Editor’s note:
Prof. Blair Henry (Sunnybrook Health Sciences Center): It is my honor to be named the inaugural chair of the newly created Ethics column for the Annals of Palliative Medicine. My motto has always been: Know better—do better! Palliative care and more specifically end-of-life care are natural nexus for ethical quandaries. In this column I hope to be able to provide our readers with interesting, topical and challenging ethical issues relevant to your clinical setting.
A reasoned argument for the demise of the “do not resuscitate” order
In a recent article, published in the New England Journal of Medicine, Truog and Burns provided an important overview of the 40-year history of the do not resuscitate (DNR) order. Rarely in the history of medicine have three simple letters ‘DNR’ evoked such controversy. Indeed, this acronym has been the epicenter of numerous legal disputes, a source of great distrust in medicine, and been associated with eliciting great moral distress and strong emotions from not only health care professionals but patients and families alike (1).
To this end, I propose in this brief commentary, an argument based on five dominant categories to support my reasons to advocate for the demise of the term DNR from our medical vocabulary, and to replace it with a clearer and more precise term such as no cardiopulmonary resuscitation (No CPR). As controversial as this may seem, my intended goal is simply to recommend the demise of the “DNR” term, rather than its intended actions.
The problem with language
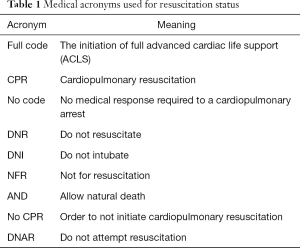
Table 1 represents a sampling of the various acronyms this writer has seen documented in patient charts over a span of ten years, indicative of the variability and confusion in clinical staff’s attempt to clarify a patient’s resuscitation status. This lack of consistent terminology has regrettably been the source of both reported near-misses and actual medical error (2). In larger academic centers, where residents move across several institutions during their medical training, the variance in terminology used can be significant.
It has been acknowledged that language choice is important. Some centers have opted for a subtle change in terminology as an attempt to make term definitions more transparent. Instead of the DNR phrase, a more appropriately worded order, Do Not Attempt Resuscitation (DNAR), is being employed. The simple addition of the word ‘attempt’ to the new order softens any implication that successful resuscitation post-cardiopulmonary resuscitation (CPR) is likely. Other institutions have replaced DNR with Allow Natural Death (AND) as this term supposedly create a more emotionally positive environment for goals of care conversations (2).
Full table
DNR impact on mortality
Surprisingly, the mortality rate for patients with and without a DNR order on their charts is significant when trying to understand the negative impact a DNR can have on both hospital outcomes and the perceived quality of care hospitalized patients receive.
Table 2 presents the results of four studies conducted on the impact of DNR orders on the mortality rate of patients admitted to hospital for a variety of causes (3-6). Understanding the limitations inherent in retrospective chart reviews, the chance of dying as a result of having a DNR order on your chart is 1.5 to 9 times greater than those without a DNR order.
A DNR order is theoretically limited only to resuscitative efforts. Nevertheless, the data suggests a DNR resuscitative status can result in differences in treatment options being presented to patients, thereby resulting in a negative effect on the overall quality of care, which may contribute to the variation noted in mortality rates between patient with and without a DNR order.
It is posited that the term “DNR” may be interpreted by some healthcare providers as meaning, do not provide additional lifesaving care. This overextension of the definition beyond the original intent of having a DNR, plainly implying that no CPR is to be attempted in the event of a cardiopulmonary arrest, may be a cause for the biased management and outcome differences noted in this review (4,6).

Full table
Fiction versus futility
A major deterrent to enabling doctors, patients and families from having a cogent conversation about DNR orders concerns the fact that CPR has been at the focal point for two very troubling influences in the history of medicine: fiction and futility.
Many clinicians will be familiar with the 1996 article in the NEJM which looked at how CPR is depicted in popular television medical dramas (d 1996). The fictional takeaway message for many people unfamiliar with acute and terminal illness was disconcerting. These programs depicted that 75% of patients were alive immediately following their arrest and upwards to 67% had what appeared to be a long term survival. It is without doubt that these statistics are considerably at odds with reality. Additionally, a majority of the patients depicted in most of the television shows were from a much younger age group and the causes of cardiac arrest were typically from more violent sources of injury, namely gunshot wounds, drownings, and motor vehicle accidents. These circumstances are neither typical nor applicable to most actual code conversations happening in a hospital setting (7).
In reality, the majority of hospital cases involve a significantly older and frail patient demographic, and many of these individuals are expected to die regardless of the provision of life-saving interventions. In these cases, clinical staff typically believes their patient will not experience any medical benefit from an attempt at resuscitation; rather, they may believe that conducting CPR will place them on the wrong side of the help-hurt line in medicine. Regrettably, the word “futility” is frequently used when trying to make families understand the wisdom in the execution of a DNR order. I say regrettably because of the controversial history the term has engendered wherein the patient/family believe that a DNR order on the chart means the clinical team is simply giving up on the patient. Many patients and families have recounted past negative experiences where they have been asked to accept a DNR order based on what they were told about a dire prognosis—only to see the patient survive that hospitalization. Statistics on quantitative or physiological futility may not be enough to dissuade some families and patients, and multiple attempts to “get the DNR’ can often lead to feeling of mistrust between the clinical team and the patient/family (8).
What does DNR mean in an acute care hospital?
The conventional approach to CPR in an acute care hospital is typically understood as the provision of advanced cardiac life support (ACLS) by a specialized “Code Team” or by staff in an emergency department or intensive care setting (ICU). ACLS guidelines are regularly updated by the American Heart Association to reflect best practice and new evidence in the field of resuscitation medicine (9).
ACLS-CPR is an organized sequential response for a pulseless apneic patient and could include any or all of the following: chest compressions, defibrillation, intubation, vasopressin, epinephrine, advanced vascular access (central line or intraosseous if peripheral access is not available), needle decompression [if pneumothorax is suspected in pulseless electrical activity (PEA)], pericardiocentesis (if tamponade is suspected in PEA) or medications that may have significant adverse effects (such as tPA for possible pulmonary embolism in PEA), in addition to transfer to an ICU setting for ongoing treatment (9).
In conducting quality review audits of CPR/DNR documentations, it is frequently noted that in many cases additional disconcerting instructions have typically been added to patient charts who were otherwise designated as being ‘full code’ (full code but no intubation, chest compressions, only no shock, etc.). Ongoing education and training is required to help staff understand that a refusal of any component of the ACLS protocol is effectively equal to a DNR.
CPR is not intubation for respiratory failure, the use of pressor for hemodynamic instability, the use of a pacemaker for third-degree heart block, or for the administration of adenosine for supraventricular tachycardia (SVT). In effect, a DNR on a patient’s chart could still mean intubation for respiratory failure, cardioversion in the case of unstable atrial fibrillation and transfer to an ICU setting for known and treatment medical emergencies. Each of these interventions would be appropriate treatments when goals of care have been clearly communicated and documented.
Consent
Consent requirements for resuscitation, either for its initiation or its withholding, are confusing. For cardiac arrests outside the hospital, the provision of CPR remains a public good, in that when a person is found without pulse and breath, a stranger is expected to initiate CPR, without consent. This societal norm is based on the high value given to life and its preservation (10).
In hospitals, however, the possibility exists that a patient’s medical status and prognosis may call to question the utility of suggesting a resuscitation attempt. Additionally, some patients, approaching the end of life, who may not want invasive attempts to prolong their life may ask or consent to a DNR as an expression of their autonomy. DNR orders are typically present in approximately 18–28% of hospitalized patients, a proportion that is generally increased in the elderly and in those with severe disease (10,11).
The inherent conflict between the patients’ autonomous right to accept or refuse any medical treatment, being interpreted by some as a right to demand medical treatments, and the right of a physician to withhold treatment perceived to present no medical benefit for the patient has resulted in end-of-life conflicts requiring judicial intervention (12). As a result of complaints lodged to the College of Physician and Surgeons of Ontario, around the perception that “unilateral” DNR orders were being use, a revision to their end-of-life policies has stated that patients or family must consent to the placement of a “No CPR” order on the chart. Without this expressed consent, CPR must be provided by the health care team (13).
An alternative approach
Managing effective conversations related to “code status” requires excellent communication skills and a clinically appropriate context. Though not considered exhaustive, our institution has instigated the following five primary steps:
- As counter-cultural as it sounds, our institution is working towards making the term “DNR” obsolete and replacing it with the term: “No CPR”. The belief is that “No CPR” is a more unambiguous and easily defined instruction to all clinical staff;
- To avoid confusion of what CPR does or does not include, a standard order set has been created to outline that a patient does not want CPR in the event of being found pulseless and apneic. The expectation would be that a patient found pulseless and apneic with a documented No CPR order would not receive any of the interventions outlined in the ACLS protocol. Conversely, a patient found pulseless and apneic without a No CPR order would be subject to all interventions (as clinically required) outlined in the ACLS protocol. No partial codes will be accepted;
- Orders for No CPR (previously DNR) cannot be hand written in our institution. The pre-printed order sheet must be used and if a hand written note is identified it is flagged as an identifiable near-miss in our patient safety system;
- All staff are trained and made aware of the appropriate “escalation of care” requirements for all ward patients. The No CPR status has been uncoupled from the idea that a patient should not receive all manner of life supportive therapies up to CPR. To stipulate this point, it would be suitable to have our ICU filled with patients who had a No CPR order if the appropriate goals of care were documented and outlined the use of life supportive treatments, as appropriate, for potentially reversible causes;
- Special tabs have been added to our electronic patient charts to identify and clearly document conversations and meetings related to both “Goals of Care” and “Advance Directives”. In an ideal situation, where a patient clearly understands their current health status (diagnosis, treatment options and prognosis), and that an honest conversation is attended to with regard to the expected goals of care during the present hospitalization, discussions related to code status can be a natural outcome as opposed to a specific and stressful agenda item for a family meeting. Goals of care should come before plans of care (14).
Conclusions
My argument for the proposed demise of the term DNR centered on the following concerns: problems with language; the negative impact DNR can have on mortality; the disconnect between reality and fiction on effectiveness of CPR based on incorrect media portrayals; a lack of a common understanding what DNR actually means in many health care settings and finally the problem of consent.
As a potential remedy, I proposed an alternative approach for consideration—one my hospital is striving towards. However, the question ultimately is: will simply using the term No CPR (in lieu of DNR) fix or redress any of these problems?
I would suggest that it does. Language is unquestionably a problem and any attempt at standardization across institutions and the provision a clear definition will help. As for the matter of how using No CPR might impact mortality—this is a more challenging point to defend. However, my contention is that using all past date representing the impact of DNR is suspect due to a lack of a consistent understanding on what that term translated to in the clinical care setting. Empirical data supports a negative impact on survival for equal status patients based simply on the fact that DNR was on their chart. I will concede that by simply using the term No CPR going forward it would be impossible to prove its overall impact mortality. However, I believe that any negative impact the previous term DNR might have had on clinicians actually proposing or suggesting aggressive and life-saving treatments will at the very least be eliminated by this change. No CPR means just that and nothing else. All other medical decisions need to be discussed and put into the plan of care. The problem related to a disconnect between actual versus perceived outcomes of CPR will not be directly addressed by a change of language alone—but I will go on the record to say that the use of the term DNR has enormous negative connotations for patients and families. If my family member could be resuscitated (as the language implies), why wouldn’t we opt for that? Some have suggested DNR be changed to DNAR where the word attempt is added to make the outcome more realistic. No CPR language takes the outcome of the act out of the equation—it changes the word resuscitation from a verb to a noun and forces us to talk more about the procedure being proposed. Semantics matter! I would also suggest that the lack of a common understanding of what DNR means in most hospitals should be cleared by replacing it with No CPR—which has a very concrete meaning. As for consent, the issue of using the term No CPR will not impact the clinical team’s requirements—but I would suggest that using No CPR will enhance the “informed” component of consent more so than DNR.
I leave it to the readers to determine if I’ve presented a strong and convincing argument. DNR is part of the culture of health care and its eradication—if that is our goal—will be hard to achieve! More importantly I believe that the basis of good ethics continues to rely on good facts. Ultimately, decisions regarding CPR should not be about making a value judgment about someone’s life. It should instead be a carefully structured conversation between all stakeholders over choices that consider the best empirical evidence and a patient’s wishes and values. These ethically fragile conversations frequently happen during emotionally laden times, and as a result, are completed hastily—I support that any measure that improves clarity and understanding of what is being communicated to all parties can only help.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Burns JP, Truog RD. The DNR Order after 40 Years. N Engl J Med 2016;375:504-6. [Crossref] [PubMed]
- Breault JL. DNR, DNAR, or AND? Is Language Important? Ochsner J 2011;11:302-6. [PubMed]
- McAlister FA, Wang J, Donovan L, et al. Influence of Patient Goals of Care on Performance Measures in Patients Hospitalized for Heart Failure: An Analysis of the Enhanced Feedback For Effective Cardiac Treatment (EFFECT) Registry. Circ Heart Fail 2015;8:481-8. [Crossref] [PubMed]
- Powell ES, Sauser K, Cheema N, et al. Severe sepsis in do-not-resuscitate patients: intervention and mortality rates. J Emerg Med 2013;44:742-9. [Crossref] [PubMed]
- Richardson DK, Zive D, Daya M, et al. The impact of early do not resuscitate (DNR) orders on patient care and outcomes following resuscitation from out of hospital cardiac arrest. Resuscitation 2013;84:483-7. [Crossref] [PubMed]
- Chen JL, Sosnov J, Lessard D, et al. Impact of do-not-resuscitation orders on quality of care performance measures in patients hospitalized with acute heart failure. Am Heart J 2008;156:78-84. [Crossref] [PubMed]
- Diem SJ, Lantos JD, Tulsky JA. Cardiopulmonary resuscitation on television. Miracles and misinformation. N Engl J Med 1996;334:1578-82. [Crossref] [PubMed]
- Schneiderman LJ. Defining Medical Futility and Improving Medical Care. J Bioeth Inq 2011;8:123-131. [Crossref] [PubMed]
- 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 7.2: Management of Cardiac Arrest. Circulation 2005;112:IV-58-IV-66.
- Burns JP, Edwards J, Johnson J, et al. Do-not-resuscitate order after 25 years. Crit Care Med 2003;31:1543-50. [Crossref] [PubMed]
- de Decker L, Annweiler C, Launay C, et al. Do not resuscitate orders and aging: impact of multimorbidity on the decision-making process. J Nutr Health Aging 2014;18:330-5. [Crossref] [PubMed]
- Cotler MP. The "do not resuscitate" order; clinical and ethical rationale and implications. Med Law 2000;19:623-33. [PubMed]
- Hawryluck L, Oczkowski SJ, Handelman M. "Must do CPR??": strategies to cope with the new College of Physicians and Surgeons of Ontario policy on end-of-life care. Can J Anaesth 2016;63:973-80. [Crossref] [PubMed]
- Kaldjian LC, Erekson ZD, Haberle TH, et al. Code status discussions and goals of care among hospitalised adults. J Med Ethics 2009;35:338-42. [Crossref] [PubMed]


