The power of integration: radiotherapy and global palliative care
Low- and middle-income countries (LMICs) have the fastest growing rates of new cancer cases, but their populations have the least access to essential cancer treatments (1) and to palliative care (2). The relative lack of access to radiotherapy (RT) in these regions contributes to poorer outcomes and unnecessary suffering. RT has been shown to prevent disease progression and to be an effective tool for controlling symptoms, including pain, dyspnea, dysphagia, paralysis, and seizures in this population (3).
The lack of RT in LMICs is due to multiple factors including outdated assumptions that it is not economically feasible. Recent work by the Global Task Force on Radiotherapy for Cancer Control helps to dispel many myths about the cost and operability of RT, and to quantify the economic cost of failing to make RT available (4). In this paper, we argue that RT should be included in the global palliative care agenda, which the Lancet Commission on Global Access to Palliative Care and Pain Control has recommended be integrated into the global health agenda (5).
Scope of the problem
The need for palliative care has increased steadily with the rising global incidence and prevalence of chronic diseases, such as cancer (5). However, of the approximately 29 million people who died from diseases requiring palliation in 2011, the World Health Organization (WHO) estimates that nearly 70% did not have access to palliative care near the end of life (6). The International Agency for Research on Cancer (IARC) GLOBOCAN project estimated that, by 2025, there will be almost twice as many cancer deaths in LMICs as high-income countries (HICs) (7). Palliative care services are being implemented throughout the world, but most LMICs still lack comprehensive palliative care policies, plans, and consistent access to pain medications (2). Patients needing palliative care in HICs consume approximately 500 times more morphine than patients living in the poorest 10% of countries (5). This inequity parallels the global divide in access to RT.
RT has been categorized by the WHO as a life-prolonging treatment (6). However, this overlooks its benefit in symptom control, in that it specifically distinguishes RT from palliative care (8). This separation of RT from palliative care is consistent with the overall exclusion of RT from the global palliative care agenda and from health systems planning (4).
The application of RT in palliation
Palliative RT is defined as treatment that is delivered to relieve symptoms of cancer and therefore improve quality of life (3). It is intended to allow for rapid and durable symptom relief with minimal side effects. In HICs, palliative RT constitutes 30−50% of the workload in RT departments (9,10). This number would be even greater in LMICs, if radiation facilities were available there, since cancer patients in LMICs tend to present at a more advanced stage of disease in these regions (2,11).
In many instances, palliative RT can be delivered in a timely and cost effective manner. Clinical scenarios of pain due to bone and visceral metastases, advanced primary tumors, or neurologic deficits related to cancer are frequent indications for palliative RT (12). RT can also be helpful in controlling bleeding due to primary or metastatic disease and in relieving obstructive symptoms such as those in the respiratory, gastrointestinal and urinary tracts. See Table 1 for a more extensive list of indications for palliative RT (12).
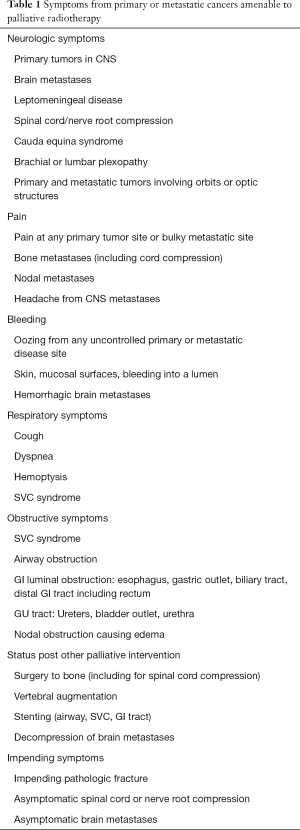
Full table
The management of bone metastases with RT illustrates the potential efficacy and efficiency of this treatment. A systematic review of studies of RT for the treatment of painful bony metastases demonstrated that a complete response can be achieved in approximately 25% of cases and a partial response in more than 60% with single-fraction radiotherapy (SFRT) or multi-fraction radiotherapy (MFRT) (13). The rate of retreatment is greater with SFRT than with MFRT (20% vs. 8%), but the outcomes in terms of long-term pain control, subsequent spinal cord compression, or pathologic fracture are not different (13,14). In addition, 45−61% of patients obtain additional benefit from re-irradiation of bone metastasis (15).
When the treatment goal in metastatic cancer is to achieve local tumour control, a higher dose of radiation may be delivered. For example, a higher dose for spine metastases with epidural extension may improve local control and prevent spinal cord compression (3). Similarly, a systematic review of palliative RT to the lung has shown that a biologically equivalent dose of 30 Gy in 10 fractions or higher has a modest improvement in survival when compared to shorter dose-fractionation schemes, although symptomatic improvement was equivalent with short and long course radiation (16).
Barriers to integration of RT into global palliative care
Although LMICs are home to 85% of the world’s population, only one-third of all RT facilities worldwide are located in these areas, reflecting an enormous global disparity in the distribution of RT resources. A 2014 publication of the International Atomic Energy Agency (IAEA) Directory of Radiotherapy Centres (DIRAC) indicated that only 4 of 139 LMICs had the recommended number of teletherapy units and that 55 (39.5%) had no access at all (17). Since RT requires specialized resources, it is frequently the last cancer service to be considered for implementation. In that regard, neither the Butaro Cancer Centre in Rwanda nor the Moi University Cancer Centre in Eldoret, Kenya yet have RT capacity (4). In cancer treatment centers in LMICs that are equipped with RT, the machines have been found to be either outdated or insufficient in capacity (17).
The effective integration of RT into palliative care programs in LMICs requires a multifaceted approach in order to overcome systemic barriers. These barriers include financial and other resource constraints, inadequate health insurance coverage and poverty, the burden of travel and accommodation for patients, weak health systems, and the lack of an infrastructure to support RT. The last includes both physical and human infrastructure, which is dependent on access to training programs, several years of educational investment, and secure employment opportunities for trainees following graduation (4). A summary of these barriers, as well as practical solutions to address them, is presented in Table 2.

Full table
Radiation and palliative care are not integrated adequately in HICs and LMICs. In LMICs, this should include integration of community healthcare workers, and traditional healers, who are often an important component of palliative and end-of-life care (18,19). Linking these healthcare providers to the formal medical system might help to ensure earlier access to interventions such as RT. Indeed, the integration of RT into both the formal and informal systems of health care may be essential to ensure its access and perceived acceptability and to diminish unnecessary suffering and expense at the end of life for many individuals in LMICs.
Palliative RT services are now being developed in many HICs, but radiation is still often not part of the overall treatment plan. Palliative care practitioners who are well versed in pain and symptom management may not appreciate RT as palliative tool (3,20). In HICs, the separation of the fields of RT and palliative care may be linked to the history of modern palliative care, which emerged in reaction to the overreliance on technology in medical care, especially near the end of life (21). In LMICs, this separation of RT and palliative care may simply reflect the dearth of health workforce in each area, particularly outside of larger urban centres (22).
The emergence and integration of palliative care and RT in LMICs: case studies of India and Kenya
Case studies on India and Kenya illustrate issues related to the integration of RT and palliative care in LMICs. These countries were selected based on the research and clinical experience of the authors, and because they illustrate contrasting and common issues related to the development and integration of RT and palliative care.
Kenya and India both have steep health-related inequities due to economic disparities and dual health systems within these countries. Both have private systems of health care for patients who can pay out of pocket for quality medical care and a second, public system for those who lack these resources. Neither country has yet adopted a plan for universal health coverage or universal health insurance, making cancer treatments difficult to afford for the majority of those with the disease. Nevertheless, evidence is accumulating to suggest that RT is a cost-effective treatment option in these countries (4).
Palliative care in public and private sectors in India
India has a total population of 1.2 billion and it has been estimated that there are 6 million people in need of palliative care annually (23). GLOBOCAN projections indicate that India’s cancer burden is expected to almost double over the next 20 years, with a projected increase in cancer deaths from 680,000 in 2012 to 1.2 million by 2035 (24). There is no comprehensive national registry, but the National Cancer Registry Programme, which includes 28 population-based and 7 hospital-based cancer registries from across the country, indicates that up to 80% of patients present to cancer centres at an advanced stage of disease (23).
A recent report from the Atomic Energy Regulatory Board of India indicates that there are currently 380 radiation centers in India with a total of 560 teletherapy machines [237 cobalt and 323 linear accelerators (linacs)] and 296 brachytherapy units (25). However, these centres are clustered in larger centers; a study of locally advanced cervical cancer patients in rural India found that over 60% were required to travel over 100 km to receive treatment (26). At All India Institute of Medical Sciences, a large public hospital in the National Capital Region (NCR), 3,167 patients received RT in 2014, of which 915 were with palliative intent. At Fortis Hospital, Gurgaon, a tertiary care private hospital located in the NCR, a review of institutional records indicates that 600 RT patients were treated in 2014 and that treatment was palliative in about 25%.
Although the first palliative care centres were established in India in the late 1980s and early 1990s (27), restrictive regulations and the lack of prioritization of palliative care within the health care sector have meant that a very small segment of cancer patients receive adequate services (28). Financial disincentives to palliative care services have also hindered the delivery of palliative RT in India. Palliative RT is less remunerative than other treatments and therefore many private or corporate hospitals in India have not established structured palliative care clinics. Within the public sector, health care resources are strained and palliative care is often not prioritized. As a result, non-governmental organizations (NGOs), such as CanSupport in Delhi, have attempted to fill this gap. This NGO provides home-based palliative care to patients free of cost, delivering narcotics and providing social support, and also links patients to radiation therapy at the public hospital as needed (29).
A public private partnership for palliative RT in Kenya: the MP Shah Hospital in Nairobi, Kenya
Kenya has a population of 45 million, 10% of whom reside in its capital city Nairobi. Palliative care services in this country vary by region, but access to adequate supplies of pain medications and other palliative care outside of urban hospital settings remains limited (6,22). Kenya’s Ministry of Health has announced plans to increase the availability of morphine and to expand palliative care services to all 47 counties nationally (22,30).
Based on a site review by the authors, as well as on published data (31), Kenya presently has nine external beam machines, six linacs and three tele-cobalt machines, although these numbers fluctuate depending on new purchases and decommissioning of equipment. This resource falls far short of the 40 machines recommended by the IAEA, based on Kenya’s cancer burden, but it is among only 25 countries in Africa with any in-country RT capacity (31).
The RT facilities in Kenya are unevenly distributed, with nearly 70% (n=6) located in Nairobi. Kenyatta National Hospital (KNH) in Nairobi currently has two cobalt machines and represents the only formal public sector RT in that city. There are plans to add linac capacity, which is urgently needed, since the current waiting time for treatment is at least one year. Further, both treatment machines at KNH were not functioning in early 2015, prompting intense discussion about how to increase RT availability for the majority of Kenyan patients (32). Private radiation facilities, including those at Nairobi Hospital, Aga Khan University Hospital and MP Shah Hospital, are unaffordable for most patients, although there is some consideration by the Ministry of Health to subsidize treatment for public sector patients at these centres (33).
Cancer Care Kenya, located at the MP Shah Hospital, a private sector dedicated oncology facility that opened in 2010, has accepted some public sector patients from KNH. Seventy patients are treated each day at Cancer Care Kenya on two linacs, of which 35–40% are expressly for palliation, and up to 60% are receiving concurrent chemotherapy. There is 1 radiation oncologist, 8 radiation therapists, 1 dosimetrist, and 1 medical physicist, all of whom were trained outside Kenya. Brachytherapy is not yet available, but implementation is planned. The cost per treatment for patients is 10,000 Kenyan shillings per treatment (95 USD) and 10% of patients receive full financial support. Other palliative services, including pain and symptom management, are also available at Cancer Care Kenya, which partners with three religiously affiliated free care hospitals outside the capital to expand the reach of RT to rural patients. In comparison to many other LMICs, Kenya and India have enhanced resources both in palliative care and RT, though the latter exist largely in the private sector. Formalizing and expanding public-private partnerships is a potential mechanism to advance the availability of palliative and curative RT in these countries and in their broader surrounding regions (34,35).
Integrating global policy and advocacy efforts
Over the last several years, the need to address cancer care and pain management and palliative care in LMICs has received increasing attention within the global health community (5). Although many LMICs are improving the availability of palliative care, only a few are methodically including RT as a palliative intervention. To address this gap, partnerships among global institutions, cancer leaders, professionals, industry and civil society around the world have emerged to advocate for better access to RT in cancer care and control.
A resolution at the 67th World Health Assembly in 2014 requested that its member states develop, strengthen and implement evidence-based and cost-effective palliative care policies (36). While the resolution did not specifically mention RT, it did provide an opportunity for RT to become part of the global discourse on palliative care. In that same year, the Worldwide Palliative Care Alliance, in collaboration with the WHO, published the Global Atlas of Palliative Care at the End of Life (6). The Atlas highlighted the need for new pain management guidelines and for a strategy to integrate palliative care in health systems across disease groups and levels of care. Following these initiatives and, in response to the large global inequalities in access to pain control and palliative care, the Lancet Commission on Global Access to Pain Control and Palliative Care, led by Felicia Knaul, was launched in early 2015 (5). The objectives of the Commission include the development and application of a comprehensive framework for palliative care embedded within universal health coverage. The work of the Commission offers an opportunity for RT to be included as part of effective coverage of palliative care in different resource settings.
Many LMICs have begun to incorporate palliative care into their National Cancer Control Plans or Programmes (NCCP). For instance, 16 countries in Latin America now have a national cancer plan or programme, 13 of which include palliative care. Chile, Colombia, Mexico and Panama have national palliative care laws as well (37). The NCCP in Bangladesh explicitly mentions the utility of RT for palliative care, recommending that all oncology/RT departments should have a pain relief and palliative care programme (38). In Africa, the NCCP of Ghana includes palliative RT as a supportive intervention in the course of illness and includes RT technicians in the core team for palliative care in tertiary care or specialized settings where RT is named as a palliative procedure (39).
Several promising global initiatives have recently been undertaken to develop an evidence base for increased RT capacity building. The Global Task Force on Radiotherapy for Cancer Control of the Union for International Cancer Control (40) identified opportunities and quantified the investment needed to ensure equity in global access to radiation therapy (4). Its work is linked to other global institutions such as the IAEA, a UN agency with the mandate to support UN Member States to support RT capacity as part of their national cancer control plans (41). In 2004, the IAEA established the Programme of Action for Cancer Therapy to provide technical support to individual countries in technology purchase for radiation and for its inclusion in cancer plan execution. They have also assisted with education in radiation oncology through the African Regional Cooperative Agreement (AFRA), which supports select African centres to develop as training and education hubs in this field.
Another approach that has helped to enhance expertise in palliative RT in LMICs is the establishment of ‘twinning programmes’. These programmes are international partnerships between RT centres in HICs and LMICs that have effectively facilitated the transfer of expertise, skills and knowledge to improve the delivery of safe RT in LMICs (42,43). Such collaborations have been mutually beneficial. In LMICS, they have facilitated the development and implementation of locally appropriate treatment protocols, health professional training, data management, and manpower and equipment support. For HIC partners, they provide opportunities to improve basic clinical skills for trainees and staff, research opportunities, cultural competency training, and improved knowledge of global health issues (43). Many twinning programmes began in the area of childhood cancer management, and were fostered by the IAEA through the Paediatric Radiation Oncology Network, which involves 14 centres in 13 LMICs from Africa, Asia and Latin America (42). This twinning model has also been applied in volunteer-run non-for-profit organizations such as Medical Physicists Without Borders (44) and the International Cancer Expert Corps (45), which are working to provide technological and human resource support for global health initiatives within radiation oncology.
Conclusions
There has been considerable recent attention to the global need for palliative care. Access to pain relief and to end-of-life care has been declared a basic human right and there has been substantial advocacy and progress to increase its availability over the past several decades. There is a similar need to increase the availability of RT. Both curative and palliative RT have been undervalued, and palliation has been especially ignored in the global health discourse.
Only recently has there been synergy between global policy and advocacy movements focused on palliative care and RT, as well as more widespread appreciation of the effectiveness of RT as a palliative intervention. The linkage of these movements will be of benefit to LMICs, where neither RT nor palliative care is widely available. Global initiatives to advance both RT and palliative care should be conducted together and connected with national structures and actors in LMICs to ensure that they are universally and equitably available and integrated into health systems.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Farmer P, Frenk J, Knaul FM, et al. Expansion of cancer care and control in countries of low and middle income: a call to action. Lancet 2010;376:1186-93. [Crossref] [PubMed]
- Hannon B, Zimmermann C, Knaul FM, et al. Provision of palliative care in low- and middle-income countries: overcoming obstacles for effective treatment delivery. J Clin Oncol 2016;34:62-8. [Crossref] [PubMed]
- Lutz ST, Jones J, Chow E. Role of radiation therapy in palliative care of the patient with cancer. J Clin Oncol 2014;32:2913-9. [Crossref] [PubMed]
- Atun R, Jaffray DA, Barton MB, et al. Expanding global access to radiotherapy. Lancet Oncol 2015;16:1153-86. [Crossref] [PubMed]
- Knaul FM, Farmer PE, Bhadelia A, et al. Closing the divide: the Harvard Global Equity Initiative-Lancet Commission on global access to pain control and palliative care. Lancet 2015;386:722-4. [Crossref] [PubMed]
- Global Atlas of palliative care at the end of life. Available online: http://www.who.int/nmh/Global_Atlas_of_Palliative_Care.pdf
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917. [Crossref] [PubMed]
- WHO definition of palliative care. Available online: http://www.who.int/cancer/palliative/definition/en/
- Stevens G, Firth I. Clinical audit in radiation oncology: results from one centre. Australas Radiol 1996;40:47-54. [Crossref] [PubMed]
- Williams MV, James ND, Summers ET, et al. National survey of radiotherapy fractionation practice in 2003. Clin Oncol (R Coll Radiol) 2006;18:3-14. [Crossref] [PubMed]
- Barton MB, Frommer M, Shafiq J. Role of radiotherapy in cancer control in low-income and middle-income countries. Lancet Oncol 2006;7:584-95. [Crossref] [PubMed]
- Jones JA, Lutz ST, Chow E, et al. Palliative radiotherapy at the end of life: a critical review. CA Cancer J Clin 2014;64:296-310. [Crossref] [PubMed]
- Chow E, Zeng L, Salvo N, et al. Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 2012;24:112-24. [Crossref] [PubMed]
- Lutz S, Berk L, Chang E, et al. Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J Radiat Oncol Biol Phys 2011;79:965-76. [Crossref] [PubMed]
- Chow E, van der Linden YM, Roos D, et al. Single versus multiple fractions of repeat radiation for painful bone metastases: a randomised, controlled, non-inferiority trial. Lancet Oncol 2014;15:164-71. [Crossref] [PubMed]
- Fairchild A, Harris K, Barnes E, et al. Palliative thoracic radiotherapy for lung cancer: a systematic review. J Clin Oncol 2008;26:4001-11. [Crossref] [PubMed]
- Datta NR, Samiei M, Bodis S. Radiation therapy infrastructure and human resources in low- and middle-income countries: present status and projections for 2020. Int J Radiat Oncol Biol Phys 2014;89:448-57. [Crossref] [PubMed]
- Campbell LM, Amin NN. A qualitative study: potential benefits and challenges of traditional healers in providing aspects of palliative care in rural South Africa. Rural Remote Health 2014;14:2378. [PubMed]
- Merriam S, Muhamad M. Roles traditional healers play in cancer treatment in Malaysia: implications for health promotion and education. Asian Pac J Cancer Prev 2013;14:3593-601. [Crossref] [PubMed]
- Jones JA, Simone CB 2nd. Palliative radiotherapy for advanced malignancies in a changing oncologic landscape: guiding principles and practice implementation. Ann Palliat Med 2014;3:192-202. [PubMed]
- Clark D. From margins to centre: a review of the history of palliative care in cancer. Lancet Oncol 2007;8:430-8. [Crossref] [PubMed]
- Bosnjak S, Maurer MA, Ryan KM, et al. Improving the availability and accessibility of opioids for the treatment of pain: the International Pain Policy Fellowship. Support Care Cancer 2011;19:1239-47. [Crossref] [PubMed]
- Khosla D, Patel FD, Sharma SC. Palliative care in India: current progress and future needs. Indian J Palliat Care 2012;18:149-54. [Crossref] [PubMed]
- Mallath MK, Taylor DG, Badwe RA, et al. The growing burden of cancer in India: epidemiology and social context. Lancet Oncol 2014;15:e205-12. [Crossref] [PubMed]
- National Symposium on "Physics, Clinical, and Radiobiological aspects of hypofractionation in current radiotherapy practice; 2015; Hyderabad, India.
- Dutta S, Biswas N, Muhkherjee G. Evaluation of socio-demographic factors for non-compliance to treatment in locally advanced cases of cancer cervix in a rural medical college hospital in india. Indian J Palliat Care 2013;19:158-65. [Crossref] [PubMed]
- Mohanti BK. Research focus in palliative care. Indian J Palliat Care 2011;17:S8-11. [Crossref] [PubMed]
- Rajagopal MR, Joranson DE, Gilson AM. Medical use, misuse, and diversion of opioids in India. Lancet 2001;358:139-43. [Crossref] [PubMed]
- CanSupport: Caring for people with cancer. Available online: http://www.cansupport.org/newcansupport/
- O'Brien M, Mwangi-Powell F, Adewole IF, et al. Improving access to analgesic drugs for patients with cancer in sub-Saharan Africa. Lancet Oncol 2013;14:e176-82. [Crossref] [PubMed]
- Abdel-Wahab M, Bourque JM, Pynda Y, et al. Status of radiotherapy resources in Africa: an International Atomic Energy Agency analysis. Lancet Oncol 2013;14:e168-75. [Crossref] [PubMed]
- Reporter N. Hundreds of lives at risk as Kenyatta National Hospital cancer machines collapse. Daily Nation: 2015.
- Ndonga S. Aga Khan Hospital steps in to ease KNH cancer care crisis. Capital News; 2015. Available online: http://www.capitalfm.co.ke/news/2015/03/aga-khan-hospital-steps-in-to-ease-knh-cancer-care-crisis/
- Ngwa W, Ngoma T, Zietman A, et al. Closing the cancer divide through ubuntu: information and communication technology-powered models for global radiation oncology. Int J Radiat Oncol Biol Phys 2016;94:440-9. [Crossref] [PubMed]
- Expanding radiotherapy services in Kenya. Available online: https://www.iaea.org/technicalcooperation/documents/Success-Stories/2013/KEN6019.pdf
- Strengthening of palliative care as a component of comprehensive care throughout the life course. Available online: http://apps.who.int/gb/ebwha/pdf_files/EB134/B134_28-en.pdf
- Pastrana T, De Lima L, Wenk R, et al. Atlas of Palliative Care in Latin America ALCP. 1st Edition. Houston: IAHPC Press; 2012.
- Anisur Rahman S, Mostafa Zaman M, Akram Hussain SM, editors. National cancer control strategy and plan of action 2009-2015. Bangladesh: Directorate General of Health Services, Ministry of Health and Family Welfare, 2008.
- National strategy for cancer control in Ghana: 2012-2016. Ghana: Ministry of Health, 2011.
- Jaffray DA, Knaul FM, Atun R, et al. Global Task Force on Radiotherapy for Cancer Control. Lancet Oncol 2015;16:1144-6. [Crossref] [PubMed]
- Rosenblatt E, Zubizarreta E, Wondergem J, et al. The International Atomic Energy Agency (IAEA): an active role in the global fight against cancer. Radiother Oncol 2012;104:269-71. [Crossref] [PubMed]
- Salminen E, Anacak Y, Laskar S, et al. Twinning partnerships through International Atomic Energy Agency (IAEA) to improve radiotherapy in common paediatric cancers in low- and mid-income countries. Radiother Oncol 2009;93:368-71. [Crossref] [PubMed]
- Hopkins J, Burns E, Eden T. International twinning partnerships: An effective method of improving diagnosis, treatment and care for children with cancer in low-middle income countries. J Cancer Policy 2013;1:e8-19. [Crossref]
- Medical Physicists without Borders. Available online: http://www.mpwb.org/
- Coleman CN, Formenti SC, Williams TR, et al. The international cancer expert corps: a unique approach for sustainable cancer care in low and lower-middle income countries. Front Oncol 2014;4:333. [Crossref] [PubMed]


