) in patients with early stage breast cancer. Int J Radiat Oncol Biol Phys 1992;23:915-23.
- Delouche G, Bachelot F, Premont M, et al. Conservation treatment of early breast cancer: long term results and complications. Int J Radiat Oncol Biol Phys 1987;13:29-34.
- Fowble BL, Solin LJ, Schultz DJ, et al. Ten year results of conservative surgery and irradiation for stage I and II breast cancer. Int J Radiat Oncol Biol Phys 1991;21:269-77.
- Stotter AT, McNeese MD, Ames FC, et al. Predicting the rate and extent of locoregional failure after breast conservation therapy for early breast cancer. Cancer 1989;64:2217-25.
- Olsen NK, Pfeiffer P, Johannsen L, et al. Radiation-induced brachial plexopathy: neurological follow-up in 161 recurrence-free breast cancer patients. Int J Radiat Oncol Biol Phys 1993;26:43-9.
- Fathers E, Thrush D, Huson SM, et al. Radiation-induced brachial plexopathy in women treated for carcinoma of the breast. Clin Rehabil 2002;16:160-5.
- Pradat PF, Maisonobe T, Psimaras D, et al. Radiation-induced neuropathies: Collateral damage of improved cancer prognosis. Rev Neurol (Paris) 2012;168:939-50.
- Dropcho EJ. Neurotoxicity of radiation therapy. Neurol Clin 2010;28:217-34.
- Mustian KM, Peppone LJ, Palesh OG, et al. Exercise and cancerrelated fatigue. US Oncological Review 2010;6:20-3.
- Knols RH, de Bruin ED, Shirato K, et al. Physical activity interventions to improve daily walking activity in cancer survivors. BMC Cancer 2010;10:406.
- Schmitz K. Physical activity and breast cancer survivorship. Recent Results Cancer Res 2011;186:189-215.
- Pekmezi DW, Demark-Wahnefried W. Updated evidence in support of diet and exercise interventions in cancer survivors. Acta Oncol 2011;50:167-78.
- Duijts SF, Faber MM, Oldenburg HS, et al. Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors--a meta-analysis. Psychooncology 2011;20:115-26.
- Friedenreich CM. Physical activity and breast cancer: review of the epidemiologic evidence and biologic mechanisms. Recent Results Cancer Res 2011;188:125-39.
- Pinto BM, Ciccolo JT. Physical activity motivation and cancer survivorship. Recent Results Cancer Res 2011;186:367-87.
- Lowe SS. Physical activity and palliative cancer care. Recent Results Cancer Res 2011;186:349-65.
- Cramp F, James A, Lambert J. The effects of resistance training on quality of life in cancer: a systematic literature review and meta-analysis. Support Care Cancer 2010;18:1367-76.
- Ahmed RL, Thomas W, Yee D, et al. Randomized controlled trial of weight training and lymphedema in breast cancer survivors. J Clin Oncol 2006;24:2765-72.
- Campbell A, Mutrie N, White F, et al. A pilot study of a supervised group exercise programme as a rehabilitation treatment for women with breast cancer receiving adjuvant treatment. Eur J Oncol Nurs 2005;9:56-63.
- Mustian KM, Peppone L, Darling TV, et al. A 4-week home-based aerobic and resistance exercise program during radiation therapy: a pilot randomized clinical trial. J Support Oncol 2009;7:158-67.
- Sprod LK, Palesh OG, Janelsins MC, et al. Exercise, sleep quality, and mediators of sleep in breast and prostate cancer patients receiving radiation therapy. Community Oncol 2010;7:463-471.
- Jensen MP, Gralow JR, Braden A, et al. Hypnosis for symptom management in women with breast cancer: a pilot study. Int J Clin Exp Hypn 2012;60:135-59.
- Cantarero-Villanueva I, Fernández-Lao C, Fernández-de-Las-Peñas C, et al. Effectiveness of water physical therapy on pain, pressure pain sensitivity, and myofascial trigger points in breast cancer survivors: a randomized, controlled clinical trial. Pain Med 2012;13:1509-19.
- Wong P, Muanza T, Hijal T, et al. Effect of exercise in reducing breast and chest-wall pain in patients with breast cancer: a pilot study. Curr Oncol 2012;19:e129-35.
- Ernst MF, Voogd AC, Balder W, et al. Early and late morbidity associated with axillary levels I-III dissection in breast cancer. J Surg Oncol 2002;79:151-5; discussion 156.
- Holli K, Pitkänen M, Järvenpää R, et al. Early skin and lung reactions in breast cancer patients after radiotherapy: prospective study. Radiother Oncol 2002;64:163-9.
- Rietman JS, Dijkstra PU, Hoekstra HJ, et al. Late morbidity after treatment of breast cancer in relation to daily activities and quality of life: a systematic review. Eur J Surg Oncol 2003;29:229-38.
- Tengrup I, Tennvall-Nittby L, Christiansson I, et al. Arm morbidity after breast-conserving therapy for breast cancer. Acta Oncol 2000;39:393-7.
- Whelan TJ, Levine M, Julian J, et al. The effects of radiation therapy on quality of life of women with breast carcinoma: results of a randomized trial. Ontario Clinical Oncology Group. Cancer 2000;88:2260-6.
- Courneya KS, Mackey JR, Bell GJ, et al. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol 2003;21:1660-8.
- Segal R, Evans W, Johnson D, et al. Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol 2001;19:657-65.


