
Methodological factors regarding patient-reported outcome information for value assessment in palliative care
Introduction
The growing number of elderly patients with multiple health conditions and the consequent rise in demand for palliative care (PC) pose significant challenges to healthcare systems. Currently, it is estimated to that over 56 million individuals are in need of PC globally each year (1). This situation necessitates assessing the value of interventions and services, allowing healthcare systems to allocate resources efficiently and fairly among competing alternatives. Health economic evaluations, the comparative analysis of alternative courses of action in terms of both costs and consequences, function as a tool to inform decision making (2). One indicator usually employed to gauge the effect of interventions or services on patients within this framework is their subjective health-related quality of life (HrQoL), which encompasses both physical and psychological well-being. To facilitate this assessment, patient-reported outcome measures (PROMs) have gained in prominence. PROMs are instruments that directly collect health-related outcomes from patients through standardized questionnaires, including multi-attribute utility scores representing individuals’ health-state preferences (3). They cover diverse health dimensions and operationalize the patient-centered perspective (4); they are therefore seen to enrich economic evaluations. However, in practice, quantifying the value of PC through PROMs presents challenges for research making us of randomized controlled trials or economic evaluations (5). Alongside difficulties related to collecting PROMs, including high attrition rates due to disease progression and death (6) and the reliability problems of proxy assessments for PC patients unable to provide PROM data directly themselves (7), there are distinct methodological factors regarding the selection and measurement of PROMs in PC that might contribute to these challenges. Awareness of these factors is crucial for critically appraising study results, designing future evaluations and prioritizing methodological research in this field. Therefore, this paper aims to discuss key methodological factors related to measuring PROMs and their impact on testing the (cost-)effectiveness of interventions in PC. In this paper, we employ the term “PC” to denote an approach aimed at improving the quality of life for both patients and their families as they face problems associated with life-threatening illness (8). This includes end-of-life care as a form of PC, applicable when the patient is close to death, without being confined to any particular setting (e.g., specialized PC wards).
Selecting PROMs for evaluating the cost-effectiveness of PC interventions
At present, a clear preference has not been established for generic or setting-specific PROMs for economic evaluations of PC, given that both types of PROMs have their advantages and disadvantages in this context (9).
In curative medical care, standard methods in health economic evaluations employ utility-based health status measures to capture HrQoL information. These measures can be combined with information on length of life to develop the outcome metric quality-adjusted life years (QALYs). Note that QALYs are based on a rather narrow definition of health (10). Examples of such generic measures include the EuroQol five-dimension questionnaire (EQ-5D) and the Short-Form Six-Dimension health index (SF-6D). These measures allow direct comparisons between different patient groups, thus aiding reimbursement decisions. However, in PC, the use of generic HrQoL PROMs, which primarily focus on health gain, is criticized. PC’s distinct treatment goals compared to curative care mean that generic HrQoL PROMs may miss important quality dimensions like spiritual/psychosocial well-being or patient dignity (11-13). Ignoring these aspects in PC intervention evaluations may result in misleading conclusions (11).
In recent years, PROMs have been developed tailored specifically to patients, their families and caregivers in the PC context. Such PROMs, like the Integrated Palliative care Outcome Scale (IPOS), focus on capturing a wider array of quality-of-life dimensions beyond health status (14). For PROMs to be useful for economic evaluations, they need weighting assigned to individual items, also known as a preference-based value set. However, only a limited number of PROMs have this feature. While alternative measures employing the broader capability well-being approach, like the ICECAP Supportive Care Measure (ICECAP-SCM), are examples for context-specific PROMs equipped with assigned preference-based value sets, they still need to undergo further practical evaluation (15).
Equitable comparisons of PROM results between interventions conducted in the PC context and those in curative settings
When comparing PC interventions with those in curative settings, only the above-mentioned generic HrQoL PROMs are suitable for economic evaluations. Given that generic HrQoL PROMs might not fully capture the impact of PC interventions, different strategies for addressing the differences in cross-setting comparisons have been discussed in the literature. For instance, one method entails broadening the generic QoL framework by incorporating additional PC-specific quality domains (5,12,16), as demonstrated in areas such as pediatric care (17). Yet, critics argue that low scores on generic HrQoL PROMs can be attributed not to limited QoL improvements but to the shorter life expectancy of PC patients (5,12,13,17). Therefore, PC interventions, even moderately priced ones, might struggle to demonstrate cost-effectiveness against interventions in curative care that both enhance QoL and prolong life or prevent premature death (5,13,16).
In the literature it is also suggested that different weights may be applied to added life years to avoid the inaccurate comparison with interventions conducted in a curative setting. Traditionally, generic HrQoL PROMs assume a linear continuum between perfect health and death. Thus, all added life years are weighted alike, regardless of the point in time at which they are added (16). Yet, empirical studies investigating individual preferences for weighting life gain for end-of-life patients show mixed results, which is why the appropriateness of placing higher weighting on time that is gained later in life has been questioned in applied economic evaluations (18). It is contended that these discrepancies in weighting should not be ignored when adding up time slices (16,17). However, there is currently no formal framework to address this aspect (12). After the National Institute for Health and Care Excellence (NICE) acknowledged that their proposed end-of-life modifier had too narrow an application (19), a more inclusive severity modifier was introduced. The new modifier is based on the absolute and proportional QALY shortfall of a diseased population in comparison to a healthy one and aims to overcome the shortcomings of the previous modifier (20). Again, the need for empirical studies confirming the appropriateness of this modifier and concerns about modifiers in general are discussed in the literature (21).
Conclusions
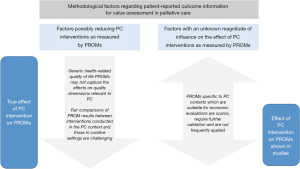
This review underscores several methodological factors linked to the selection and measurement of PROMs which could impact the (cost-)effectiveness assessment of a PC intervention. Certain factors could notably reduce the impact of a PC intervention on PROM outcomes while others may affect it to an unknown extent (Figure 1).
Ignoring these factors when planning and analyzing (economic) evaluations of PC interventions using PROM data can lead to incorrect conclusions and an improper allocation of resources. Addressing these challenges requires focused methodological research to unveil the true value of PC for patients, families and healthcare systems. To enhance cross-setting comparisons, it is essential to rigorously test both generic HrQoL PROMs and PC-specific ones in parallel in studies (16). This will lay the groundwork for subsequent methodological studies like construct validity testing and mapping studies (22,23). These analyses can then offer more profound insights into the similarities and differences between these measurement approaches. With regards to economic evaluations of PC, it will be necessary to increase the number and size of validity testing studies on available measures (e.g., ICECAP-SCM). Further research may focus on personalizing evaluation frameworks for specific groups [i.e., the Palliative Care Yardstick (PalY) (13) or Valuation Index (Palliative) (VIP) (12)], enabling certain dimensions to be incorporated more accurately, such as the caring effect on carers (13), as well as tackling valuation problems (13,17). To better understand whether different weighting schemes should be considered for the PC context when evaluating health state utilities, alternative methods, e.g., discrete choice experiments (DCEs) or best-worst scaling (BWS), should be further explored. They allow the simultaneous consideration of various patient-preference domains, a crucial aspect when evaluating complex interventions as is the case in the PC context (24), but they also allow death, as an inevitable outcome, to become “acceptable” (12).
Acknowledgments
Funding: This study has been conducted as part of the PallPROMs study, which has received funding from
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Palliative Medicine for the series “Value of Palliative Care”. The article has undergone external peer review.
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-23-364/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-23-364/coif). The series “Value of Palliative Care” was commissioned by the editorial office without any funding or sponsorship. C.F. and J.S. received support from EU Horizon 2020. E.K.M. is a Member of the Austrian Palliative Care Association. C.F. declares lecture for Paracelsus Medizinische Universität. C.F. served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Implementing World Health Assembly Resolution on Palliative care. 2021. Accessed on 12.06.2023. Available online: https://www.who.int/news/item/12-10-2021-implementing-world-health-assembly-resolution-on-palliative-care
- Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. 4th Edition. Oxford: Oxford University Press; 2015.
- Kluzek S, Dean B, Wartolowska KA. Patient-reported outcome measures (PROMs) as proof of treatment efficacy. BMJ Evid Based Med 2022;27:153-5. [Crossref] [PubMed]
- Devlin NJ, Appleby J. Getting the most out of PROMs. Putting health outcomes at the heart of NHS decision-making. London: The King's Fund; 2010.
- Hughes J. Palliative care and the QALY problem. Health Care Anal 2005;13:289-301. [Crossref] [PubMed]
- Hui D, Glitza I, Chisholm G, et al. Attrition rates, reasons, and predictive factors in supportive care and palliative oncology clinical trials. Cancer 2013;119:1098-105. [Crossref] [PubMed]
- Howland M, Allan KC, Carlton CE, et al. Patient-rated versus proxy-rated cognitive and functional measures in older adults. Patient Relat Outcome Meas 2017;8:33-42. [Crossref] [PubMed]
- WHO. National cancer control programmes: policies and managerial guidelines. World Health Organization; 2002.
- Wichmann AB, Goltstein LCMJ, Obihara NJ, et al. QALY-time: experts' view on the use of the quality-adjusted LIFE year in COST-effectiveness analysis in palliative care. BMC Health Serv Res 2020;20:659. [Crossref] [PubMed]
- Helter TM, Coast J, Łaszewska A, et al. Capability instruments in economic evaluations of health-related interventions: a comparative review of the literature. Qual Life Res 2020;29:1433-64. [Crossref] [PubMed]
- McCaffrey N, Currow DC, Eckermann S. Measuring impacts of value to patients is crucial when evaluating palliative care. J Pain Symptom Manage 2009;37:e7-9. [Crossref] [PubMed]
- Round J. Is a QALY still a QALY at the end of life? J Health Econ 2012;31:521-7. [Crossref] [PubMed]
- Murtagh FEM, Iris Groeneveld E, Kaloki YE, et al. Capturing activity, costs, and outcomes: the challenges to be overcome for successful economic evaluation in palliative care. Prog Palliat Care 2013;21:232-5. [Crossref]
- Murtagh FE, Ramsenthaler C, Firth A, et al. A brief, patient- and proxy-reported outcome measure in advanced illness: Validity, reliability and responsiveness of the Integrated Palliative care Outcome Scale (IPOS). Palliat Med 2019;33:1045-57. [Crossref] [PubMed]
- Nwankwo H, Coast J, Hewison A, et al. A think-aloud study of the feasibility of patients with end-stage organ failure completing the ICECAP-SCM. Palliat Med 2022;36:1559-69. [Crossref] [PubMed]
- Wichmann AB, Adang EM, Stalmeier PF, et al. The use of Quality-Adjusted Life Years in cost-effectiveness analyses in palliative care: Mapping the debate through an integrative review. Palliat Med 2017;31:306-22. [Crossref] [PubMed]
- Normand C. Measuring outcomes in palliative care: limitations of QALYs and the road to PalYs. J Pain Symptom Manage 2009;38:27-31. [Crossref] [PubMed]
- Shah KK, Tsuchiya A, Wailoo AJ. Valuing health at the end of life: A review of stated preference studies in the social sciences literature. Soc Sci Med 2018;204:39-50. [Crossref] [PubMed]
- Shah KK, Tsuchiya A, Wailoo AJ. Valuing health at the end of life: a stated preference discrete choice experiment. Soc Sci Med 2015;124:48-56. [Crossref] [PubMed]
- Shield A, Oshin L, Heer S, et al. EE117 Understanding the Expected Severity Modifiers Across Diseases Following Changes to NICE Methodology. Value Health 2022;25:S76. [Crossref]
- Large S. HTA127 What Does the NICE Severity Modifier Mean in Reality? Has Cost Neutrality Restricted It Too Much? Value Health 2022;25:S321. [Crossref]
- Dzingina MD, McCrone P, Higginson IJ. Does the EQ-5D capture the concerns measured by the Palliative care Outcome Scale? Mapping the Palliative care Outcome Scale onto the EQ-5D using statistical methods. Palliat Med 2017;31:716-25. [Crossref] [PubMed]
- Myring G, Mitchell PM, Kernohan WG, et al. An analysis of the construct validity and responsiveness of the ICECAP-SCM capability wellbeing measure in a palliative care hospice setting. BMC Palliat Care 2022;21:121. [Crossref] [PubMed]
- McCaffrey N, Eckermann S. Raise the Bar, Not the Threshold Value: Meeting Patient Preferences for Palliative and End-of-Life Care. Pharmacoecon Open 2018;2:93-5. [Crossref] [PubMed]


