Integrated pain and palliative medicine model
Introduction
Pain and symptom management are the essence of palliative care (1). Good and easily accessible pain management and palliative care are conceptually so analogous that there is a rising call to address them together. Both of them targets reduction of suffering, restoring function and improving quality of life (QOL) (2). Integrated pain and palliative medicine can therefore be a novel contribution or ‘a way of dignified life and death in patients suffering from chronic and life-threatening diseases’ of healthcare system to the mankind. The purpose of this review is to ponder upon the need, logistics, advantages, barriers and recommendations for integration of pain and palliative medicine and to propose an ‘Integrated pain-palliative medicine’ (IPPM) model.
The need of integrating pain and palliative medicine
Palliative care has been defined by World Health Organization (WHO) as “an approach that improves the QOL of patients (adults and children) and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual (2)”. Worldwide 35 million people requires palliative care and with the rise of aging population, cancer and lifestyle disorders the need and the dearth of good palliative care services is only going to increase (3,4). What is required is the recognition of this need jointly by the governing and health care authorities.
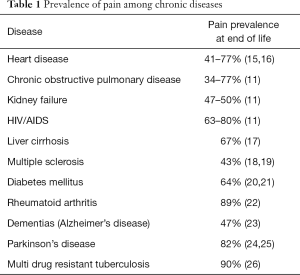
Pain is often the most distressing and feared symptom (5-9). An estimated 53% and 64% of patients with cancer and advanced cancer respectively suffer from pain with more than one-third of patients having moderate-severe pain (10). An approximately 25 million patients die in pain every year (11). Cancer pain is usually multifactorial in etiology and may be due to (I) tumor itself (nerve or bone compression); (II) iatrogenic (anti-cancer treatments); (III) debility; (IV) completely different etiology (prolapsed intervertebral disc or osteoarthritis); or (V) non-physical causes (psychological distress) (12,13). Zech et al. found cancer pain to be somatic, visceral, neuropathic and mixed in 35%, 17%, 9% and remainder patients respectively (14). Pain is also prevalent in other chronic and life-threatening diseases (Table 1) (15,16).
Full table
These high prevalence rates define the magnitude of unrelieved pain and indicate that the adequate pain relief is not available to the majority. Adequate pain management is considered as a ‘fundamental human right’ (27,28). Its importance is reflected by its recognition as the ‘Fifth vital sign’ by Joint Committee on Accreditation of Health Organizations (JCAHO) and the UN Committee on Economic, Social and Cultural Rights emphasizing that it is critical to avoid pain to allow the patients to die with dignity (2,29,30).
Pain is a bio-psychosocial phenomenon and physical, social, spiritual, economic and cognitive factors underlining the experience of total pain may act as originators of other symptoms as well (31-36). Pain has deleterious consequences on emotional health and may be associated with cognitive impairment and sleep disturbance (33,37,38). Therefore, going according to the diction “Need is the mother of all inventions”; pain and palliative medicine should be integrated and instituted with a goal of delivering co-ordinated and consistent services to those in need.
Integrating palliative care into pain training and practice
The facts justifying the integration include:
- There is a shortage of both pain and palliative care physicians in developing countries. An integrated model will ensure more manpower available to address the rising needs;
- A lot of pain physicians are already performing interventional techniques for cancer pain;
- Cancer pain and pain in cancer are not synonymous. Cancer patients do suffer from a number of non-cancer etiologies which might be better addressed by pain physician.
Need of the hour: sensitizing, educating and training the pain fellows and physicians in:
- Evidence based pain assessment and management including prescribing oral morphine;
- Comprehensive patient care;
- Principles of palliative care;
- Symptom assessment and alleviation.
The advantages of IPPM services
An integrated team approach will have far reaching consequence on strengthening the concept of ‘palliative care’. Some of the stipulated and achievable advantages are:
- Pain can be used both as an indicator of need as well as outcome measure of palliative care. A number of questionnaires assessing various dimensions of QOL have been devised for e.g., ‘Medical Outcomes Short-Form Health Survey Questionnaire 36’ (SF-36), and the ‘European Organization for Research and Treatment of Cancer Quality of Life Core Questionnaire’ (EORTC QLQ-C30). For assessment of pain in cognitively impaired and elderly patients, special tools such as Doloplus-2 are present (39-44). Adapted tools such as the “African version of Palliative Outcome Scale” are available to be used in developing countries;
- A broad multidisciplinary approach will rope in expertise with the common intention of providing a good QOL;
- Early and efficient pain control in conjunction with palliative care leads to better outcomes of curative therapies and increased cancer survival (5,45);
- Optimal pain management at all stages of illness in a terminally ill patient will allow patients to live as actively as possible and avoid needless suffering.
The existing barriers retarding the establishment of IPPM
- Lack of evidence based education and training opportunities: despite the growing evidence physicians and nurses still lack the basic concepts of pain assessment and management (46-50). Inadequate assessment usually results in inadequate pain management (13). Health care professionals dis-interest may be due to lack of: (i) recognition of palliative care as a specialty; (ii) evidence-based standards and guidelines; (iii) recognition both by patients and colleagues and; (iv) ignorance by private and corporate sector as they regard it as a non-profitable business. Owing to intensive efforts palliative medicine is officially certified in a number of countries like United Kingdom, Ireland, Australia, New Zealand, Taiwan, Hong Kong, Poland, Romania and United states (51-53). It is required to follow the same in other countries as well (53).
- Inadequate access to essential drugs especially opioids: not only is the access to drugs but also access to all the formulations of available drugs is inadequate. An estimated 83% of countries have low to non-existent access to opioids (54). Strict regulations on opioid prescribing, fear and misconceptions about opioid over-dosage, tolerance, addiction and diversion contributes to inadequate opioid supply and prescription (55,56). Concerns regarding altered pharmacokinetics of opioids and exaggerated pharmacodynamic effects in patients with organ dysfunction may act as hurdle in adequate opioid prescribing.
- Under-reporting of symptoms due to: (i) giving less importance to symptom owing to the notion that symptoms would subside with disease control; (ii) fear of being tagged as a complaining patient; (iii) misconceptions like addiction and tolerance; and (iv) fear of effects like constipation and respiratory depression leading to ‘opiophobia’ (56,57)./
- Problems inherent to team approach and human nature such as: (i) split responsibilities; (ii) role overlap and conflicts; (iii) duplication or fragmentized efforts; (iv) promotion of superiority, seniority and groups; (v) imposition of one’s perception, influencing others and claiming one modality of treatment to be superior to others; (vi) reluctance to initiate efforts, take accountabilities, share resources and manpower.
- Lack of infrastructure and funding.
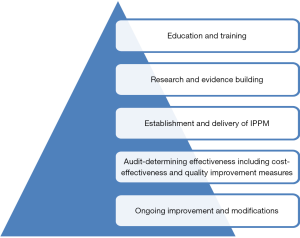
Recommendations-converting concept into reality! (Figure 1)
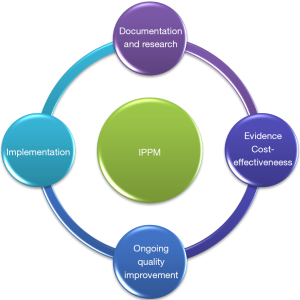
Recommendations based on evidence and expert opinion ensures quality and consistent practices. It is important to recognize that good pain and palliative care needs are required across different disease groups, to broaden the horizon of palliative care and to improve QOL in whomsoever patients it is required (58). A successful IPPM model should include the following (Figure 2).
Education, training and building manpower
Inclusion of pain and palliative care in undergraduate curriculum would enable the budding physicians to get accustomed with the key concepts such as symptom relief. Early introduction of knowledge may improve cancer pain control (59). WHO recommends inclusion of pain in ‘courses leading to basic professional qualification’ and multi-professional cancer pain education has been introduced by some (60,61). Development and reinforcement of evidence based curriculum like ‘European Association of Palliative Care (EAPC) undergraduate curriculum for physicians’, ‘Core Curriculum for Professional Education in Pain’ and ‘Recommendations for Nursing Practice in Pain Management’ (62,63).
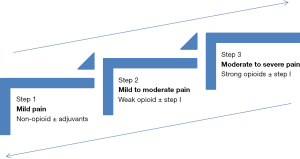
- Transforming ‘primary care physicians’ into ‘primary pain and palliative care physicians’ by imparting them basic concepts of pain assessment and management including the mechanism based analgesia and the WHO analgesic ladder (Figure 3) (64,65).
- Creation of ‘pain and palliative care specialist’ with expertise in dealing complex cases and advanced interventions. Following patients may be referred to benefit from specialized pain services (66):
- VAS of ≥60;
- Severe pain;
- Neuropathic pain;
- Side-effects with medications provided and;
- Unrelieved pain for more than 2 weeks in spite of best therapy at primary care.
- Multidisciplinary palliative care teams, in which health care providers from all specialties are trained, educated and facilitate knowledge exchange to improve competence and hence minimize substandard cancer pain treatment (67). This should include:
- Co-location of services;
- Good referral systems eliminating the need of waiting for appointments or segregated appointments on different days stretching the patient’s economic and time constraints;
- Electronic referral of cases eliminating the time draining process of procuring files, rearranging them, finding the missing links, re-referring the patient to other concerned specialties and acquainting the primary physician with the treatment changes;
- Shared information system, care, decision making and discharge planning;
- Designation of a responsible coordinating person.
- Creation of ‘pain and palliative care nurses’ trained in acknowledging and managing factors contributing to ‘total pain’ and other symptoms (13). Nurses may play a pivotal role in keeping the patient pain and symptom free by early assessment and intervention (13). However inadequate assessment and imparting more strength to their own observation results in suboptimal pain management (47,68). It is required to impart core concepts like ‘pain is what and where the patient says it is’ (69), total pain, use of WHO analgesic ladder, titration of analgesics, early recognition and management of side-effects.
- Empowering social workers and caregivers by educating them about pain and other symptom recognition so that cost-effective services can be provided as close to home as possible. A number of home based palliative programs like Kaiser Permanente’s In-Home Palliative Care program and Sutter Health’s Advanced Illness Management (AIM) program are operational with the aim of home based care of patients with advanced illnesses. ‘Home based palliative care’ has been found to be associated with improved patient satisfaction; patient’s more likely to die in accordance with their wishes, reduced emergency visits, inpatient admissions and cost (70-72). The American pain society recommends healthcare professionals to educate cancer patients and their caregivers about cancer pain and its management (73).
Research and evidence building
Development and dissemination of evidence based:
- Guidelines, recommendations and algorithms for effective analgesia at all stages in terminally ill patients (17). Dr. Cicely Saunders conceptualized the pain associated with the dying process as the ‘total pain’ composed of four components: (I) physical; (II) emotional; (III) interpersonal conflicts; and (IV) nonacceptance of one’s own dying. Neglecting any of the components may result in inadequate pain relief (69,74,75);
- Adoption and adaptation of multi-dimensional and scientifically validated assessment tools like ‘Edmonton symptom assessment scale’ (ESAS), ‘Memorial symptom assessment scale’ (MSAS), ‘Needs at the end of life screening tool’ and ‘Palliative Outcome Scale’ as their use may be associated with improved patient and family outcomes (76,77). Most of the existing tools fail to address all the dimensions relevant for palliative care pain assessment (78). Trowbridge et al. established that use of standardized pain assessment improved pain management and reduced reported pain severity in cancer patients (79);
- Promotion of research and proper documentation to facilitate availability of data and outcome measures of IPPM services (Figure 4);
- Monitor the cost-effectiveness and impact of such integrated services on the community, patient and healthcare system to ensure consistent care (80,81);
- Neuropathic pain is found in a substantial portion of cancer patients either alone or in combination with nociceptive pain (14,82,83). Neuropathic pain is difficult to treat and requires ‘adjuvant analgesics’ (84). Not only are the physicians ignorant of the diagnostic but also the therapeutic modalities available for neuropathic pain. Most of the guidelines for treatment of neuropathic pain including data on pharmacodynamic variables like ‘Number needed to treat’ (NNT) and ‘Number needed to harm’ (NNH) have been developed in non-cancer conditions like diabetic neuropathy and extrapolated to be used in neuropathic cancer pain (84-86). Research pertinent to prevalence, validity of different neuropathic tools in cancer pain and efficacy of adjuvants in neuropathic cancer pain is required to fill this existing gap;
- Recommendations for special groups with differing needs such as pediatric patients. About 1.2 million children suffering from congenital heart diseases, protein-energy malnutrition, meningitis, cardiovascular and other chronic diseases require palliative care (58). There is scarcity of data available on symptoms experienced by this patient group (87,88). An estimated 53–91.5% of pediatric cancer patients requiring palliative care at end of life suffer from pain (89-93). Children presents unique challenges in both assessment as well as management and are at risk of under-treatment due to (88,94-99): (I) scarcity of verbal communicators of presence, intensity and quality of pain especially in neonates and toddlers; (II) failure to identify ‘non-physical’ like psychological and social contributors to pain; (III) ‘pediatric gap’ existing in the pharmaceutical world (100-102); (IV) misconceptions that children have less sensitivity to pain (101); (V) inability to use important routes of opioid delivery such as submucosal, sublingual and patient controlled analgesia in neonates; (VI) fear of doing harm and side-effects; (VII) parent’s denial, considering pain as a sign of deterioration; (VIII) absence of expertise required to perform interventions in pediatric patients. Effective assessment and management should take developmental stage into consideration (103). The food and drug modernization act has stimulated a number of pediatric clinical studies but still few analgesic drugs are investigated in pediatric patients (88,100). Teaching physicians, nurses and guardians in identification of non-verbal indicators of pain, use of pain scales such as ‘Wong-baker faces pain rating scale’ as well as pharmacological and non-pharmacological pain management is required to tackle unrelieved pain (104).
Establishment and delivery
- A global task force to assess the feasibility, existing barrier and gaps;
- Strong inter-professional networks consisting of pain, palliative care, geriatric, family and other physicians;
- Partnership with NGO’s to deliver efficient door step palliative care;
- Integration of IPPM services into countries healthcare system as recommended by the worldwide palliative care alliance and establishment of National and regional IPPM centers (105);
- Proper allocation of global, national and state funds to ensure adequate availability of manpower, equipment and supplies;
- Easily accessible IPPM forums bringing care providers to care givers, addressing their needs and problems;
- Pain management guidelines should be integrated into institution’s palliative care program as the use of simple institutional protocol has been associated with reduced cancer pain severity (106);
- Timely institution of interventional pain procedures in severe pain where pharmacological management is ineffective or associated with side effects (107,108). It has been estimated that 10–15% of cancer patients with pain may require interventional treatments considered now as the ‘fourth step’ of WHO analgesic ladder (Figure 5) (109-112). Analgesic interventions can be classified according into:
- Intention of the intervention: (i) diagnostic; (ii) therapeutic;
- Nervous system targeted: (i) somatic blocks; (ii) sympathetic blocks;
- On the basis of modality used: (i) anaesthetic blocks: local anaesthetic; (ii) neurolytic blocks: chemical—alcohol, phenol, glycerol etc; thermal—conventional, pulsed and cooled radiofrequency ablation (RFA); surgical neurolysis [some of the neurolytic blocks found to be of proven value in cancer patients are: (a) neurolytic celiac plexus block (NCPB) for intractable upper abdominal visceral pain originating from structures innervated by celiac plexus (113-116); (b) superior hypogastric plexus block (SHPB) for visceral pelvic pain (110,117); (c) ganglion impar block for perineal cancer pain and radiation induced proctitis pain (118,119)]; (iii) neuromodulation: spinal cord stimulation, peripheral nerve stimulation, deep brain stimulation; (iv) neuraxial drug delivery systems: delivery of drugs like opioids, alfa 2 agonists, local anaesthetics, ziconotide and baclofen etc through epidural or intrathecal drug delivery system (111).
- Ensuring availability, rational use and inclusion of non-opioids, opioid and adjuvant analgesics into essential drugs list. Morphine and other opioid analgesics have been regarded as essential medicines by a WHO expert committee (120-122). The International Association for Hospice and Palliative Care (IAHPC) has recommended a list of 33 essential palliative care drugs (123). Existing drug laws should be amended, if found to be overly restrictive;
- Establishment of IPPM departments in corporate and private institutions. Uniform implementation throughout the healthcare system is essential for equitable delivery. It is important to make them realize that the paying capacity of people has changed and there is a segment which needs quality services even at end of life. When this segment can spend a substantial amount on curative treatments in the hope of a cure, they will be and are eager to spend for maintenance of symptom-free and quality life as well. Recognition of the above facts have resulted in a phenomenal shift in the developed countries with more and more palliative care services being provided by for-profit organizations. Developing palliative and hospice care programs may act both as cost and quality incentive for healthcare providers and organizations (55). To be fully operational such departments should have both outpatients as well as inpatient facilities;
- Collaboration with allied organizations with the aim of conducting countrywide surveys on prevalence and establishing guidelines like the one between Indian association of palliative care and Indian society of critical care for end of life guidelines (124,125).
Essential ingredients for designing IPPM
- Review of availability of resources;
- Elimination of traditional barriers;
- Education and training of physicians, nurses and patients;
- Communication/collaboration/partnership and networking;
- Information sharing;
- Strategies adopted on the basis of prevailing needs, local health policies, economic and cultural context.
Organizational framework of IPPM model
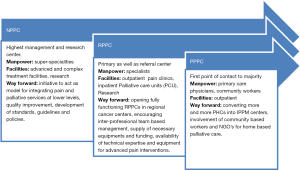
Pain and palliative care services should be integrated at all level of healthcare system (Figure 6):
- Primary pain and palliative care centers (PPPC): the bottom-up description emphasizes the importance of primary healthcare centers as the first access to health system to a majority of population. These centers usually operate on outpatient basis. It is importance to train the manpower at PHC in efficient, cost-effective and home-based pain and symptom management; with early referral to regional centers of complex cases;
- Regional pain and palliative care centers (RPPC): these centers may act both as primary or referral centers, have both outpatient clinics and inpatient palliative care units (PCU) and are already operational (to varying extents) in regional and national cancer centers. These centers should be manned by ‘inter-disciplinary palliative care teams’ apt to deal with complex cases requiring rapid opioid titration, high doses of opioids, opioid addicts and interventions. Equipment necessary for performance of above interventions like should be made available at these and higher centers. Board room discussions of complex cases and research facilities should be encouraged to ensure delivery of comprehensive and evidence based management;
- National pain and palliative care centers (NPPC): these centers will act as the highest level management and research centers and should have all the super-specialties including experts in highly advanced interventions like spinal cord stimulators, intrathecal opioid device implantation in recalcitrant cases. National surveys to enumerate the prevalence of pain and palliative care requirements in various population groups should be conducted at these centers. To be successfully implemented it is important to have a hassle free referrals of difficult and recalcitrant cases from one to a higher center as every patient has the ‘right to be referred’ and every physician is ‘obliged to refer’ (72).
Above model and recommendations provide a broad base; with scope of modifications and diversification to suit different cultural, socio-economic contexts as well support from government and various non-government organizations.
Conclusions
Pain is a global problem among chronic and terminally ill patients requiring palliative care. The physical, psychological, socioeconomic and spiritual factors underlying the total pain experience may also act as the underlying cause of other distressing symptoms. Therefore, meticulous pain management conforming to individual patient needs is of utmost importance to avoid needless suffering. Widespread dissemination of principles of cancer pain assessment, management, use of WHO analgesic ladder, employing interventional pain management in severe, recalcitrant pain with early and ego-free referral among inter-disciplinary pain and palliative care team members are required to have a multipronged approach and to curb this exponentially rising problem of ‘unrelieved pain’. With the prevailing shortage of manpower apt to deal with this problem, rising trends in cancer prevalence, patients with advanced cancer living longer and in pain; it is required to educate healthcare professional in pain and other symptom management, formulate policies, standards, guidelines and evaluate their effectiveness now so that we are ready for tomorrow. To achieve an equitable delivery to those in needs, it is of vital importance to introduce IPPM services at all levels of healthcare system including corporate sector. Proper education and training to build adequate manpower apt to manage pain and other symptom, involvement of NGO’s and community workers are required to ensure cost-effective ‘Home and community based’ pain and palliative services’. The authors realize that it is going to be a difficult but not an invincible task.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Howie L, Peppercorn J. Early palliative care in cancer treatment: rationale, evidence and clinical implications. Ther Adv Med Oncol 2013;5:318-23. [Crossref] [PubMed]
- WHO Definition of Palliative Care. Available online: www.who.int/cancer/palliative/definition/en
- Stjernsward J, Clark D. Palliative medicine-a global perspective. In: Doyle D, Hanks G, Cherny N, et al, editors. Oxford textbook of palliative medicine, 3rd ed. Oxford: Oxford University Press, 2004:1197e1224.
- Incidence and mortality data. Available online: www.who.int/whr/2003/en/Annex2-en.pdf
- Walid MS, Donahue SN, Darmorhray DM, et al. The fifth vital sign-what does it mean. Pain Pract 2008;8:417-22. [Crossref] [PubMed]
- Breitbart W. Psychiatric management of cancer pain. Cancer 1989;63:2336-42. [Crossref] [PubMed]
- Given B, Given CW, McCorckle R, et al. Pain and fatigue management: the results of a nursing randomized clinical trial. Oncol Nurs Forum 2002;29:949-56. [Crossref] [PubMed]
- Ferrell BR, Dean G. The meaning of cancer pain. Semin Oncol Nurs 1995;11:17-22. [Crossref] [PubMed]
- Grond S, Zech D, Diefenbach C, et al. Prevalence and pattern of symptoms in patients with cancer pain: a prospective evaluation of 1635 cancer patients referred to a pain clinic. J Pain Symptom Manage 1994;9:372-82. [Crossref] [PubMed]
- Van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 2007;18:1437-49.
- Solano JP, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage 2006;31:58-69. [Crossref] [PubMed]
- Davis MP, Dickerson D, Pappagallo M, et al. Palliative care: long term solution for long- term care. Part 2. Types of pain: a review. Home Care Provid 2001;6:126-33. [Crossref] [PubMed]
- Mehta A, Chan LS. Understanding of the concept of total pain: A prerequisite for pain control. J Hosp Palliat Nurs 2008;10:26-32. [Crossref]
- Zech DF, Grond S, Lynch J, et al. Validation of World Health Organization guidelines for cancer pain relief. Pain 1995;63:65-76. [Crossref] [PubMed]
- Higginson IJ, editor. Palliative and terminal care healthcare needs assessment: The epidemiologically based needs assessment reviews. New York: CRC Press, 1997.
- Global Health Estimates. Causes of Death 2000-2011. World Health Organization, 2013. Available online: www.who.int/healthinfo/global_burden_disease/en
- Rogal SS, Winger D, Bielefeldt K, et al. Pain and opioid use in chronic liver disease. Dig Dis Sci 2013;58:2976-85. [Crossref] [PubMed]
- Solaro C, Brichetto G, Amato MP, et al. The prevalence of pain in multiple sclerosis: A multicenter cross-sectional study. Neurology 2004;63:919-21. [Crossref] [PubMed]
- Higginson IJ, Hart S, Silber E, et al. Symptom prevalence and severity in people severely affected by multiple sclerosis. J Palliat Care 2006;22:158-65. [PubMed]
- Davies M, Brophy S, Williams R, et al. The prevalence, severity and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care 2006;29:1518-22. [Crossref] [PubMed]
- Halawa MR, Karawagh A, Zeidan A, et al. Prevalence of painful diabetic peripheral neuropathy among patients suffering from diabetes mellitus in Saudi Arabia. Curr Med Res Opin 2010;26:337-43. [Crossref] [PubMed]
- Chung TC, Yen JH, Ou TT, et al. Prevalence of neuropathic pain in patients with rheumatoid arthritis. Formosan Journal of Rheumatology 2009;23:19-24.
- Zwakhalen SM, Koopmans RT, Geels PJ, et al. The prevalence of pain in nursing home residents with dementia measured using an observational pain scale. Eur J Pain 2009;13:89-93. [Crossref] [PubMed]
- Higginson IJ, Gao W, Saleem TZ, et al. Symptoms and quality of life in late stage Parkinson syndromes: a longitudinal community study of predictive factors. PLoS One 2012;7:e46327. [Crossref] [PubMed]
- Saleem TZ, Higginson IJ, Chaudhuri KR, et al. Symptom prevalence, severity and palliative care needs assessment using the Palliative Outcome Scale: A cross-sectional study of patients with Parkinson’s disease and related neurological conditions. Palliat Med 2013;27:722-31. [Crossref] [PubMed]
- Sagwa E, Mantel-Teeuwisse A, Ruswa N, et al. The burden of adverse events during treatment of multi-drug-resistant tuberculosis in Namibia. South Med Rev 2012;5:6-13. [PubMed]
- Brennan F, Carr D, Cousins M. Pain management: a fundamental human right. Anesth Analg 2007;105:205-21. [Crossref] [PubMed]
- Fishman SM. Recognizing pain management as a human right: a first step. Anesth Analg 2007;105:8-9. [Crossref] [PubMed]
- Dahl J. Implementing the JCAHO pain management standards. American Pain Society 19th Annual Meeting November 2–5, 2000, Atlanta, Georgia. Accessed July 9, 2007.
- Committee on Economic, Social and Cultural Rights (CESCR) General Comment 14, para. 25. Available online: https://www1.umn.edu/humanrts/gencomm/escgencom14.htm
- Engel GL. The need for a new medical model: A challenge for biomedicine. Science 1977;196:129-36. [Crossref] [PubMed]
- Saunders C. Introduction: history and challenge. In: Saunders C, Sykes N, editors. The Management of Terminal Malignant Disease. London, Great Britain: Hodder and Stoughton, 1993:1-14.
- Montes-Sandoval L. An analysis of the concept of pain. J Adv Nurs 1999;29:935-41. [Crossref] [PubMed]
- Strang P. Emotional and social aspects of cancer pain. Acta Oncol 1992;31:323-26. [Crossref] [PubMed]
- Allard P, Maunsell E, Labbe J, et al. Educational interventions to improve cancer pain control: a systemic review. J Palliat Med 2001;4:191-203. [Crossref] [PubMed]
- Saunders C. Nature and management of terminal pain. In: Shotter EF, editor. Matters of Life and Death. London: Darton, Longman & Todd, 1970:15-26.
- Ko HJ, Seo SJ, Youn CH, et al. The association between pain and depression, anxiety, and cognitive function among advanced cancer patients in the hospice ward. Korean J Fam Med 2013;34:347-56. [Crossref] [PubMed]
- K C B, Binti Mohd Yusoff Z, Alrasheedy AA, et al. The characteristics and the pharmacological management of cancer pain and its effect on the patients’ daily activities and their quality of life: a cross - sectional study from Malaysia. J Clin Diagn Res 2013;7:1408-13. [PubMed]
- National committee for Quality Assurance/physician Consortium for performance Improvement (2008). Palliative Care Clinician Performance measurement Set.
- Graham B. Generic health instruments, visual analog scales, and the measurement of clinical phenomena. J Rheumatol 1999;26:1022-3. [PubMed]
- Jensen MP. The validity and reliability of pain measures in adults with cancer. J Pain 2003;4:2-21. [Crossref] [PubMed]
- Rosier EM, Iadarola MJ, Coghill RC. Reproducibility of pain measurement and pain perception. Pain 2002;98:205-16. [Crossref] [PubMed]
- Scott DL, Garrood T. Quality of life measures: use and abuse. Baillieres Best Pract Res Clin Rheumatol 2000;14:663-87. [Crossref] [PubMed]
- Lefebvre-Chapiro S. The DOLOPLUS® 2 scale - evaluating pain in the elderly. European Journal of Palliative Care 2001;8:191-4.
- Lillemoe KD, Cameron JL, Kaufman HS, et al. Chemical splanchnicectomy in patients with unresectable pancreatic cancer. A prospective randomized trial. Ann Surg 1993;217:447-55. [Crossref] [PubMed]
- Lin CC. Enhancing management of cancer pain: contribution of the internal working model. Cancer Nurs 1998;21:90-96. [Crossref] [PubMed]
- Gunnarsdottir S, Donovan HS, Ward S. Interventions to overcome clinician- and patient-related barriers to pain management. Nurs Clin North Am 2003;38:419-34. [Crossref] [PubMed]
- Rushton P, Eggett D, Sutherland CW. Knowledge and attitudes about cancer pain management: a comparison of oncology and non-oncology nurses. Oncol Nurs Forum 2003;30:849-55. [Crossref] [PubMed]
- Donnelly G. Theory based nursing practice in pain management. Concern 1996;25:21-4. [PubMed]
- Green CR, Wheeler JR, LaPote F. Clinical decision making in pain management: contributions of physician and patient characteristics to variations in practice. J Pain 2003;4:29-39. [Crossref] [PubMed]
- Hoy AM. Training specialists in palliative medicine. In: Doyle D, Hanks G, Cherny N, et al, editors. Oxford textbook of palliative medicine. Oxford University Press, 2004:1167-8.
- Holman GH, Smith DC. Board certification in palliative care in U.S. physicians. J Pain Symptom Manage 1999;17:309-10. [Crossref] [PubMed]
- Centeno C, Noguera A, Lynch T, et al. Official certification of doctors working in palliative medicine in Europe: data from an EAPC study in 52 European countries. Palliative Medicine 2007;21:683-7. [Crossref] [PubMed]
- Seya MJ, Gelders SF, Achara OU, et al. A first comparison between the consumption of and the need for opioid analgesics at country, regional, and global levels. J Pain Palliat Care Pharmacother 2011;25:6-18. [Crossref] [PubMed]
- Lebaron V, Beck SL, Maurer M, et al. An ethnographic study of barriers to cancer pain management and opioid availability in India. Oncologist 2014;19:515-22. [Crossref] [PubMed]
- Maltoni M. Opioids, pain and fear. Ann Oncol 2008;19:5-7. [Crossref] [PubMed]
- Fotedar KK. WHO ladder-relevance in today’s world. Int J Perioper Ultra Appl Technol 2013;2:49-53. [Crossref]
- World health organization. Global atlas of palliative care at end of life. Available online: www.who.int
- Wilkes G, Lasch KE, Lee JC, et al. Evaluation of a cancer education module. Oncol Nurs Forum 2003;30:1037-43. [Crossref] [PubMed]
- World Health Organization. Cancer Pain Relief. 2nd ed. Geneva: World Health Organization; 1996. Available online: whqlibdoc.who.int/publications/9241544821.pdf
- Sloan PA, Plymale PA, LaFountain P, et al. Equipping medical students to manage cancer pain in a comparison of three educational methods. J Pain Symptom Manage 2004;27:333-42. [Crossref] [PubMed]
- International Association for the Study of Pain (IASP). Core Curriculum for Professional Education in Pain. 2nd ed. Seattle, WA: IASP, 1997a.
- Pain Society. Recommendations for Nursing Practice in Pain Management. London: Pain Society, 2002.
- Sindrup SH, Jensen TS. Efficacy of pharmacological treatments of neuropathic pain: an update and effect related to mechanism of drug action. Pain 1999;83:389-400. [Crossref] [PubMed]
- Vargas-Schaffer G. Is the WHO analgesic ladder still valid? Can Fam Physician 2010;56:514-7. [PubMed]
- Ahmedzai SH, Costa A, Blengini C, et al. A new international framework for palliative care. Eur J Cancer 2004;40:2192-200. [Crossref] [PubMed]
- Plymale MA, Sloan PA, Johnson M, et al. Cancer pain education: a structured clinical instruction module for hospice nurses. Cancer Nurs 2001;24:424-9. [Crossref] [PubMed]
- McCaffery M, Ferrell BR. Nurses’ knowledge about cancer pain: a survey of five countries. J Pain Symptom Manage 1995;10:356-69. [Crossref] [PubMed]
- Leleszi JP, Lewandowski JG. Pain Management in End-of-Life Care. J Am Osteopath Assoc 2005;105:S6-11. [PubMed]
- Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 2007;55:993-1000. [Crossref] [PubMed]
- Enguidanos SM, Cherin D, Brumley R. Home-based palliative care study: site of death, and costs of medical care for patients with congestive heart failure, chronic obstructive pulmonary disease, and cancer. J Soc Work End Life Palliat Care 2005;1:37-56. [Crossref] [PubMed]
- Brumley RD, Enguidanos S, Cherin DA. Effectiveness of a home-based palliative care program for end-of-life. J Palliat Med 2003;6:715-24. [Crossref] [PubMed]
- American Pain Society. Guidelines for the Management of Cancer Pain in Adults and Children. Available online: www.ampainsoc.org
- Saunders CM. The challenge of terminal care. In: Symington T, Carter RL, editors. Scientific Foundations of Oncology. London, England: Heinemann, 1976:673-9.
- Paradise LA, Raj PP. Competency and certification of pain physicians. Pain Pract 2004;4:235-44. [Crossref] [PubMed]
- Ferris FD, Balfour HM, Bowen K, et al. A model to guide patient and family care: based on nationally accepted principles and norms of practice. J Pain Symptom Manage 2002;24:106-23. [Crossref] [PubMed]
- Weissman DE, Meier DE. Identifying Patients in Need of a Palliative Care Assessment in the Hospital Setting: A Consensus Report from the Center to Advance Palliative Care. J Palliat Med 2011;14:17-23. [Crossref] [PubMed]
- Hølen JC, Polit C, Hjermstad MJ, et al. Pain Assessment Tools: Is the Content Appropriate for Use in Palliative Care? J Pain Symptom Manage 2006;32:567-80. [Crossref] [PubMed]
- Trowbridge R, Dugan W, Jay SJ, et al. Determining the effectiveness of a clinical-practice intervention in improving the control of pain in outpatients with cancer. Acad Med 1997;72:798-800. [Crossref] [PubMed]
- Smith D, Caragian N, Kazlo E, et al. Can we make reports of end-of-life care quality more consumer-focused? Results of a nationwide quality measurement program. J Palliat Med 2011;14:301-7. [Crossref] [PubMed]
- Hardy JR, Haberecht J, Maresco-pennisi D, et al. Audit of the care of the dying in a network of hospitals and institutions in Queensland. Intern Med J 2007;37:315-9. [Crossref] [PubMed]
- Caraceni A, Portenoy RK. IASP task force: an international survey of cancer pain characteristics and syndromes. Pain 1999;82:263-74. [Crossref] [PubMed]
- Grond S, Radbruch L, Meuser T, et al. Assessment and treatment of neuropathic cancer pain following WHO guidelines. Pain 1999;79:15-20. [Crossref] [PubMed]
- Vadalouca A, Raptis E, Moka E, et al. Pharmacological treatment of neuropathic cancer pain: A comprehensive review of current literature. Pain Practice 2012;12:219-51. [Crossref] [PubMed]
- Orza F, Boswell MV, Rosenberg SK. Neuropathic pain: review of mechanisms and pharmacologic management. NeuroRehabilitation 2000;14:15-23. [PubMed]
- Boulton AJM, Gries FA, Jervell JA. Guidelines for the diagnosis and outpatient management of diabetic peripheral neuropathy. Diabet Med 1998;15:508-14. [Crossref] [PubMed]
- Page JC, Chen EY. Management of painful diabetic neuropathy. A treatment algorithm. J Am Podiatr Med Assoc 1997;87:370-79. [Crossref] [PubMed]
- Drake R, Frost J, Collins JJ. The symptoms of dying children. J Pain Symptom Manage 2003;26:594-603. [Crossref] [PubMed]
- Grégoire MC, Frager G. Ensuring pain relief for children at the end of life. Pain Res Manag 2006;11:163-71. [Crossref] [PubMed]
- Wolfe J, Grier HE, Klar N, et al. Symptoms and suffering at the end of life in children with cancer. N Engl J Med 2000;342:326-33. [Crossref] [PubMed]
- Hongo T, Watanabe C, Okada S, et al. Analysis of the circumstances at the end of life in children with cancer: Symptoms, suffering and acceptance. Pediatr Int 2003;45:60-4. [Crossref] [PubMed]
- Jalmsell L, Kreicberg U, Onelov E, et al. Symptoms affecting children with malignancies during the last month of life: A nationwide follow-up. Pediatrics 2006;117:1314-20. [Crossref] [PubMed]
- Goldman A, Hewitt M, Collins GS, et al. Symptoms in children/young people with progressive malignant disease: United Kingdom Children’s Cancer Study Group/Paediatric Oncology Nurses Forum Survey. Pediatrics 2006;117:e1179-86. [Crossref] [PubMed]
- Galloway KS, Yaster M. Pain and symptom control in terminally ill children. Pediatr Clin North Am 2000;47:711-46. [Crossref] [PubMed]
- Liben S. Pediatric palliative medicine: Obstacles to overcome. J Palliat Care 1996;12:24-8. [PubMed]
- Liben S, Goldman A. Home care for children with life-threatening illness. J Palliat Care 1998;14:33-38. [PubMed]
- McGrath PJ, Finley GA. Attitudes and beliefs about medication and pain management in children. J Palliat Care 1996;12:46-50. [PubMed]
- Chaffee S. Pediatric palliative care. Prim Care 2001;28:365-90. [Crossref] [PubMed]
- Groopman J. The Pediatric Gap. The New Yorker, January 10, 2005.
- Roberts R, Rodriguez W, Murphy D, et al. Pediatric drug labeling: Improving the safety and efficacy of pediatric therapies. JAMA 2003;290:905-11. [Crossref] [PubMed]
- American Academy of Pediatrics. Committee on Psychosocial Aspects of Child and Family Health; Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 2001;108:793-7. [PubMed]
- Abu-Saad HH, Hamers JP. Decision-making and pediatric pain: a review. J Adv Nurs 1997;26:946-52. [Crossref] [PubMed]
- Srouji R, Ratnapalan S, Schneeweiss S. Pain in Children: Assessment and Nonpharmacological Management. Int J Pediatr 2010;2010. pii: 474838.
- Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs 1988;14:9-17. [PubMed]
- WPCA Policy statement on defining palliative care. Available online: www.thewpca.org/EasySiteWeb/GatewayLink.aspx?alId=85177
- Du Pen SL, Du Pen AR, Pollisar N, et al. Implementing guidelines for cancer pain management: results of a randomized controlled clinical trial. J Clin Oncol 1999;17:361-70. [PubMed]
- Sloan PA. The evolving role of interventional pain management in oncology. J Support Oncol 2004;2:491-500. [PubMed]
- Zuurmond WW, Perez RS, Loer SA. New aspects in performing interventional techniques for chronic pain. Curr Opin Support Palliat Care 2007;1:132-6. [Crossref] [PubMed]
- Jadad AR, Browman GP. The WHO analgesic ladder for cancer pain management. Stepping up the quality of its evaluation. JAMA 1995;274:1870-3. [Crossref] [PubMed]
- Birthi P, Sloan P. Interventional treatment of refractory cancer pain. Cancer J 2013;19:390-6. [Crossref] [PubMed]
- Miguel R. Interventional treatment of cancer pain: the fourth step in theworld health organization analgesic ladder? Cancer Control 2000;7:149-56. [PubMed]
- Jain PN, Shrikhande SV, Myatra SN, et al. Neurolytic celiac plexus block: a better alternative to opioid treatment in upper abdominal malignancies: an Indian experience. J Pain Palliat Care Pharmacother 2005;19:15-20. [PubMed]
- Loukas M, Klaassen Z, Merbs W, et al. A review of the thoracic splanchnic nerves and celiac ganglia. Clin Anat 2010;23:512-22. [Crossref] [PubMed]
- Polati E, Luzzani A, Schweiger V, et al. The role of neurolytic celiac plexus block in the treatment of pancreatic cancer pain. Transplant Proc 2008;40:1200-4. [Crossref] [PubMed]
- Marra V, Debernardi F, Frigerio A, et al. Neurolytic block of the celiac plexus and splanchnic nerves with computed tomography: the experience in 150 cases and an optimization of the technic. Radiol Med 1999;98:183-8. [PubMed]
- Levy MJ, Chari ST, Wiersema MJ. Endoscopic ultrasound-guided celiac neurolysis. Gastrointest Endosc Clin N Am 2012;22:231-47. [Crossref] [PubMed]
- Bosscher H. Blockade of the superior hypogastric plexus block for visceral pelvic pain. Pain Pract 2001;1:162-70. [Crossref] [PubMed]
- Mohamed SA, Ahmed DG, Mohamad MF. Chemical neurolysis of the inferior hypogastric plexus for the treatment of cancer-related pelvic and perineal pain. Pain Res Manag 2013;18:249-52. [Crossref] [PubMed]
- Khosla A, Adeyefa O, Nasir S. Successful treatment of radiation-induced proctitis pain by blockade of the ganglion impar in an elderly patient with prostate cancer: a case report. Pain Med 2013;14:662-6. [Crossref] [PubMed]
- Smith TJ, Staats PS, Deer T, et al. Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol 2002;20:4040-49. [Crossref] [PubMed]
- World Health Organization. Essential medicines-WHO model list. 15th ed. Geneva. Switzerland: World Health Organization; 2007. Available online: www.who.int/medicines/publications/08_ENGLISH_indexFINAL_EML15.pdf
- World Health Organization. Essential medicines (Website). Geneva. Switzerland: 2005. Available online: http://www.who.int/topics/essential_medicines/en/
- De Lima L, Krakauer EL, Lorenz KA, et al. Ensuring palliative medicine availability: The development of IAHPC list of essential medicines for palliative care. J. Pain Symptom. Manage 2007;33:521-26. [Crossref] [PubMed]
- Mani RK, Amin P, Chawla R, et al. Limiting life-prolonging interventions and providing palliative care towards the end-of- life in Indian intensive care units. Indian J Crit Care Med 2005;9:96-107. [Crossref]
- Macaden SC. Moving toward a national policy on palliative and end of life care. Indian J Palliat Care 2011;17:S42-4. [Crossref] [PubMed]