Solitary brain metastasis from prostate cancer: a case report
Introduction
Prostate cancer commonly metastasizes to the pelvic lymph nodes, axial skeleton, and lungs (1,2). Brain metastases from prostate cancer are rare and are usually discovered post-mortem. These metastases typically only occur in the context of widespread metastatic disease. It is even more uncommon to have the brain as the sole site of metastatic prostate cancer. We present the case of a 67-year-old male who presented with recurrence of prostate cancer with a solitary brain metastasis, treated with tumor resection and adjuvant stereotactic radiation treatment (RT) to the surgical bed.
Case presentation
A 67-year-old male was initially diagnosed with prostate cancer in 2008, presenting with a prostate specific antigen (PSA) of 53.13 ng/dL. Clinical exam and biopsy revealed a Gleason 8 (4+4), T3a prostate cancer. Staging with CT scans and bone scan did not show any evidence of systemic disease.
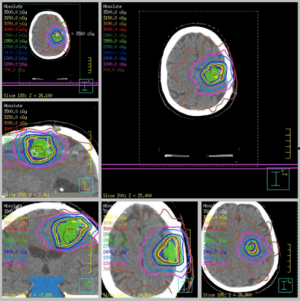
The patient received RT in a two phase plan to his pelvic lymph nodes and prostate. The pelvis received a dose of 46 Gy in 23 fractions in phase 1, and a total dose of 76 Gy in 38 fractions by the end of phase 2. Androgen deprivation therapy (ADT) was subsequently initiated for a period of three years. Approximately one year after initiation of ADT, his PSA was undetectable. The patient remained on ADT until 2012, and showed no evidence of recurrence until 2014, when he presented with symptoms of dizziness, mild dysphagia and imbalance. Following a suspicious fall in his urologist’s office, he was referred to the Emergency Department where an MRI of his brain showed a heterogeneous, multi-lobulated intra-axial lesion in the left frontal lobe with rim enhancement and surrounding edema (Figure 1). He was referred to a neurosurgeon and had repeat staging which showed no evidence of extra-cranial disease. His PSA two years following termination of ADT rose from an undetectable <0.2 to 3.7 ng/dL.
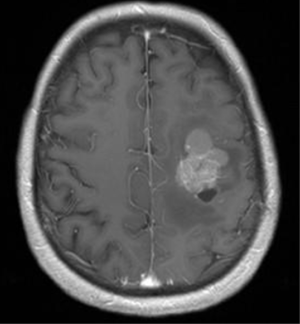
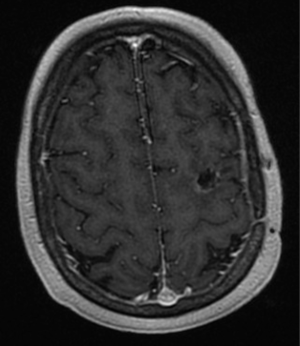
A left temporal craniotomy and gross total resection of the tumor was performed. The final pathologic diagnosis confirmed prostate cancer, staining positive for PSA. The patient experienced a complication-free postoperative recovery with no neurological deficits. Tumor resection was followed by stereotactic radiation therapy to the surgical cavity with a dose of 30 Gy in 5 fractions (Figure 2). ADT was subsequently re-initiated, resulting in the patient’s PSA returning to an undetectable level and remaining undetectable with no evidence of disease 17 months post-radiotherapy. Follow-up MRI imaging of his head confirmed no residual or recurrent disease (Figure 3).
Discussion
The ante-mortem diagnosis of a solitary metastasis to the brain from prostate cancer is exceedingly rare; our review of the literature identified 16 previously-reported cases in the literature over the past 25 years (3-13) (Table 1). Survival in these cases generally mostly ranged between 2 to 20 months, with some patients still alive at the time of reporting. In one case, a patient presenting with a right cerebellar infarct following transurethral resection of the prostate three months earlier was reported to remain alive and symptom-free 5 years post-operatively following sub-occipital craniotomy with excision of the mass, which was noted to be moderately differentiated adenocarcinoma, and whole brain radiation therapy (WBRT) and radiotherapy to the posterior fossa (4). In another case, a patient with pathologic Gleason 9 (4+5) prostate adenocarcinoma was reported to remain alive 5 years post-treatment without signs of recurring disease (11).

Full table
For decades, surgical resection with adjuvant WBRT has been the standard of care for solitary metastases in the brain. This combined therapy strategy has been evaluated in randomized studies and found to significantly reduce the risk of recurrence when compared with surgical resection or WBRT alone (14-17). These studies, however, did not include any patients with prostate cancer brain metastases patients. Due to concerns of WBRT-related neurotoxicity and the risk of neurocognitive side effects, the application of high dose radiation to the postoperative surgical bed through stereotactic radiosurgery has been increasing in clinical practice (18). Stereotactic radiosurgery alone following surgical resection of a brain metastasis has the potential to limit long-term neurocognitive side effects and improve local control as compared to WBRT (19,20).
The risk of distant brain recurrence in patients with brain metastases from prostate cancer is unknown. The potential for WBRT to decrease distant brain recurrence as compared to cavity stereotactic radiosurgery is, therefore, also unknown. In this case, given that there was only one site of disease, it was felt to be reasonable to forego WBRT and monitor with brain imaging on a three-month basis. The approach has appeared effective thus far, with no evidence of new or recurrent disease in the brain at the time of report.
Conclusions
Metastatic disease exclusive to the brain in prostate cancer patients remains extremely infrequent. This unique case of a 67-year-old male with a solitary brain metastasis arising from prostate cancer demonstrates that aggressive treatment with tumor resection and adjuvant stereotactic RT to the surgical bed without WBRT may be optimal in the management of such patients.
Acknowledgements
This work was supported by the Bratty Family Fund; Michael and Karyn Goldstein Cancer Research Fund; Joey and Mary Furfari Cancer Research Fund; Pulenzas Cancer Research Fund; Joseph and Silvana Melara Cancer Research Fund; and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Bubendorf L, Schopfer A, Wagner U, et al. Metastatic patterns of prostate cancer: an autopsy study of 1,589 patients. Hum Pathol 2000;31:578-83. [Crossref] [PubMed]
- Hess KR, Varadhachary GR, Taylor SH, et al. Metastatic patterns in adenocarcinoma. Cancer 2006;106:1624-33. [Crossref] [PubMed]
- Rao KG. Carcinoma of prostate presenting as intracranial tumor with multiple cranial nerve palsies. Urology 1982;19:433-5. [Crossref] [PubMed]
- Lynes WL, Bostwick DG, Freiha FS, et al. Parenchymal brain metastases from adenocarcinoma of prostate. Urology 1986;28:280-7. [Crossref] [PubMed]
- Kasabian NG, Previte SR, Kaloustian HD, et al. Adenocarcinoma of the prostate presenting initially as an intracerebral tumor. Cancer 1992;70:2149-51. [Crossref] [PubMed]
- Kunkler RB, Cooksey G, Millac P. Carcinoma of the prostate presenting with a cerebral metastasis. Br J Urol 1993;71:103-4. [Crossref] [PubMed]
- Gupta A, Baidas S, Cumberlin RK. Brain stem metastasis as the only site of spread in prostate carcinoma. A case report. Cancer 1994;74:2516-9. [Crossref] [PubMed]
- Sutton MA, Watkins HL, Green LK, et al. Intracranial metastases as the first manifestation of prostate cancer. Urology 1996;48:789-93. [Crossref] [PubMed]
- McCutcheon IE, Eng DY, Logothetis CJ. Brain metastasis from prostate carcinoma: antemortem recognition and outcome after treatment. Cancer 1999;86:2301-11. [Crossref] [PubMed]
- Salvati M, Frati A, Russo N, et al. Brain metastasis from prostate cancer: report of 13 cases and critical analysis of the literature. J Exp Clin Cancer Res 2005;24:203-7. [PubMed]
- Sweets T, Bracken RB, Geisler EJ, et al. Intracranial treatment for solitary prostatic adenocarcinoma brain metastasis is curative. Urology 2009;73:681.e7-9. [Crossref] [PubMed]
- Mithal P, Gong Y, Sirkis H, et al. A brain lesion as the sole metastasis of prostate cancer. J Clin Urol 2014. [Crossref]
- Craig J, Woulfe J, Sinclair J, et al. Isolated brain metastases as first site of recurrence in prostate cancer: case report and review of the literature. Curr Oncol 2015;22:e493-7. [Crossref] [PubMed]
- Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 1990;322:494-500. [Crossref] [PubMed]
- Noordijk EM, Vecht CJ, Haaxma-Reiche H, et al. The choice of treatment of single brain metastasis should be based on extracranial tumor activity and age. Int J Radiat Oncol Biol Phys 1994;29:711-7. [Crossref] [PubMed]
- Kocher M, Soffietti R, Abacioglu U, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 2011;29:134-41. [Crossref] [PubMed]
- Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain. JAMA 1998;280:1485-9. [Crossref] [PubMed]
- Roberge D, Petrecca K, El Refae M, et al. Whole-brain radiotherapy and tumor bed radiosurgery following resection of solitary brain metastases. J Neurooncol 2009;95:95-9. [Crossref] [PubMed]
- Muacevic A, Kreth FW, Horstmann GA, et al. Surgery and radiotherapy compared with gamma knife radiosurgery in the treatment of solitary cerebral metastases of small diameter. J Neurosurg 1999;91:35-43. [Crossref] [PubMed]
- Loeffler JS, Kooy HM, Wen PY, et al. The treatment of recurrent brain metastases with stereotactic radiosurgery. J Clin Oncol 1990;8:576-82. [PubMed]