Community-based participatory research: understanding a promising approach to addressing knowledge gaps in palliative care
Over the past several decades, increased attention has been paid to the need for effective and accessible healthcare, especially for individuals suffering from advanced illness (1). As a holistic and interdisciplinary approach to treatment, palliative care combines the perspectives of front-line clinicians and other providers with those of patients and their families to deliver comprehensive treatment and care (2,3).
Although palliative care has been recognized as a promising approach to addressing the needs and priorities of individuals with advanced illness (4,5), significant knowledge gaps remain (6,7). Recent systematic reviews (7,8) consensus reports (3,6), and policy statements (4) continue to advocate for increasing the current knowledge base and recommend rigorous, evidence-based efforts to promote effective translation of research evidence into practice.
Especially critical is the need to align research efforts with the priorities of key stakeholder groups; namely patients, their family members, and interdisciplinary teams of healthcare providers who deliver palliative care (6). Systematic engagement of these groups can lead to tailored and appropriate care for underserved and vulnerable patient populations and their families (9) as well as culturally-sensitive interventions (10).
To address the call for targeted and systematic inquiry, we propose community-based participatory research (CBPR) as one promising strategy. In this paper, we first define what CBPR is, and present a rationale for its applicability to palliative care research. We then describe how CBPR could address specific gaps in the field, highlight several examples where this approach has been used in palliative care, and finally outline barriers to applying CBPR in this field.
What is community-based participatory research?
Across the fields of medicine, social science and public health, a number of partnership approaches to research have been described. Although the term “CBPR” has been used interchangeably with “community-centered”, “community-involved”, “participatory”, or “collaborative” research, a fundamental characteristic of CBPR is the intentional engagement of community members in sharing their unique perspectives and local knowledge (11). More specifically, CBPR is distinguished from other approaches that conduct research in community settings, but do not actively involve community members in all phases of the research process (11).
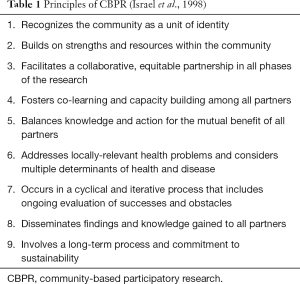
CBPR is defined by nine key principles (11) (Table 1). At its core, CBPR is a collaborative approach to research that seeks to address a locally-relevant health issue. This methodology intentionally and equitably engages researchers and community members in all aspects of the research process, including decision-making, capacity building, knowledge generation, and dissemination of findings. CBPR projects begin by defining a “community of concern,” which may consist of individuals within a given geographic region or individuals with a shared identity (e.g., ethnic group, health concern). CBPR is a cyclical and iterative process; one that is designed to promote long-term commitment by researchers and community members alike (11). Ultimately, the goal of this research strategy is to integrate new knowledge and understanding with community change efforts for the mutual benefit of all partners (11). As such, CBPR offers practical and sustainable solutions that are intended to improve the health and well-being of the involved communities.
Full table
The literature has pointed to a number of advantages that can accrue from using a CBPR approach (12). These benefits include: (I) ensuring that the research topic reflects a major issue identified by community; (II) improving the quality, validity and sensitivity of the research by drawing upon community wisdom; (III) promoting trust between communities and researchers; (IV) improving the translation of research findings into policy and practice; and (V) enhancing uptake of the research findings by community members.
Specific benefits of using CBPR approaches in palliative care research
In the following section, we describe the ways in which CBPR can be employed to address several challenges that occur routinely when conducting research in populations receiving palliative care. Specifically, we highlight how CBPR could help to facilitate recruitment and retention of study participants, enhance measurement quality, and improve intervention research, while empowering patients and their family members to make their voices heard (Table 2).

Full table
Facilitating recruitment and retention
Palliative care research has suffered from small, unrepresentative samples (13), with the majority of studies enrolling non-Hispanic white participants (14). Importantly, CBPR is an effective tool for recruiting vulnerable and hard to reach populations (15,16) including ethnic minorities (17).
A number of studies point to the important role community partners and liaisons play in improving recruitment and retention (17). For instance, research with veterans has engaged community-based liaisons to successfully reach and involve ethnic minorities in focus groups (18). Similar findings have been demonstrated among older adults. In research debriefings, older community members involved in a CBPR initiative attributed its high response rate to local volunteerism, further proposing that older people may be more receptive to local residents than to academic researchers (19).
In addition to improving subject recruitment, CBPR also promotes long-term commitment by inviting community members to select a topic that is relevant to their needs (11,18). Joint ownership over the research project leads to lasting investment by community members, and ultimately, lower attrition rates (20). For example, older adults involved in a CBPR initiative aimed at improving elder services emphasized that their desire to bring tangible benefits to their community was critical in keeping them actively involved in the research project (19).
Enhancing measurement quality
The palliative care literature has also lamented the field’s continued reliance on generic and inappropriate assessment tools (7). Notably, CBPR has been cited as an advantageous approach in developing tailored assessment tools for specific populations (20,21). Indeed, clinical trials incorporating community involvement have demonstrated pronounced benefits in terms of measurement quality of health care delivery (17).
Further, research with advanced cancer patients has successfully employed a collaborative approach to questionnaire development, where nurses assisted in constructing a valid questionnaire that would also minimize patient burden (15). Incorporating patient input has been shown to improve participants’ acceptance of assessment tools (20) and could be used with palliative care patients and their families who may share concerns about time burdens and fatigue.
Improving intervention effectiveness
CBPR has demonstrated promise in enhancing interventions by drawing upon local wisdom to develop and adapt interventions to the community’s unique needs and priorities. For example, in a study of stroke-related social services, stroke survivors, caregivers, and health professionals played a meaningful role in formulating service development plans, “information packs” for navigating stroke care, as well as a rehabilitation program that directly addressed the survivor-identified need for social integration (22). Clinical trials also acknowledge the benefits of patient involvement (17), noting that CBPR ensures that the trial is relevant to the lives of afflicted individuals (23). This approach could be readily employed with palliative care populations to promote greater alignment between intervention programs and palliative care patient priorities.
Integrating the perspectives of key stakeholders facilitates uptake of the intervention by community members, and enhances methodological rigor through encouraging community feedback and bi-directional dialogue about the procedural aspects of the initiative (15). Overall, CBPR’s emphasis on community engagement enhances the external validity of research protocols, especially in adapting cultural content and knowledge (24).
Encouraging equity
Within CBPR initiatives, community members and researchers equitably share power and control over all phases of the research process. Through the reciprocal transfer of knowledge, skills and capacities, decision-making power and resources, community members and researchers achieve equal ownership of the project information and outcomes. In turn, this sense of partnership translates into tangible benefits (22). For example, among older adults, CBPR has been shown to promote feelings of empowerment as respected members of the research team by providing them with the opportunity to impart their unique experiences and insights (25).
Central to the focus of this article, CBPR’s strength in upholding community integrity and empowerment runs parallel with palliative care’s emphasis on dignity-conserving care (26). Through treating patients as equals and encouraging family members’ involvement in the research process, the dignity approach promotes individual autonomy in decision-making and overall quality of life (26).
Examples of CBPR studies employed in palliative care
We have described the ways in which CBPR could be used to address specific challenges in palliative care research. Below, we provide a summary of studies that have implemented elements of this research strategy with terminally ill and end-of-life populations; though none have applied CBPR in its purest form, where partnership is present in every aspect of the research process.
Williams and colleagues employed a CBPR approach to design and implement a pilot randomized controlled trial that sought to improve quality of life among adults with end-stage acquired immunodeficiency syndrome (AIDS) (27,28). Building on an academic-community agency partnership, critical feedback regarding elements of the intervention (i.e., delivery of meditation and massage) and outcome assessments was obtained prior to implementing the study. In turn, the investigators were able to demonstrate significant improvements in quality of life among intervention (vs. control) patients, and credited CBPR as a tool that helped them to successfully design an intervention deemed acceptable by individuals with advanced AIDS.
In addition, several studies have demonstrated the benefits of using CBPR to address the needs of patients with advanced cancer. For example, Hanson and colleagues (29) used this approach to develop and implement a peer support training intervention for African Americans living with advanced cancer. Throughout the project, community stakeholder groups provided recommendations about how best to recruit and train lay persons who received (and ultimately delivered) the support intervention. The partnership was able to demonstrate broad reach of the intervention in the community, with 23 community organizations adopting its use (29).
Another study focusing on advanced cancer employed a CBPR approach that brought together clinicians, academicians, patients at the end of life (end users) to develop a method for addressing the problem of comorbid weight loss and eating difficulties among individuals receiving palliative care (15). The authors were able to successfully recruit participants for study (58% response rate) and credited the use of CBPR, in particular meaningful dialogue between the stakeholder groups and tailoring of the study methods, as being instrumental in their ability to successfully implement the study in this population.
Two ongoing projects provide further evidence of the growing interest in employing CBPR approaches in palliative care research, and in particular, with minority groups (30,31). In a multi-level partnership including community-based organizations, caregivers, Latina breast cancer survivors, healthcare providers, and researchers, Rush and colleagues developed and are evaluating an 8-week skill-building intervention targeting Latina breast cancer survivors and their family caregivers, with the aim of enhancing participants’ stress management, self care and communication abilities (30). In addition, CBPR methods are being used to develop a culturally appropriate palliative care program tailored to adult ages 60 years and older facing a terminal illness (31). Researchers are collecting information from potential end users and soliciting input from a community advisory board to develop the intervention, which will be pilot tested (using a telemedicine approach) to establish its feasibility and potential efficacy. The investigators hypothesize that use of CBPR principles will increase the likelihood of program acceptability, adoption across multiple agencies, and ultimately sustainability at the agency level.
Barriers to applying CBPR as a research tool in palliative care
Although CBPR holds promise for addressing knowledge gaps in palliative care, as noted in the above examples, several barriers and obstacles must be acknowledged.
Ethical challenges
Upholding ethical standards, especially patient privacy and protection, is of utmost importance in human subjects research. Among individuals receiving palliative care and their family members, participation may be viewed by research ethics boards as an undue burden with the potential to exacerbate the already fragile state of these groups (32). Because CBPR encourages collaborative decision-making, thereby upholding the ethical standard of patient autonomy, it requires a significant level of patient and family participation. Consequently, along with the benefit of direct involvement in CBPR emerges the residual challenge of increased time commitment by patients and families (33). Still, there is evidence that the demands of the research process may not be as overwhelming as expected: A participatory approach to studying palliative care revealed that patients actually welcome the opportunity to contribute to finding solutions for others facing advanced cancer (15).
Practical challenges
In addition to ethical issues, certain practical barriers also need to be surmounted. Patients’ own symptoms, including pain and fatigue, may preclude them from successfully completing self-report measures or adhering to structured interviews (34). For other patients, “gatekeeping” by healthcare providers may thwart their participation (34). Well-intentioned providers may attempt to protect patients from the burden of research involvement either by not offering consent, or acting on the patients’ behalf when they believe the patient would not wish to participate.
Although CBPR approaches are thought to place increased time demands on healthcare providers (17), recent work has challenged this assumption. Palliative care teams engaged in participatory research have noted that the protocol actually took less time and was less demanding than expected (15).
A final challenge is that of funding. Acknowledging this issue, funding agencies have begun to request applications for projects involving community partners. For example, The Centers for Disease Control and Prevention has required community involvement for research on health promotion and disease prevention, while The National Center for Minority Health and Health Disparities of the National Institutes of Health (NIH) recently released a call for applications specifically involving CBPR approaches to health research. In addition, funding by the Patient Centered Outcomes Research Institute (PCORI) requires meaningful engagement of key stakeholder groups (i.e., patients, caregivers, and clinicians) in all aspects of the research process, including study design, conduct, and dissemination of results. Despite this dramatic increase in federal and private foundation support for CBPR over the past decade, funding for CBPR interventions remains a small fraction of the billions of dollars in support of more traditional research efforts (16).
Conclusions
The goal of this article was to shed light on the potential benefits of employing CBPR approaches in palliative care and to offer tangible and specific examples of how this strategy has been previously employed. We also delineated several ethical and practical challenges that may arise when implementing CBPR with palliative care populations. Despite the identified barriers, we contend that CBPR is uniquely situated to address a range of methodological and practical challenges in palliative care research. Through targeted involvement of community members, CBPR initiatives ensure that the research has contextual and cultural relevance while fostering long-standing partnerships between communities and researchers. The natural overlap between palliative care’s emphasis on patient dignity and CBPR’s focus on empowerment will lend itself to fruitful researcher-community member partnerships.
Acknowledgements
We thank Karl Pillemer and Corinna Löckenhoff for their feedback on an initial draft of this manuscript.
Funding: This work was supported by the Edward R. Roybal Centers for Translation of the Behavioral and Social Sciences of Aging (P30AG022845 to M.C.R.). C Riffin is currently supported by a National Institute on Aging Training Grant (T32AG1934).
Footnote
*Catherine Riffin is now at Yale School of Medicine in the Division of Geriatrics.
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Aziz NM, Miller JL, Curtis JR. Palliative and end-of-life care research: embracing new opportunities. Nurs Outlook 2012;60:384-90. [Crossref] [PubMed]
- Crawford GB, Price SD., et al. Team working: palliative care as a model of interdisciplinary practice. Med J Aust 2003;179:S32-4. [PubMed]
- Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Source Washington (DC): National Academies Press (US), 2015.
- American Public Health Association Policy 2005-9: Supporting Public Health’s Role in Addressing Unmet Needs at the End of Life. Available online: http://apha.org/policies-and-advocacy/public-health-policy-statements/policy-database?q=2005-9
- Sepúlveda C, Marlin A, Yoshida T, et al. Palliative Care: the World Health Organization's global perspective. J Pain Symptom Manage 2002;24:91-6. [Crossref] [PubMed]
- Pillemer K, Chen EK, Riffin C, et al. Practice-Based Research Priorities for Palliative Care: Results From a Research-to-Practice Consensus Workshop. Am J Public Health 2015;105:2237-44. [Crossref] [PubMed]
- Riffin C, Pillemer K, Chen EK, et al. Identifying Key Priorities for Future Palliative Care Research Using an Innovative Analytic Approach. Am J Public Health 2015;105:e15-e21. [Crossref] [PubMed]
- Lorenz KA, Lynn J, Morton SC, et al. Methodological approaches for a systematic review of end-of-life care. J Palliat Med 2005;8 Suppl 1:S4-11. [Crossref] [PubMed]
- MacLeod A, Skinner MW, Low E. Supporting hospice volunteers and caregivers through community-based participatory research. Health Soc Care Community 2012;20:190-8. [Crossref] [PubMed]
- Kayser K, DeMarco RF, Stokes C, et al. Delivering palliative care to patients and caregivers in inner-city communities: challenges and opportunities. Palliat Support Care 2014;12:369-78. [Crossref] [PubMed]
- Israel BA, Schulz AJ, Parker EA, et al. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998;19:173-202. [Crossref] [PubMed]
- O’Fallon LR, Tyson F, Dearry A. Executive summary. In O’Fallon LR, Tyson FL, Dearry A. editors. Successful Models of Community-Based Participatory Research: Final Report. Research Triangle Park, NC: National Institute of Environmental Health Sciences, 2000:1-3.
- El-Jawahri A, Greer JA, Temel JS. Does palliative care improve outcomes for patients with incurable illness? A review of the evidence. J Support Oncol 2011;9:87-94. [Crossref] [PubMed]
- Morgan L, Howe L, Whitcomb J, et al. Improving communication and cost-effectiveness in the intensive care unit through palliative care: a review of literature. Dimens Crit Care Nurs 2011;30:133-8. [Crossref] [PubMed]
- Hopkinson JB, Wright DN, Corner JL. Seeking new methodology for palliative care research: challenging assumptions about studying people who are approaching the end of life. Palliat Med 2005;19:532-7. [Crossref] [PubMed]
- Minker M, Wallerstein N. editors. Community-based participatory research for health: From process to outcomes. San Francisco: Jossey-Bass, 2003.
- De las Nueces D, Hacker K, DiGirolamo A, et al. A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Serv Res 2012;47:1363-86. [Crossref] [PubMed]
- Dhanani S, Damron-Rodriguez J, Leung M, et al. Community-based strategies for focus group recruitment of minority veterans. Mil Med 2002;167:501-5. [PubMed]
- Doyle M, Timonen V. Lessons From a Community-Based Participatory Research Project: Older People's and Researchers' Reflections. Res Aging 2010;32:244-63. [Crossref]
- Leung MW, Yen IH, Minkler M. Community based participatory research: a promising approach for increasing epidemiology's relevance in the 21st century. Int J Epidemiol 2004;33:499-506. [Crossref] [PubMed]
- Minkler M. Community-based research partnerships: challenges and opportunities. J Urban Health 2005;82:ii3-12. [Crossref] [PubMed]
- Jones SP, Auton MF, Burton CR, et al. Engaging service users in the development of stroke services: an action research study. J Clin Nurs 2008;17:1270-9. [Crossref] [PubMed]
- Seifer SD, Michaels M, Collins S. Applying community-based participatory research principles and approaches in clinical trials: forging a new model for cancer clinical research. Prog Community Health Partnersh 2010;4:37-46. [Crossref] [PubMed]
- Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health 2010;100 Suppl 1:S40-6. [Crossref] [PubMed]
- Blair T, Minkler M. Participatory action research with older adults: key principles in practice. Gerontologist 2009;49:651-62. [Crossref] [PubMed]
- Östlund U, Brown H, Johnston B., et al. Dignity conserving care at end-of-life: a narrative review. Eur J Oncol Nurs 2012;16:353-67. [Crossref] [PubMed]
- Williams A, Selwyn PA, McCorkle R, et al. Application of community-based participatory research methods to a study of complementary medicine interventions at end of life. Complement Health Prac Rev 2005;10:91-104.
- Williams AL, Selwyn PA, Liberti L, et al. A randomized controlled trial of meditation and massage effects on quality of life in people with late-stage disease: a pilot study. J Palliat Med 2005;8:939-52. [Crossref] [PubMed]
- Hanson LC, Armstrong TD, Green MA, et al. Circles of care: development and initial evaluation of a peer support model for African Americans with advanced cancer. Health Educ Behav 2013;40:536-43. [Crossref] [PubMed]
- Rush CL, Darling M, Elliott MG, et al. Engaging Latina cancer survivors, their caregivers, and community partners in a randomized controlled trial: Nueva Vida intervention. Qual Life Res 2015;24:1107-18. [Crossref] [PubMed]
- Available online: http://grantome.com/grant/NIH/R21-AG046772-01A1
- de Raeve L. Ethical issues in palliative care research. Palliat Med 1994;8:298-305. [Crossref] [PubMed]
- Tomlinson D, Bartels U, Hendershot E, et al. Challenges to participation in paediatric palliative care research: a review of the literature. Palliat Med 2007;21:435-40. [Crossref] [PubMed]
- Ewing G, Rogers M, Barclay S, et al. Recruiting patients into a primary care based study of palliative care: why is it so difficult? Palliat Med 2004;18:452-9. [Crossref] [PubMed]


